Table of Contents
ToggleDisorders of the Biliary System
Review of Liver Disorders
Liver disorders are common and can result from various causes, including viral infections (hepatitis) or exposure to toxic substances like alcohol. A significant and often fatal liver disorder is hepatocellular carcinoma, a highly malignant tumor that is difficult to treat. While it accounts for less than 1% of cancers in the United States, it is a major health issue elsewhere, accounting for up to 50% of cancer cases in some parts of the world. Liver cancer can originate in the liver (primary) or metastasize to the liver from other sites.
Anatomy and Physiology of the Liver
The liver is the largest gland in the body, weighing about 1,500 g (1.5 kg). It functions as a complex "chemical factory" that manufactures, stores, metabolizes, and excretes a vast number of substances essential for life.
Location and Structure
- The liver is located in the upper right portion of the abdominal cavity, situated behind the ribs.
- It is divided into four lobes. A thin layer of connective tissue surrounds each lobe and extends into it, dividing the liver mass into microscopic functional units called lobules.
Blood Circulation
The liver has a unique dual blood supply, which is critical to its function:
- Hepatic Portal Vein (approx. 75% of blood supply): This large vessel drains the GI tract and is rich in absorbed nutrients. This strategic location allows the liver to directly process nutrients from digestion, either storing them or transforming them into chemicals needed elsewhere in the body.
- Hepatic Artery (approx. 25% of blood supply): This vessel supplies the liver with oxygen-rich arterial blood.
Terminal branches of these two vessels mix in capillary beds called sinusoids, which bathe the liver cells (hepatocytes). The blood then collects in central veins, which merge to form the hepatic vein, finally draining into the inferior vena cava.
Bile Drainage
- Bile, produced by hepatocytes, is secreted into small ducts called canaliculi.
- These canaliculi merge to form larger bile ducts, which eventually form the main hepatic duct.
- The hepatic duct joins with the cystic duct from the gallbladder to form the common bile duct.
- The common bile duct empties into the duodenum, and the flow of bile is controlled by the sphincter of Oddi.
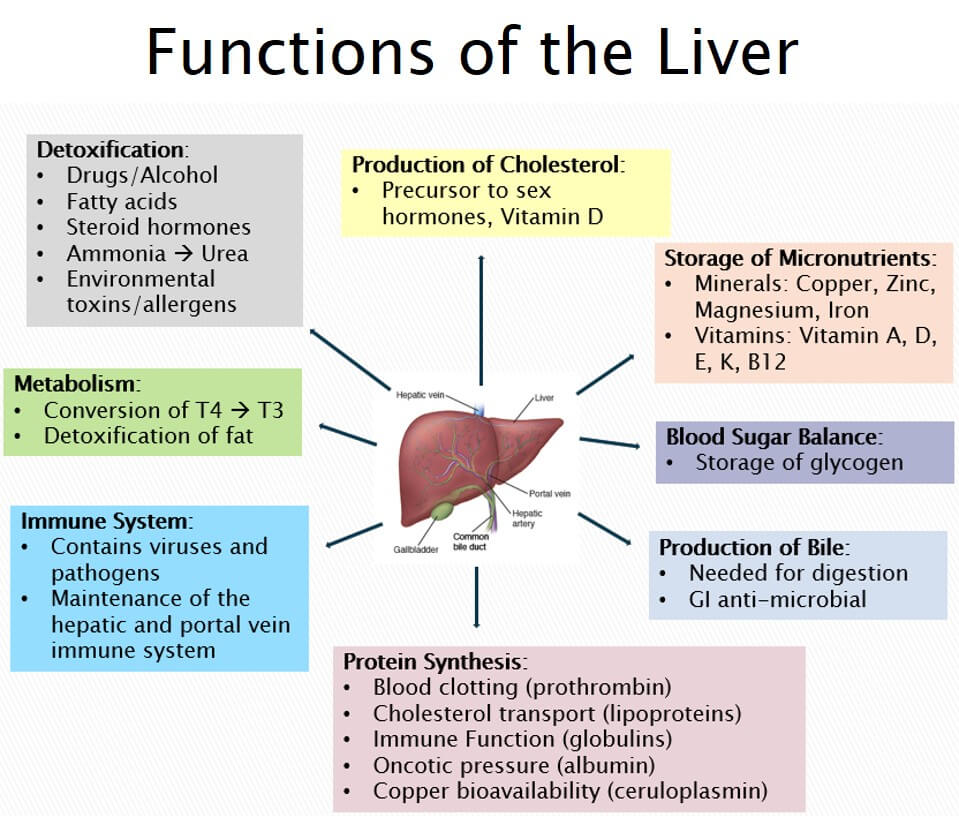
Major Functions of the Liver
- Glucose Metabolism: Plays a central role in maintaining blood glucose levels through processes like glycogenesis (storing glucose as glycogen), glycogenolysis (releasing glucose), and gluconeogenesis (creating glucose from non-carbohydrates).
- Protein Metabolism: Synthesizes most plasma proteins, including albumin (maintains osmotic pressure) and clotting factors.
- Fat Metabolism: Breaks down fatty acids for energy, synthesizes cholesterol, and produces triglycerides.
- Ammonia Conversion: Converts toxic ammonia (a byproduct of protein breakdown) into urea, which is then excreted by the kidneys.
- Bile Formation: Manufactures and secretes bile, which is essential for the digestion and absorption of fats and fat-soluble vitamins in the GI tract.
- Bilirubin Excretion: Breaks down old red blood cells and excretes bilirubin (a component of hemoglobin) into the bile.
- Stores essential nutrients like vitamins (A, D, E, K, and B12) and minerals (iron and copper).
- Drug Metabolism: Metabolizes and detoxifies drugs, alcohol, and other harmful chemicals, making them less toxic and easier to excrete.
- Removes waste products and bacteria from the bloodstream.
Age-Related Changes of the Hepatobiliary System
- Steady decrease in the size and weight of the liver, particularly in women.
- Decrease in total blood flow to the liver.
- Decreased ability for replacement and repair of liver cells after injury.
- Reduced drug metabolism and a decline in drug clearance capability, increasing the risk of drug toxicity in the elderly.
- Slowed clearance of hepatitis B surface antigen.
- Increased prevalence of gallstones due to increased cholesterol secretion in the bile.
- Decreased gallbladder contraction after a meal, which can lead to inefficient bile emptying.

DISORDERS OF THE LIVER: JAUNDICE (Hyperbilirubinemia)
Key Facts
- Jaundice is a symptom, not a disease itself. It is characterized by a yellowish discoloration of the sclera (whites of the eyes) and skin.
- It is caused by an abnormally high concentration of the pigment bilirubin in the blood (hyperbilirubinemia).
- Bilirubin is a by-product of the normal breakdown of red blood cells. It is processed (conjugated) by the liver and then excreted into the bile.
- Jaundice becomes clinically evident when the total serum bilirubin level is approximately three times the normal level (above 2 to 3 mg/dL).
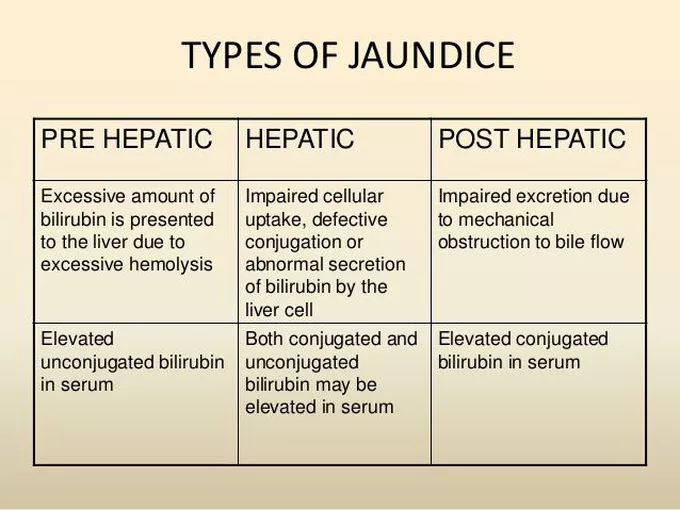
Types of Jaundice
Jaundice is classified into three main types based on where the disruption in bilirubin metabolism occurs.
1. Hemolytic Jaundice (Pre-hepatic)
This type is caused by an increased breakdown of red blood cells (hemolysis), which produces an amount of unconjugated bilirubin that exceeds the liver's capacity to process it. The liver itself is functioning normally.
Causes
- Blood Transfusion Reactions: Mismatched blood causes rapid destruction of transfused red blood cells.
- Hemolytic Anemias: Conditions where red blood cells are destroyed prematurely, such as Sickle Cell Disease.
- Sepsis / Severe Infections: Can lead to increased hemolysis.
- Pregnancy-Related Conditions: HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelet count).
- Disseminated Intravascular Coagulation (DIC): A condition causing widespread clotting and bleeding, which destroys red blood cells.
2. Hepatocellular Jaundice (Hepatic)
This type is due to the inability of damaged liver cells (hepatocytes) to clear normal amounts of bilirubin from the blood. The liver's ability to take up, conjugate, and excrete bilirubin is impaired.
Causes
- Hepatitis: Viral (A, B, C), alcoholic, or autoimmune inflammation of the liver.
- Drugs and Toxins: Many medications and toxins are harmful to the liver (hepatotoxic).
- Alcohol: Chronic, excessive alcohol consumption is a primary cause of liver damage.
- Cirrhosis: Late-stage scarring of the liver.
- Liver Tumors: Primary or metastatic cancer in the liver.
- Autoimmune diseases, Cholangitis, and certain herbal preparations.
3. Obstructive Jaundice (Post-hepatic)
This type results from an impeded or obstructed flow of bile through the liver or the biliary duct system. Bilirubin is conjugated by the liver but cannot be excreted into the duodenum.
Causes
The obstruction can be intrahepatic (within the liver) or extrahepatic (outside the liver).
- Gallstones: A common cause, blocking the common bile duct.
- Carcinoma of the Head of the Pancreas: A tumor that compresses the common bile duct.
- Liver Tumors, Hepatitis, or Cirrhosis: Can cause intrahepatic obstruction.
- Strictures: Narrowing of the bile ducts, often from previous surgery.
- Pancreatitis: Inflammation of the pancreas can cause swelling that obstructs the bile duct.
- Pressure from an Enlarged Organ.
Clinical Features of Jaundice
- General Symptoms: Lack of appetite, nausea, malaise, fatigue, weakness, and weight loss.
- Urine Changes: Passing of deep orange and foamy urine due to the presence of conjugated bilirubin (which is water-soluble and excreted by the kidneys).
- Stool Changes: Passing of light or clay-colored stools, as bilirubin is not reaching the intestine to be converted to stercobilin (the pigment that gives stool its brown color). This is a hallmark of obstructive jaundice.
- Skin Changes: Intense pruritus (itching) due to the deposit of bile salts on the skin.
- GI Symptoms: Dyspepsia and intolerance to fatty foods, as bile is not available for fat digestion.
Investigations
- Liver Function Tests (LFTs): To measure levels of bilirubin, liver enzymes (ALT, AST, ALP), and proteins (albumin) to assess liver function.
- Hepatitis Serology: Blood tests to rule out viral hepatitis A, B, and C.
- Blood Smear (BS): To rule out malaria, which can cause hemolysis.
- Hemoglobin Electrophoresis: To confirm sickle cell disease.
- Complete Blood Count (CBC): To assess for anemia and signs of bacterial infection.
- Abdominal Ultrasound Scan: A key imaging study to visualize the liver, gallbladder, and bile ducts, and to detect gallstones or dilated ducts indicative of obstruction.
- Renal Function Tests: To assess for any concurrent kidney abnormalities.
- Liver Biopsy: To obtain a tissue sample to diagnose conditions like cirrhosis or liver malignancy.
Management of Jaundice
The core principle guiding the management of jaundice, a yellow discoloration of the skin, sclera (whites of the eyes), and mucous membranes due to hyperbilirubinemia, is to identify and treat the specific underlying cause of the elevated bilirubin levels. Given the diverse etiologies of jaundice (pre-hepatic, hepatic, and post-hepatic), a comprehensive diagnostic workup is essential before initiating specific treatments. Management strategies are multifaceted, encompassing supportive care, targeted interventions for the primary condition, and symptom relief.
Key Management Strategies for Jaundice
- Rehydration with IV Fluids: Patients with jaundice, especially if accompanied by nausea, vomiting, or poor appetite (common in liver diseases or infections), are at risk of dehydration and electrolyte imbalances. Intravenous fluid administration is often necessary to correct these deficits, maintain hydration, and support overall physiological function.
- Nutritional Support: Depending on the cause and severity, nutritional support may be needed. Patients with chronic liver disease may require dietary modifications (e.g., restricted protein in hepatic encephalopathy) or nutritional supplements.
- Monitoring Vital Signs and Fluid Balance: Close monitoring helps detect signs of worsening liver function, infection, or dehydration.
- Antivirals: For viral hepatitis (e.g., Hepatitis B or C) that leads to hepatic jaundice, antiviral medications are prescribed to suppress viral replication and reduce liver inflammation. Examples include Lamivudine or Adefovir (older agents for Hepatitis B), or direct-acting antivirals (DAAs) for Hepatitis C, which have revolutionized treatment for this virus.
- Antibiotics: If jaundice is caused by bacterial infections, particularly those affecting the biliary tree such as cholangitis (inflammation of the bile ducts), antibiotics are crucial. Intravenous antibiotics (e.g., IV Ceftriaxone, Piperacillin-tazobactam) are often initiated promptly to control the infection and prevent sepsis.
- Antimalarials: In regions where malaria is endemic, severe malaria, particularly falciparum malaria, can cause jaundice due to hemolysis and liver dysfunction. Antimalarial drugs (e.g., IV Artesunate, quinine) are administered to treat the parasitic infection.
- Corticosteroids/Immunosuppressants: For autoimmune liver diseases (e.g., autoimmune hepatitis), immunosuppressive therapy with corticosteroids or other agents may be used to reduce inflammation and prevent further liver damage.
- Chelating Agents/Specific Therapies: For metabolic disorders causing jaundice (e.g., Wilson's disease with copper overload, hemochromatosis with iron overload), specific therapies like chelating agents or phlebotomy are employed.
- Cessation of Hepatotoxic Drugs: If drug-induced liver injury is suspected, the offending medication must be immediately discontinued.
- Strict Avoidance of Alcohol Intake: Alcohol is a potent hepatotoxin. For patients with any form of liver disease causing jaundice (e.g., alcoholic hepatitis, cirrhosis), complete and strict abstinence from alcohol is paramount to prevent disease progression, further liver damage, and improve prognosis.
- Dietary Adjustments: Depending on the type and severity of liver dysfunction, dietary changes might be recommended (e.g., low-sodium diet for ascites, adequate protein intake unless hepatic encephalopathy is severe, avoiding raw shellfish).
- Avoidance of Liver-Toxic Substances: Patients should be educated to avoid other substances known to be hepatotoxic, including certain over-the-counter medications or herbal supplements without consulting a physician.
- Medications to Control Severe Itching (Pruritus): Elevated bilirubin and bile salts in the skin can cause intense itching. Management includes:
- Cholestyramine or Colestipol: Bile acid sequestrants that bind bile acids in the gut, preventing their reabsorption and promoting excretion.
- Antihistamines: May offer some relief, especially from associated sedative effects.
- Ursodeoxycholic Acid (UDCA): Can help improve bile flow in cholestatic conditions.
- Rifampicin or Naltrexone: Used in severe, refractory cases under specialist guidance.
- Skin care: Lukewarm baths, gentle soaps, emollients, and avoiding irritating clothing.
- Pain Management: If jaundice is associated with pain (e.g., from gallstones or cholangitis).
- Management of Nausea/Vomiting: Antiemetics may be prescribed.
- Phototherapy: This treatment utilizes ultraviolet (UV) light to break down unconjugated bilirubin in the skin into water-soluble isomers that can be excreted in bile and urine without requiring conjugation in the liver. It is primarily and highly effective for neonatal jaundice, where the immature liver cannot efficiently conjugate bilirubin. It is not typically used for jaundice in adults unless specific rare conditions are present.
- Surgical/Endoscopic Procedures: These are crucial for managing post-hepatic (obstructive) jaundice, where a blockage in the bile ducts prevents bile flow.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A minimally invasive endoscopic procedure used to diagnose and treat conditions of the bile ducts and pancreatic duct. It can be used to relieve biliary obstruction by:
- Removing gallstones or common bile duct stones (choledocholithiasis).
- Placing stents to bypass strictures or tumors in the bile ducts.
- Taking biopsies to diagnose strictures or tumors.
- Percutaneous Transhepatic Cholangiography (PTC): An alternative to ERCP, involving a needle inserted through the skin into a bile duct, often used when ERCP is not feasible or successful, for drainage or stenting.
- Surgical Intervention: May be required to remove large or impacted gallstones, resect tumors causing obstruction (e.g., pancreatic cancer, cholangiocarcinoma), or perform reconstructive procedures on the biliary tree. For example, a cholecystectomy (gallbladder removal) is done for symptomatic cholelithiasis.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A minimally invasive endoscopic procedure used to diagnose and treat conditions of the bile ducts and pancreatic duct. It can be used to relieve biliary obstruction by:
- Liver Transplantation: For end-stage liver disease (e.g., from chronic hepatitis, cirrhosis, or certain genetic disorders) that has resulted in intractable jaundice and severe liver failure, liver transplantation may be the definitive treatment.
