Table of Contents
ToggleCHOLECYSTITIS
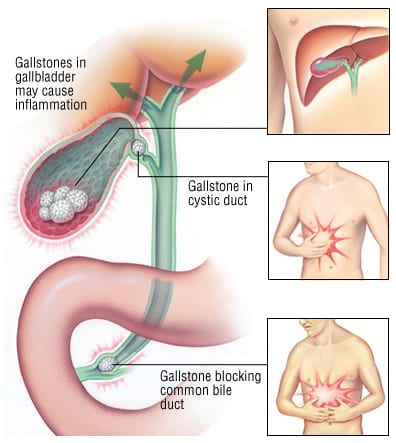
Cholecystitis is an inflammation of the gallbladder and/or the biliary tract. Acute cholecystitis typically causes pain, tenderness, and rigidity in the upper right abdomen, which may radiate to the midsternal area or right shoulder.
- Calculous Cholecystitis (90% of cases): This is the most common type. The inflammation is caused by a gallstone obstructing the cystic duct, leading to bile stasis. The trapped bile acts as a chemical irritant, resulting in inflammation, edema, and potential compromise of the vascular supply, which can lead to gangrene.
- Acalculous Cholecystitis: This describes acute gallbladder inflammation that occurs in the absence of obstruction by gallstones. It typically occurs in critically ill patients after major surgery, severe trauma, or burns.
Causes
- Obstruction of the cystic duct by gallstones (most common cause).
- Major abdominal trauma or severe burns.
- Major surgery (especially abdominal surgery).
- Multiple blood transfusions.
- Primary bacterial infections of the gallbladder (e.g., from E. coli, Klebsiella).
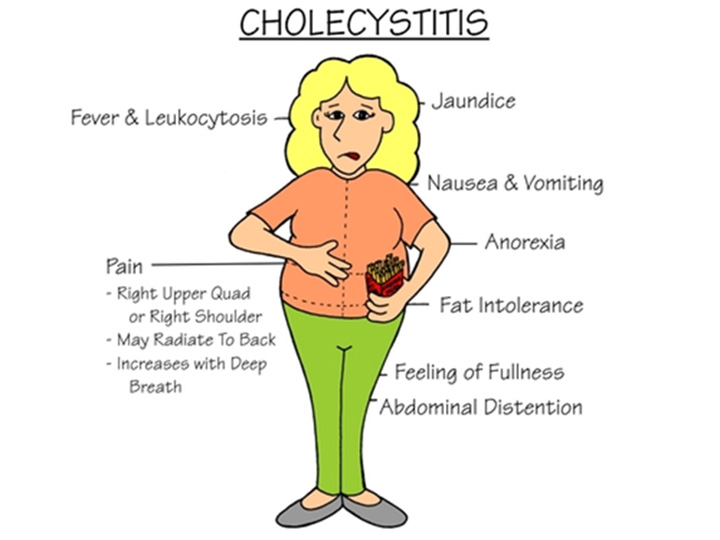
Clinical Features of Cholecystitis
- Jaundice: Yellow discoloration of the skin and sclera due to the buildup of bilirubin if a stone obstructs the common bile duct.
- Changes in Urine and Stool: Very dark urine (due to bilirubin excretion in urine) and clay-colored stools (due to lack of bilirubin in stool) are indicative of complete bile duct obstruction.
- Severe Pruritus (itching): Due to bile salt deposition in the skin.
- Vitamin Deficiency: Impaired bile flow can lead to poor absorption of fat-soluble vitamins (A, D, E, and K), which can manifest as night blindness (A), bone problems (D), neurological issues (E), and bleeding tendencies (K).
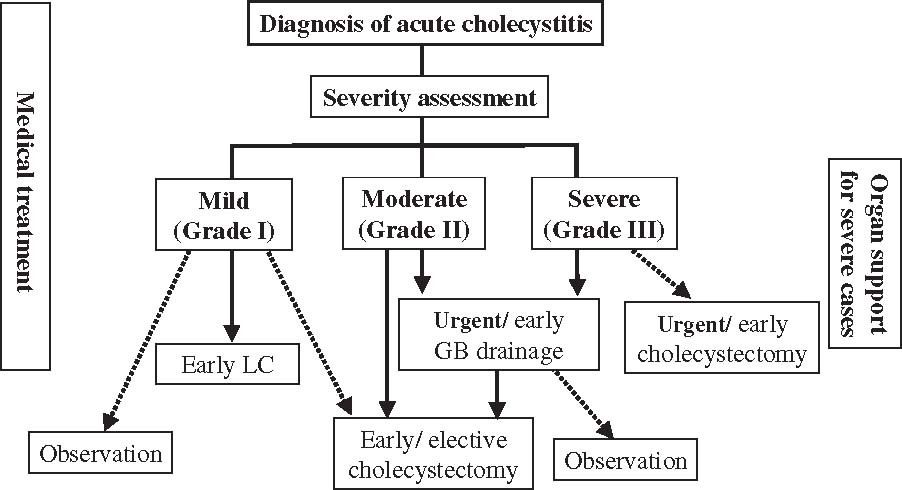
Classification of Acute Cholecystitis
The severity is classified into three grades to guide treatment and prognosis (Tokyo Guidelines 2018):
- Elevated white blood cell count (WBC > 18,000/mm³)
- Palpable tender mass in the RUQ
- Duration of symptoms > 72 hours
- Evidence of local inflammation (e.g., pericholecystic fluid, localized peritonitis, phlegmonous cholecystitis on imaging)
Investigations
- Liver Function Tests (LFTs): Elevated bilirubin, alkaline phosphatase, ALT, and AST may indicate biliary obstruction (cholestasis) or liver involvement.
- Renal Function Tests: Urea, creatinine, and electrolytes are monitored to assess kidney function, especially in critically ill patients or those with dehydration.
Complications of Acute Cholecystitis
- Empyema or Abscess: Formation of pus within the gallbladder, leading to severe localized infection. This is a life-threatening complication.
- Perforation: Rupture of the inflamed and necrotic gallbladder wall, leading to leakage of bile into the peritoneal cavity, causing biliary peritonitis (a severe and generalized infection of the abdominal cavity). This often requires emergency surgery.
- Fistula Formation: An abnormal connection between the gallbladder and an adjacent organ (e.g., duodenum, colon), known as a cholecystoenteric fistula. This can lead to gallstone ileus if a large stone passes into the bowel and obstructs it.
- Gangrene of the gallbladder: This occurs due to severe inflammation and compromised blood supply, leading to tissue death. It significantly increases the risk of perforation.
- Gallstone Ileus: Mechanical bowel obstruction caused by a large gallstone that has passed into the intestinal lumen, usually through a cholecystoenteric fistula.
- Choledocholithiasis: The presence of gallstones in the common bile duct, which can lead to cholangitis (infection of the bile ducts) or pancreatitis.
- Cholangitis: An acute inflammation and infection of the bile ducts, usually due to obstruction by stones and bacterial ascent from the duodenum. It is a severe, life-threatening condition.
- Pancreatitis: Inflammation of the pancreas, often caused by a gallstone obstructing the common bile duct at the ampulla of Vater, causing reflux of bile into the pancreatic duct.
Management of Cholecystitis
Management of acute cholecystitis typically involves a combination of conservative (medical) and surgical approaches, tailored to the patient's severity (as per the Tokyo Guidelines classification), co-morbidities, and clinical response.
Conservative Management (Medical)
This approach is often used initially to stabilize the patient, particularly in mild to moderate cases, or as a bridge to definitive surgical treatment.
Aims of Medical Management
- To treat and prevent the underlying cause of inflammation, primarily bacterial infection.
- To relieve symptoms, especially severe pain, nausea, and vomiting.
- To prevent further complications, such as gallbladder perforation, gangrene, or systemic sepsis.
- To optimize the patient's condition for eventual surgical intervention, if indicated.
Interventions
- Nil Per Mouth (NPO/NBM - Nil by Mouth): The patient is kept NPO to rest the gastrointestinal tract and, crucially, to minimize stimulation of the gallbladder, reducing pain and inflammation. This prevents further contraction of the gallbladder and bile flow.
- Intravenous (IV) Fluids: Essential to maintain adequate hydration, correct any electrolyte imbalances (especially if the patient has been vomiting), and provide a route for medication administration.
- Pain Management: Analgesics are given to control severe pain. Opioids like Pethidine (meperidine) or morphine are commonly used. Non-steroidal anti-inflammatory drugs (NSAIDs) may also be used in conjunction or for milder pain, provided there are no contraindications (e.g., renal impairment, bleeding risk).
- Note: Historically, morphine was thought to cause spasm of the sphincter of Oddi, but current evidence suggests its clinical significance in this context is minimal, and it is a safe and effective analgesic for biliary pain.
- Antibiotics: IV antibiotics are administered promptly to treat and prevent bacterial infection, as bacterial invasion of the inflamed gallbladder wall is common. Broad-spectrum antibiotics covering common enteric organisms (e.g., E. coli, Klebsiella, Enterococcus) are typically initiated, such as third-generation cephalosporins (e.g., Ceftriaxone), fluoroquinolones (e.g., Ciprofloxacin), or combinations like Piperacillin-Tazobactam. The choice may be refined based on culture results if obtained (e.g., from bile).
- Antiemetics: Medications such as Ondansetron, Metoclopramide, or Prochlorperazine are administered to control nausea and vomiting, improving patient comfort and reducing the risk of dehydration.
- Nasogastric (NG) Tube: May be inserted if the patient has severe vomiting or gastric distension to decompress the stomach.
Surgical Management
Cholecystectomy (surgical removal of the gallbladder) is the definitive treatment for acute cholecystitis and is the standard of care for most patients. It eliminates the source of inflammation and prevents recurrence. The timing of surgery depends on the severity of the cholecystitis, the patient's overall condition, and the surgeon's preference.
- Laparoscopic Cholecystectomy: This is the most common and preferred surgical approach. It is a minimally invasive procedure performed through small incisions, offering benefits such as less pain, shorter hospital stay, and faster recovery. It is typically performed:
- Early (within 24-72 hours of symptom onset): This is increasingly favored, especially for mild to moderate cases, as it can reduce hospital stay and complications associated with prolonged inflammation.
- Delayed (after resolution of acute inflammation): For patients who are initially managed conservatively due to severe inflammation, co-morbidities, or delayed presentation. The patient is discharged and readmitted for elective surgery usually 6-8 weeks later, once the inflammation has subsided ("interval cholecystectomy").
- Open Cholecystectomy: This involves a larger incision in the abdomen and is reserved for cases where laparoscopic surgery is contraindicated or technically challenging (e.g., severe inflammation, adhesion, morbid obesity, suspicion of malignancy, or if complications arise during laparoscopic surgery).
- Percutaneous Cholecystostomy: In critically ill patients who are not surgical candidates due to high operative risk, a percutaneous cholecystostomy tube may be inserted under imaging guidance to drain the gallbladder and relieve pressure and inflammation. This is often a temporizing measure to stabilize the patient, with cholecystectomy performed later when the patient's condition improves.
Nursing Diagnoses and Interventions for Cholecystitis
Below are common nursing diagnoses for patients with cholecystitis, along with their associated nursing interventions.
1. Acute Pain
- Assess Pain: Use a standardized pain scale (0-10) to assess pain intensity, location, character, and aggravating/alleviating factors regularly.
- Administer Analgesics: Administer prescribed analgesics (opioids, NSAIDs) promptly and evaluate their effectiveness. Consider multimodal pain management.
- Positioning: Assist the patient to a comfortable position, often semi-Fowler's, to reduce pressure on the abdomen.
- Rest: Encourage bed rest during acute pain episodes to reduce metabolic demand and discomfort.
- NPO Status: Maintain NPO status as ordered to minimize gallbladder stimulation.
- Relaxation Techniques: Teach and encourage deep breathing, guided imagery, or distraction techniques.
- Post-operative Pain Management: Provide continuous assessment of incisional pain, administer analgesics (oral, IV, PCA), and encourage splinting the incision during coughing/movement.
2. Nausea and Vomiting
- Assess Nausea/Vomiting: Monitor frequency, amount, and character of emesis. Assess for associated symptoms (e.g., abdominal pain, dizziness).
- Administer Antiemetics: Give prescribed antiemetics (e.g., Ondansetron, Metoclopramide) promptly and evaluate effectiveness.
- Maintain NPO Status: Adhere to NPO orders. Progress diet slowly after symptoms subside, starting with clear liquids.
- Oral Hygiene: Provide frequent mouth care, especially after vomiting, to remove unpleasant tastes and odors.
- Environmental Control: Minimize unpleasant odors, provide a well-ventilated and quiet environment.
- IV Fluids: Ensure adequate IV fluid replacement to prevent dehydration and electrolyte imbalances.
- NG Tube Management: If an NG tube is in place, ensure it is patent and draining effectively.
3. Deficient Fluid Volume / Risk for Deficient Fluid Volume
- Monitor Fluid Balance: Accurately record strict intake and output. Monitor daily weight.
- Assess Hydration Status: Check skin turgor, mucous membranes, thirst, and capillary refill.
- Monitor Vital Signs: Assess for signs of hypovolemia (tachycardia, hypotension).
- Administer IV Fluids: Administer prescribed IV fluids as ordered to maintain hydration and correct electrolyte imbalances.
- Monitor Electrolytes: Review laboratory results for electrolyte abnormalities (e.g., sodium, potassium, chloride).
- Oral Rehydration: Once tolerated, encourage sips of clear fluids and gradually advance diet.
- Educate Patient/Family: On the importance of hydration and reporting symptoms of dehydration.
4. Risk for Infection (or Imbalanced Body Temperature: Hyperthermia)
- Monitor for Signs of Infection: Monitor temperature regularly (e.g., every 4 hours), assess for chills, increased pain, or localized tenderness. Review WBC count.
- Administer Antibiotics: Administer prescribed IV antibiotics promptly and ensure the full course is completed. Monitor for effectiveness and side effects.
- Aseptic Technique: Maintain strict aseptic technique for all invasive procedures (IV insertion, wound care post-op).
- Wound Care (Post-op): Assess surgical incision for redness, swelling, heat, pain, and drainage. Perform wound dressing changes as ordered using sterile technique.
- Pulmonary Hygiene (Post-op): Encourage deep breathing, coughing, and incentive spirometry to prevent atelectasis and pneumonia.
- Hydration and Nutrition: Promote adequate hydration and nutrition to support the immune system.
- Patient Education: Educate on signs of infection to report, proper hand hygiene, and wound care (if applicable).
5. Knowledge Deficit
- Assess Knowledge Level: Determine the patient's and family's current understanding of cholecystitis, its causes, treatment options, and post-discharge care.
- Provide Information: Explain the diagnosis, planned investigations, medical management, and surgical options in clear, understandable language. Use visual aids if helpful.
- Pre-operative Teaching: If surgery is planned, educate on the procedure, expected post-operative course, pain management, early ambulation, and wound care.
- Dietary Education: Explain the importance of a low-fat diet post-discharge to minimize discomfort and prevent recurrence, especially after cholecystectomy.
- Medication Education: Discuss all prescribed medications (purpose, dose, frequency, side effects, storage).
- Symptom Management: Educate on how to manage pain, nausea, and other symptoms at home.
- Warning Signs: Instruct on when to seek immediate medical attention (e.g., worsening pain, fever, jaundice, persistent vomiting).
- Follow-up Care: Emphasize the importance of attending follow-up appointments.
- Encourage Questions: Create an open environment for questions and clarification. Provide written materials for reinforcement.