Table of Contents
ToggleARTERIOSCLEROSIS & ATHEROSCLEROSIS
ARTERIOSCLEROSIS
Introduction
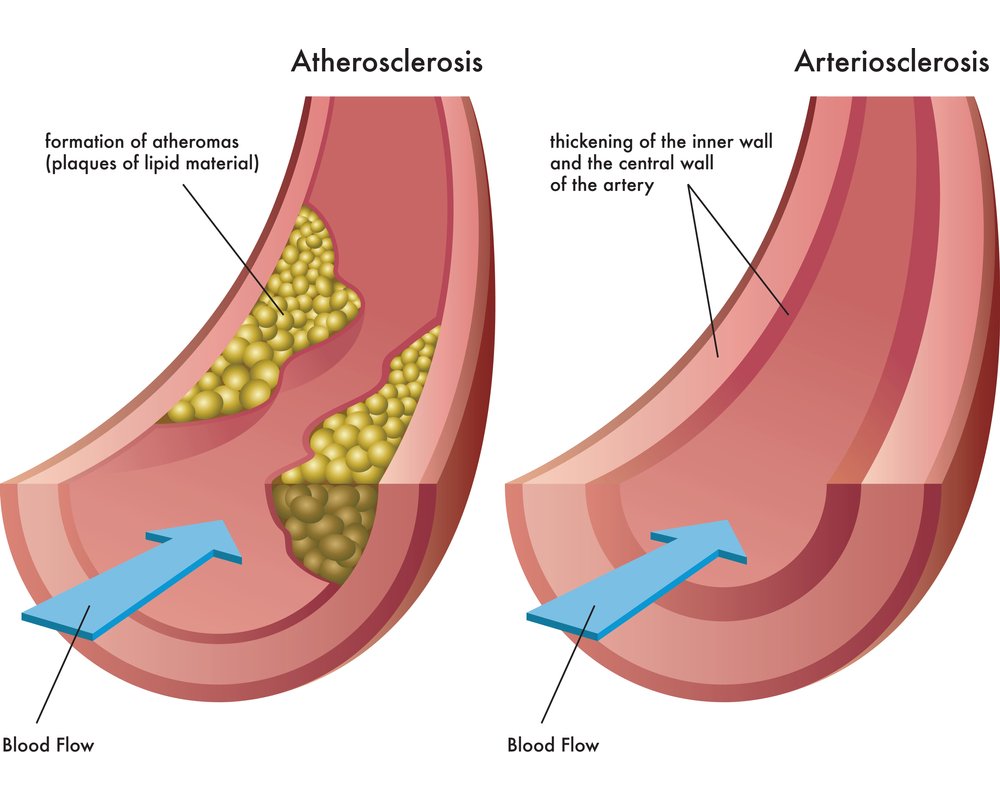
Arteriosclerosis is the thickening, hardening, and loss of elasticity of the walls of arteries. Arteriosclerosis is the most common disease of the arteries; the term means hardening of the arteries. It is a diffuse process whereby the muscle fibers and the endothelial lining of the walls of small arteries and arterioles become thickened. This process gradually restricts the blood flow to one's organs and tissues and can lead to severe health risks brought on by atherosclerosis, which is a specific form of arteriosclerosis caused by the buildup of fatty plaques, cholesterol, and some other substances in and on the artery walls.
Pathophysiology
The lesions of arteriosclerosis begin as the intima (innermost layer of blood vessel wall) of the arterial wall start to fill up with the deposition of cellular wastes. As these start to mature, they can take different forms of arteriosclerosis. All are linked through common features such as the stiffening of arterial vessels, thickening of arterial walls and degenerative nature of the disease. Arteriolosclerosis, unlike atherosclerosis, is a sclerosis that only affects small arteries and arterioles, which carry nutrients and blood to the cells.
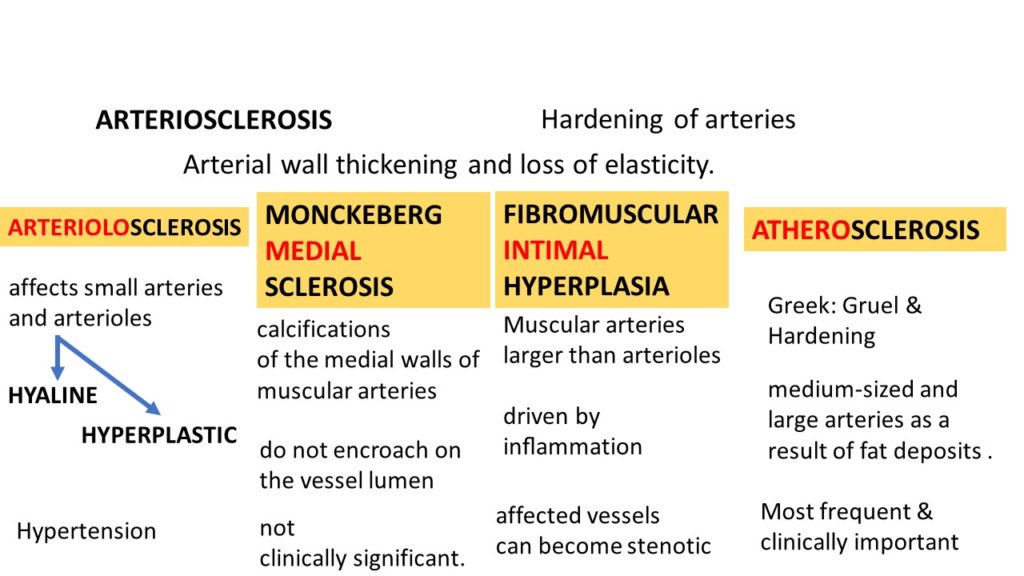
Types of Arteriosclerosis
- Monckeberg's arteriosclerosis or medial calcific sclerosis is seen mostly in the elderly, commonly in arteries of the extremities. This involves calcification of the media of muscular arteries, without obstruction of the vessel lumen.
- Hyperplastic: Hyperplastic arteriosclerosis refers to the type of arteriosclerosis that affects small arteries and arterioles, characterized by concentric thickening of the vessel walls (often described as "onion-skinning") due to smooth muscle cell proliferation, commonly seen in severe hypertension.
- Hyaline type: Hyaline arteriosclerosis, also referred to as arterial hyalinosis and arteriolar hyalinosis, refers to lesions that are caused by the deposition of homogenous hyaline (a proteinaceous material) in the small arteries and arterioles, leading to luminal narrowing. This is often associated with benign hypertension and diabetes mellitus.
ATHEROSCLEROSIS
Introduction
Definition: Atherosclerosis is the buildup of fatty material called plaque or atheroma, in the lining of the artery walls. It is a specific type of arteriosclerosis.
This buildup causes the narrowing of the affected arteries. When the arteries are narrowed, blood cannot go through it easily. This can lead to reduced delivery of oxygen and nutrients to the cells of the body.
Causes of Atherosclerosis
The exact cause of atherosclerosis isn’t known. However, studies show that atherosclerosis is a slow, complex disease that may start in childhood. It develops faster as you age. Atherosclerosis may start when certain factors damage the inner layers of the arteries.
- Hypercholesterolemia (especially high levels of low-density lipoprotein (LDL)-cholesterol, often referred to as "bad" cholesterol)
- Hypertension (High Blood Pressure)
- Diabetes mellitus (High blood sugar levels can damage blood vessels over time)
- Cigarette smoking (Damages the inner lining of blood vessels, promotes inflammation, and alters lipid profiles)
- Age (Male older than 45 years and female older than 55 years; risk increases with age due to cumulative exposure to risk factors and natural aging processes)
- Male gender (Men tend to develop atherosclerosis earlier than women, though risk for women increases after menopause)
- Strong family history of early heart disease (suggests a genetic predisposition)
- Also, a sedentary lifestyle (lack of physical activity contributes to obesity, hypertension, diabetes, and dyslipidemia)
- Obesity (especially abdominal obesity, linked to metabolic syndrome and increased cardiovascular risk)
- Diets high in saturated and trans-fatty acids, and certain genetic mutations contribute to risk.
- While a low level of high-density lipoprotein (HDL)-cholesterol is considered a risk factor (HDL helps remove cholesterol from arteries, so low levels are detrimental)
- High levels of C-reactive protein (CRP), a marker of inflammation (indicates systemic inflammation, which plays a role in atherosclerosis development)
- Sleep apnea (can contribute to hypertension and other cardiovascular risks)
- Chronic kidney disease
- Inflammatory diseases (e.g., lupus, rheumatoid arthritis)
Pathophysiology of Atherosclerosis
Atherosclerosis is a chronic inflammatory response in the walls of arteries, primarily driven by endothelial dysfunction and lipid accumulation. The process typically unfolds over decades:
- Endothelial Damage/Dysfunction: The process begins with injury or dysfunction to the endothelium (the innermost lining of the artery). This damage can be caused by risk factors like hypertension, high cholesterol, smoking, and diabetes. Damaged endothelium becomes more permeable and allows LDL cholesterol to enter the arterial wall.
- Lipid Accumulation and Oxidation: LDL particles penetrate the intimal layer of the artery and become trapped. Within the arterial wall, these LDL particles undergo oxidation. Oxidized LDL is highly inflammatory and toxic.
- Immune Response and Foam Cell Formation: The oxidized LDL triggers an inflammatory response. Monocytes (a type of white blood cell) are recruited to the site, adhere to the dysfunctional endothelium, and migrate into the intima. Once in the intima, monocytes transform into macrophages. These macrophages engulf large amounts of oxidized LDL, becoming lipid-laden "foam cells."
- Fatty Streak Formation: An accumulation of foam cells forms visible yellowish lesions called "fatty streaks" on the arterial wall. These are the earliest macroscopic lesions of atherosclerosis and can be seen even in childhood.
- Smooth Muscle Cell Migration and Proliferation: In response to growth factors and cytokines released during the inflammatory process, smooth muscle cells (SMCs) from the media (middle layer of the artery) migrate into the intima. These SMCs proliferate and produce extracellular matrix components (collagen, elastin, proteoglycans), which contribute to the bulk of the plaque.
- Fibrous Plaque Formation: The proliferating SMCs, extracellular matrix, lipids (both intracellular and extracellular), and inflammatory cells form a "fibrous plaque." This plaque has a lipid-rich core (necrotic core) surrounded by a fibrous cap composed of SMCs and collagen.
- Plaque Progression and Complications:
- Growth: Plaques grow over time, gradually narrowing the artery lumen and impeding blood flow. This can lead to symptoms of ischemia (e.g., angina, claudication).
- Calcification: Over time, plaques often calcify, becoming harder and more rigid.
- Rupture/Erosion: The fibrous cap can thin and become unstable, making it prone to rupture or erosion. When a plaque ruptures, the highly thrombogenic (clot-forming) contents of the lipid core are exposed to the blood.
- Thrombosis: Exposure of the plaque contents triggers immediate platelet aggregation and activation of the coagulation cascade, leading to the formation of a thrombus (blood clot) on top of the ruptured plaque.
- Acute Events: A thrombus can completely occlude the artery, leading to acute ischemic events like myocardial infarction (heart attack) or ischemic stroke. Even if it doesn't fully occlude, it can further narrow the artery or detach and travel downstream (embolism).
Clinical manifestations
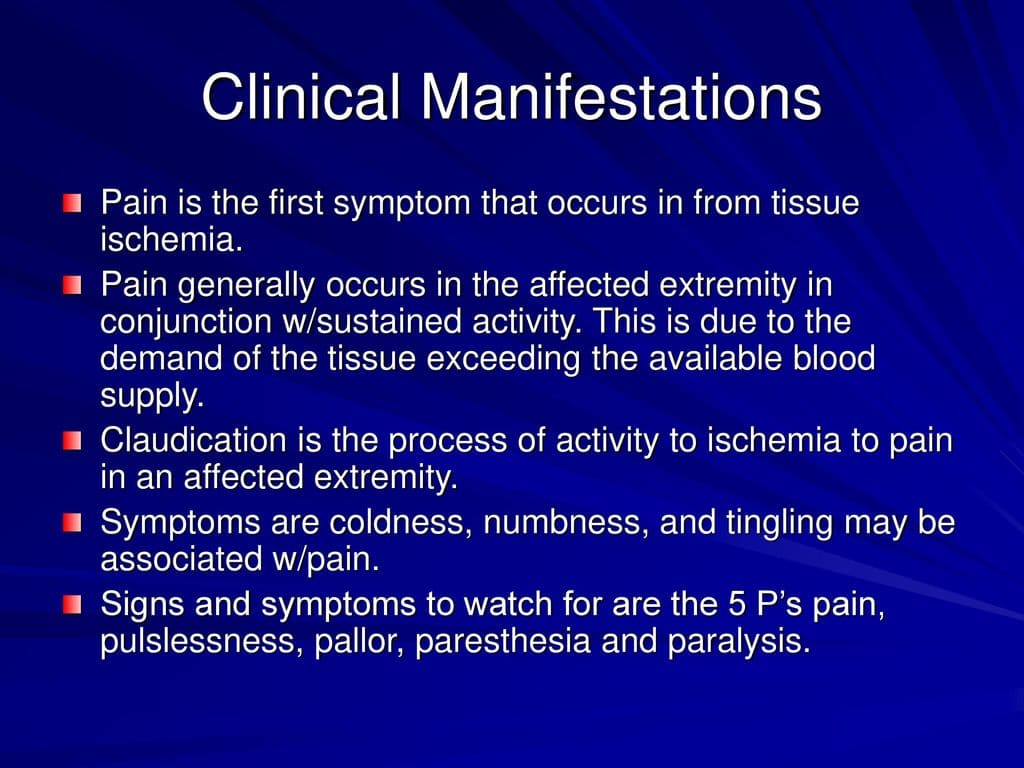
Signs and symptoms will depend on which arteries are affected, and often only appear when an artery is significantly narrowed or blocked, or when an acute event (like plaque rupture) occurs.
Coronary Arteries (Leading to Coronary Artery Disease - CAD)
When atherosclerosis affects the arteries supplying blood to the heart, it leads to CAD, which can manifest as:
- Angina Pectoris: Chest pain or discomfort, often described as pressure, squeezing, fullness, or pain, typically triggered by exertion or stress and relieved by rest or nitroglycerin. This is due to insufficient blood flow to the heart muscle (ischemia).
- Shortness of Breath (Dyspnea): Especially with exertion, due to the heart's inability to pump enough blood efficiently.
- Tachycardia: Rapid heart rate, as the heart tries to compensate for reduced blood flow.
- Palpitations: Awareness of irregular or forceful heartbeats.
- Fatigue and Weakness: Due to reduced oxygen supply to the body.
- Myocardial Infarction (Heart Attack): Occurs when blood flow to a part of the heart is completely blocked, usually by a blood clot forming on a ruptured plaque, leading to heart muscle death. Symptoms include severe chest pain (often radiating to arm, back, neck, jaw, or stomach), shortness of breath, cold sweat, nausea, lightheadedness.
- Arrhythmias: Irregular heart rhythms.
Carotid Arteries (Leading to Carotid Artery Disease)
The carotid arteries supply oxygen-rich blood to the brain. If plaque narrows or blocks these arteries, one may have symptoms of a transient ischemic attack (TIA) or stroke. These symptoms may include:
- Sudden weakness, numbness, or paralysis of the face, arm, or leg, especially on one side of the body.
- Confusion or trouble understanding speech.
- Trouble speaking (aphasia) or slurred speech (dysarthria).
- Trouble seeing in one or both eyes (amaurosis fugax, often described as a curtain coming down over vision).
- Difficulty in swallowing (dysphagia).
- Dizziness, trouble walking, loss of balance or coordination, and unexplained falls.
- Loss of consciousness.
- Sudden and severe headache with no known cause.
Peripheral Arteries (Leading to Peripheral Artery Disease - PAD)
Plaque also can build up in the major arteries that supply oxygen-rich blood to the legs, arms, and pelvis. If these major arteries are narrowed or blocked, you may have:
- Intermittent Claudication: Pain, cramping, aching, or fatigue in the legs, calves, buttocks, or thighs during exercise (like walking) that disappears with rest. This is the hallmark symptom.
- Numbness or weakness in the legs or feet.
- Coldness in the lower leg or foot, especially compared with the other side.
- Sores on the toes, feet, or legs that heal slowly or not at all.
- A change in the color of the legs (pallor or bluish discoloration).
- Hair loss or slower hair growth on the legs and feet.
- Slower growth of toenails.
- Shiny skin on the legs.
- No or a weak pulse in the legs or feet.
- Erectile dysfunction in men.
- In severe cases, rest pain (pain in the feet or toes even at rest) and critical limb ischemia (leading to gangrene and potential amputation).
Renal Arteries (Leading to Renal Artery Stenosis)
The renal arteries supply oxygen-rich blood to the kidneys. If plaque builds up in these arteries, one may develop renal artery stenosis, which can lead to:
- Difficult-to-control high blood pressure (hypertension), especially if it develops suddenly or worsens rapidly.
- Worsening kidney function, particularly when taking certain medications for blood pressure.
- Fluid retention and generalized swelling.
- Early kidney disease often has no signs or symptoms. As the disease gets worse, it can cause tiredness, changes in how you urinate (more often or less often), loss of appetite, nausea (feeling sick to the stomach), swelling in the hands or feet, itchiness or numbness and trouble concentrating.
- Abdominal bruits (whooshing sounds heard with a stethoscope over the affected kidney artery).
Mesenteric Arteries (Leading to Chronic Mesenteric Ischemia)
Atherosclerosis in the arteries supplying the intestines can cause:
- Severe abdominal pain after eating (often called "abdominal angina"), as digestion requires increased blood flow.
- Weight loss due to fear of eating.
- Nausea, vomiting, diarrhea.
Diagnosis of Atherosclerosis
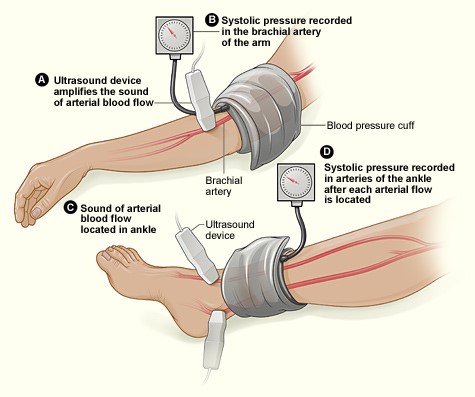
Diagnosis of atherosclerosis involves a combination of medical history, physical examination, and various diagnostic tests:
- Lipid Panel: Measures total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides.
- Blood Glucose/HbA1c: To check for diabetes.
- High-sensitivity C-reactive protein (hs-CRP): A marker of inflammation that can indicate increased risk.
- Kidney and Liver Function Tests: To assess organ health.
- CT Angiography (CTA): Uses X-rays and contrast dye to create detailed images of blood vessels.
- MR Angiography (MRA): Uses magnetic fields and radio waves to create images of blood vessels, often without contrast or with a different type of contrast.
- Conventional Angiography (Catheter Angiography): An invasive procedure where a catheter is inserted into an artery and guided to the area of interest, then contrast dye is injected to visualize the arteries on X-ray. Considered the gold standard for detailed arterial imaging.
Medical Management / Treatment for Atherosclerosis
Treatment for atherosclerosis focuses on slowing or reversing plaque buildup, managing symptoms, and preventing complications. It often involves a combination of lifestyle modifications, medications, and sometimes medical procedures.
A. Lifestyle Modifications (Cornerstone of Management):
- Consume a diet rich in fruits, vegetables, whole grains, lean proteins (fish, poultry, legumes), and healthy fats (monounsaturated and polyunsaturated).
- Limit saturated and trans fats, cholesterol, sodium, and added sugars.
- Examples: Mediterranean diet, DASH diet.
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week.
- Helps control weight, lower blood pressure, improve cholesterol levels, and manage diabetes.
B. Medications:
- Statins (e.g., atorvastatin, simvastatin): First-line therapy, highly effective at lowering LDL-cholesterol, stabilizing plaques, and reducing cardiovascular events.
- Ezetimibe: Reduces cholesterol absorption in the intestine.
- PCSK9 inhibitors (e.g., alirocumab, evolocumab): Powerful LDL-lowering drugs, typically used for patients with very high cholesterol or those intolerant to statins.
- Other agents: Fibrates, Niacin (less commonly used due to side effects or less robust outcome data).
- Aspirin: Often prescribed to prevent blood clots in patients with established cardiovascular disease or high risk.
- P2Y12 inhibitors (e.g., clopidogrel, ticagrelor): Stronger antiplatelets, used in patients with recent heart attack, stroke, or after stent placement.
- ACE Inhibitors (e.g., lisinopril, enalapril) or Angiotensin Receptor Blockers (ARBs) (e.g., valsartan, losartan): Protect the heart and kidneys, especially important in patients with diabetes or kidney disease.
- Beta-Blockers (e.g., metoprolol, carvedilol): Lower heart rate and blood pressure, reduce oxygen demand of the heart, often used after heart attack or in heart failure.
- Calcium Channel Blockers (e.g., amlodipine, diltiazem): Relax blood vessels, lower blood pressure.
- Diuretics (e.g., hydrochlorothiazide, furosemide): Help the body eliminate excess fluid and sodium, lowering blood pressure.
C. Medical Procedures and Surgeries:
These are typically reserved for cases where atherosclerosis is causing significant symptoms, severely narrowing arteries, or posing an immediate threat.
- A catheter with a balloon is inserted into the narrowed artery and inflated to widen it.
- A stent (a small mesh tube) is often placed to keep the artery open. Commonly used in coronary arteries (Percutaneous Coronary Intervention - PCI), carotid arteries, and peripheral arteries.
- Coronary Artery Bypass Grafting (CABG): For severe blockages in coronary arteries.
- Peripheral Bypass Surgery: For blockages in leg arteries.
Medical and Surgical Management
Medical Management
- Blood thinning agents such as Aspirin – to reduce the ability of the blood to clot, so that the blood flows easier through the narrowed arteries.
- Nitrates – to relax the blood vessels.
- Beta blockers – to decrease the cardiac demand for oxygen by means of lowering the heart rate and blood pressure levels
- Calcium channel blockers – used in combination with beta blockers
- Diuretics to reduce blood pressure
- Ranolazine – to treat angina
Surgical Management
- Surgery. Surgical interventions are required if the medical team believes that an urgent, more aggressive treatment for the complications of atherosclerosis (such as CAD and PVD) is needed. These surgeries include:
- Coronary artery bypass surgery – creation of a graft to reroute the blood flow away from the diseased artery
- Fibrinolytic therapy – usage of a clot-dissolving drug to dissolve the atheroma
- Endarterectomy – surgical removal of atheroma from the narrowed arteries
- Angioplasty and stent placement: A catheter is first inserted into the blocked or narrowed part of the artery, followed by a second one with a deflated balloon that is passed through the catheter into the narrowed area. The balloon is then inflated, pushing the deposits back against the arterial walls, and then a mesh tube is usually left behind to prevent the artery from retightening.
Lifestyle Changes
A low cholesterol, low sugar diet to control cholesterol and blood glucose levels is needed for a patient with atherosclerosis. Foods rich in omega-3 fatty acids such as fish, soybeans, and flaxseeds are recommended. Smoking is another risk factor of atherosclerosis and CAD. Increased physical activity by doing at least 150 minutes of moderate aerobic exercises will help promote an active lifestyle.
NURSING DIAGNOSES FOR ARTERIOSCLEROSIS AND ATHEROSCLEROSIS
Nursing diagnoses provide a framework for nursing care, identifying patient problems that nurses can independently address. For patients with arteriosclerosis and atherosclerosis, common nursing diagnoses include:
- Ineffective Peripheral Tissue Perfusion related to decreased arterial blood flow secondary to narrowed or occluded vessels.
- Defining Characteristics: Diminished or absent pulses, prolonged capillary refill, pallor on elevation, rubor on dependency, cool extremities, pain (claudication or rest pain), non-healing wounds, trophic changes (hair loss, brittle nails, shiny skin).
- Acute Pain / Chronic Pain related to myocardial ischemia (angina), peripheral ischemia (claudication), or cerebral ischemia.
- Defining Characteristics: Verbalization of pain (chest, leg, abdominal, headache), guarding behavior, restlessness, changes in vital signs (tachycardia, hypertension during acute pain episodes), facial mask of pain.
- Activity Intolerance related to imbalance between oxygen supply and demand secondary to myocardial or peripheral ischemia.
- Defining Characteristics: Dyspnea on exertion, chest pain with activity, leg pain with activity (claudication), weakness, fatigue, abnormal heart rate or blood pressure response to activity.
- Risk for Decreased Cardiac Output related to myocardial ischemia, left ventricular dysfunction, or arrhythmias.
- Defining Characteristics (if actual): Tachycardia, dysrhythmias, decreased blood pressure, decreased peripheral pulses, crackles in lungs, S3 or S4 heart sounds, decreased urine output, altered mental status. (Note: "Risk for" implies potential, not actual, signs).
- Risk for Impaired Cerebral Tissue Perfusion related to interrupted blood flow secondary to carotid artery stenosis or emboli.
- Defining Characteristics (if actual): Changes in mental status, neurological deficits (weakness, paralysis, aphasia, visual disturbances), dizziness, headache.
- Risk for Imbalanced Nutrition: More Than Body Requirements related to excessive intake of saturated fats, cholesterol, and calories, or sedentary lifestyle.
- Defining Characteristics: BMI > 25, observed excessive food intake, sedentary activity level.
- Deficient Knowledge regarding disease process, risk factors, medications, diet, and lifestyle modifications.
- Defining Characteristics: Verbalization of misconceptions, inaccurate follow-through of instructions, recurrence of preventable complications.
- Anxiety related to chest pain, fear of death, threat to health status, or perceived change in health status.
- Defining Characteristics: Verbalization of anxiety, restlessness, apprehension, increased heart rate, shortness of breath.
- Ineffective Health Management related to complexity of therapeutic regimen, perceived barriers, or insufficient social support.
- Defining Characteristics: Failure to take medications as prescribed, failure to follow diet/exercise recommendations, frequent exacerbations of chronic disease.
Nursing Interventions for Arteriosclerosis and Atherosclerosis
Nursing interventions are actions taken by nurses to achieve patient outcomes based on nursing diagnoses. These interventions aim to alleviate symptoms, prevent complications, and promote patient well-being.
- Assess the patient’s vital signs and characteristics of heart beat (rate, rhythm, strength) at least every 4 hours, and more frequently if unstable or during acute episodes. Auscultate heart sounds for murmurs, gallops (S3, S4), and rubs. Observe for signs of decreasing peripheral tissue perfusion such as slow capillary refill, facial pallor, cyanosis (especially lips, nail beds), and cool, clammy skin. Document findings and report significant changes to the physician.
- Administer prescribed medications for atherosclerosis (e.g., antiplatelets, statins, antihypertensives, nitrates) as ordered, noting patient response and any adverse effects. Educate the patient about the purpose, dosage, frequency, and potential side effects of each medication. Emphasize adherence to the medication regimen.
- Administer supplemental oxygen, as prescribed, especially during episodes of chest pain or dyspnea, to improve myocardial oxygen supply and reduce demand. Monitor oxygen saturation (SpO2) closely. Discontinue if SpO2 level is above the target range (usually >92-94%), or as ordered by the physician, to prevent oxygen toxicity or hyperoxia.
- Educate patient on stress management techniques, deep breathing exercises, and relaxation techniques (e.g., guided imagery, progressive muscle relaxation) to help reduce sympathetic nervous system activation, which can exacerbate cardiovascular symptoms. Encourage participation in stress-reducing activities.
- Administer prescribed medications that alleviate the symptoms of pain (e.g., nitroglycerin for chest pain, analgesics for leg/limb pain) promptly. Assess the patient’s vital signs and characteristics of pain (location, intensity using a pain scale, quality, duration, precipitating and relieving factors) at least 30 minutes after administration of medication to evaluate effectiveness and identify need for further intervention.
- Elevate the head of the bed (semi-Fowler's or high-Fowler's position) if the patient is short of breath, to facilitate lung expansion and ease breathing. Administer supplemental oxygen, as prescribed, and monitor respiratory status (rate, depth, effort, breath sounds).
- Place the patient in complete bed rest when in severe pain (e.g., unstable angina, acute myocardial infarction) to decrease myocardial oxygen demand. Ensure a calm and quiet environment. Assist with all activities of daily living (ADLs).
- Promote gradual increase in activity as tolerated and indicated, following physician orders or cardiac rehabilitation guidelines. Monitor patient's response to activity (vital signs, SpO2, pain, dyspnea). Teach patient signs of activity intolerance to report.
- Monitor fluid balance (intake and output, daily weights, assess for edema) especially in patients with heart failure or renal involvement, to prevent fluid overload or dehydration. Administer diuretics as prescribed and monitor electrolyte levels.
- Implement a heart-healthy and low-sodium diet in collaboration with a dietitian. Educate the patient and family about dietary restrictions and food choices (e.g., lean proteins, whole grains, fruits, vegetables, low-fat dairy, limited processed foods, saturated/trans fats, and cholesterol).
- Encourage smoking cessation. Provide resources and support (e.g., nicotine replacement therapy, counseling, support groups). Educate on the detrimental effects of smoking on cardiovascular health.
- Promote regular exercise as appropriate for the patient's condition and tolerance. Refer to cardiac rehabilitation programs or provide guidance on safe exercise routines.
- Monitor blood glucose levels closely in diabetic patients and ensure adherence to antidiabetic medications and dietary recommendations to prevent micro- and macrovascular complications.
- Assess skin integrity regularly, especially on the extremities, for signs of impaired perfusion such as non-healing wounds, ulcers, or changes in skin color/temperature. Provide meticulous wound care if present.
- Educate patient and family about the disease process, risk factors, early signs and symptoms of complications (e.g., chest pain, stroke symptoms, worsening claudication), and when to seek emergency medical attention. Encourage active participation in self-management.
- Provide emotional support and address anxiety. Listen to patient concerns, provide clear explanations, and involve family in care. Refer to social work or counseling if needed.
- Prevent complications of immobility (e.g., deep vein thrombosis, pressure ulcers) through appropriate interventions such as repositioning, leg exercises, and ensuring adequate hydration and nutrition.
Complications of Atherosclerosis
The complications of atherosclerosis are varied and often severe, depending on which arteries are affected. They arise from the narrowing of blood vessels (ischemia) or the rupture of plaques leading to clot formation (thrombosis/embolism).
- Coronary Artery Disease (CAD):
- Angina (stable or unstable)
- Myocardial Infarction (Heart Attack)
- Heart Failure (due to chronic ischemia or damage from MIs)
- Arrhythmias (e.g., sudden cardiac death)
- Cerebrovascular Disease (leading to Stroke or TIA):
- Transient Ischemic Attack (TIA - "mini-stroke")
- Ischemic Stroke (due to blockages in brain arteries or emboli from carotid plaques)
- Vascular Dementia (due to chronic reduced blood flow to the brain)
- Peripheral Artery Disease (PAD):
- Intermittent claudication
- Non-healing ulcers/wounds in the extremities
- Critical limb ischemia (severe rest pain, tissue loss)
- Gangrene and limb amputation
- Renal Artery Stenosis:
- Refractory Hypertension (difficult to control)
- Chronic Kidney Disease progressing to kidney failure
- Mesenteric Ischemia:
- Chronic mesenteric ischemia (abdominal pain after eating, weight loss)
- Acute mesenteric ischemia (sudden, severe abdominal pain, bowel necrosis – a medical emergency)
- Aneurysms: Atherosclerosis can weaken arterial walls, leading to the formation of aneurysms (bulges or balloons in the artery), most commonly in the aorta (abdominal aortic aneurysm - AAA). Aneurysms can rupture, causing life-threatening internal bleeding.
Revision Questions:
- What is the fundamental difference between arteriosclerosis and atherosclerosis?
- A patient presents with sudden weakness on one side of their body and trouble speaking. Blockage in which arteries should be suspected?
- List five major modifiable risk factors for the development of atherosclerosis.
- What is the primary goal of surgical procedures like angioplasty or coronary artery bypass surgery in managing atherosclerosis?
- Describe three key nursing interventions for a patient with severe atherosclerosis experiencing chest pain.