ANAEMIA IN PREGNANCY
Anaemia during pregnancy refers to a condition where the red blood cell count or haemoglobin level in the mother’s blood is lower than normal. Anaemia in pregnancy is defined as haemoglobin (Hb) concentration is less than 11 g/dl.
Anaemia means a reduction in oxygen carrying capacity or in quantity of red blood cells. Red blood cells carry oxygen throughout the body, and low levels can lead to oxygen deprivation for both the mother and developing fetus.
This may be due to:
- A reduction in the number of red blood cells.
- A low concentration haemoglobin .
- A combination of both
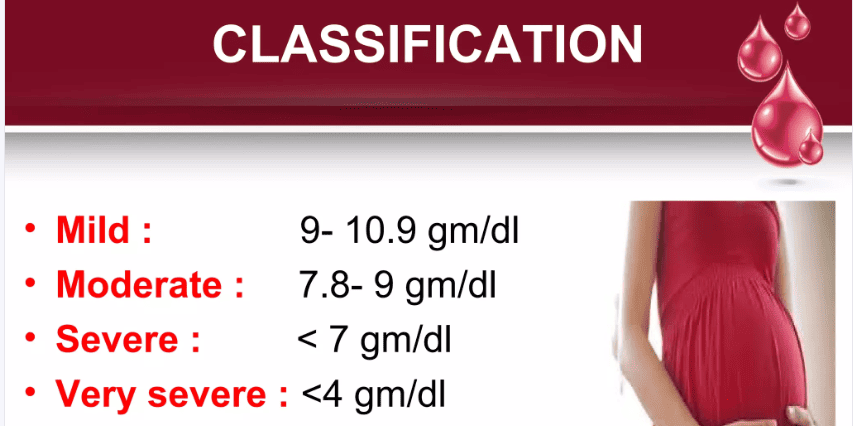
Classifications/Degrees of Anaemia
- Mild anaemia: haemoglobin levels between 9.0 and 10.9 g/dL.
- Moderate anaemia: haemoglobin levels between 7.8 and 9.0 g/dL.
- Severe anaemia: haemoglobin levels below 7.0 g/dL.
- Very Severe anaemia: haemoglobin levels below 4.0 g/dL.
Causes of anaemia in Pregnancy
1. Social and Economic Factors:
- Ignorance about utilizing food: Lack of knowledge about nutritious food sources and dietary practices, especially for iron-rich foods.
- Poverty: Inability to afford a balanced diet rich in protein, iron, and other essential nutrients.
- Unstable country / Insecurity: Conflict, displacement, and lack of access to healthcare resources can contribute to malnutrition and anaemia.
- Beliefs and Cultural Superstitions: Certain cultural beliefs or practices might restrict the consumption of essential foods like chicken, eggs, or other iron-rich sources.
2. Obstetrical Causes:
- Frequent childbearing: Closely spaced pregnancies can deplete iron stores, making anaemia more likely.
- Repeated Hemodilution: The blood volume expands significantly during pregnancy to accommodate the needs of the growing fetus. This expansion can dilute the existing red blood cells, leading to lower haemoglobin levels even if the body is producing enough red blood cells.
- Multiple Pregnancy: The fetus requires iron for growth and development. The mother also needs extra iron to support the increased blood volume and oxygen delivery. This increased demand can deplete iron stores, leading to iron-deficiency anaemia.
- Hyperemesis Gravidarum: Severe morning sickness can lead to poor absorption of nutrients, including vitamin B12, which is crucial for red blood cell production.
- Abortions, Ruptured Ectopic Pregnancies, Postpartum Hemorrhage (PPH), Antepartum Hemorrhage (APH), and Heavy Periods: These conditions can lead to blood loss and iron deficiency.
3. Medical Causes:
- Frequent Attacks of Malaria: Malaria infection destroys red blood cells, contributing to anaemia.
- Hookworm Infestation: Hookworms can cause blood loss from the intestines, leading to iron deficiency anaemia.
- Infections: Infections like septicemia (blood poisoning) and tuberculosis (TB) can impair red blood cell production.
- Sickle Cell anaemia: A genetic blood disorder characterized by abnormal red blood cells, leading to chronic anaemia.
- Drugs: Certain medications like chloramphenicol can interfere with red blood cell production and contribute to anaemia.
Other Factors
- Dietary Deficiencies: Inadequate intake of iron, folate, and vitamin B12 are common contributing factors to anaemia.
- Underlying Medical Conditions: Conditions like celiac disease, chronic kidney disease, or certain types of cancer can impair the body’s ability to produce red blood cells.
- Previous anaemia: Women with a history of anaemia before pregnancy are more likely to experience it again.
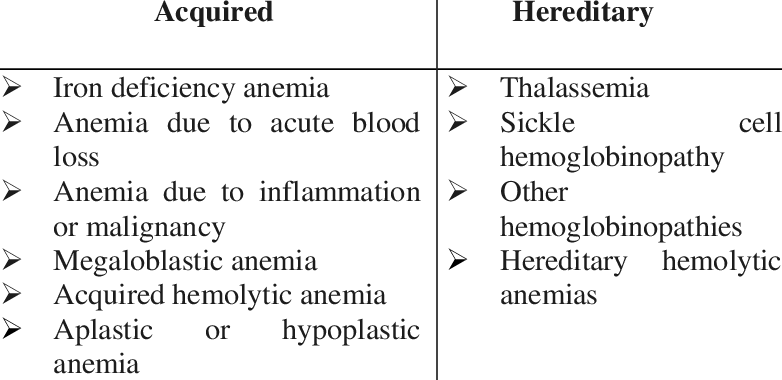
Types of Anaemia
- Physiological anaemia.
- Nutritional anaemia.
- Aplastic anaemia.
- Haemorrhagic anaemia.
- Haemolytic anaemia.
- Pernicious anaemia.
1. Physiological Anaemia: A temporary, physiological decrease in haemoglobin levels, often during pregnancy. This type of anaemia is considered “normal” during pregnancy and is primarily due to hemodilution. As the blood volume increases by 25-30% during pregnancy to accommodate the growing fetus, the concentration of red blood cells (and haemoglobin) appears to decrease, leading to a diluted blood picture.
- Hemodilution: During pregnancy, blood volume increases significantly, diluting the haemoglobin concentration. This is a normal adaptation to support the growing fetus and placenta.
- Increased Iron Demand: The growing fetus requires a substantial amount of iron for development, potentially leading to a temporary iron deficiency.
- Physiological anaemia is usually mild and resolves itself after childbirth.
2. Nutritional Anaemia: Anaemia caused by dietary deficiencies of essential nutrients required for RBC production. Nutritional anaemia can present as;
- Iron Deficiency Anaemia: The most common type, caused by insufficient iron intake or absorption. Iron is essential for haemoglobin synthesis. Inadequate iron leads to smaller, paler RBCs (hypochromic microcytic anaemia). The increased fetal demand for iron, especially from the 28th week onwards, exacerbates this issue. Excessive morning sickness can also contribute by reducing iron absorption.
- Folate Deficiency Anaemia (Megaloblastic Anaemia): A lack of folate (vitamin B9) disrupts DNA synthesis, leading to the formation of large, immature RBCs (megaloblasts). These cells are less effective at carrying oxygen.
- Vitamin B12 Deficiency Anaemia (Pernicious Anaemia): A deficiency in vitamin B12, important for DNA synthesis and maturation of RBCs, results in megaloblastic anaemia. A lack of protein can also contribute to this type.
- Vitamin C Deficiency: Vitamin C is important for iron absorption. Its deficiency can worsen iron deficiency anaemia.
- Impact: Nutritional anaemia is preventable and treatable with dietary modifications and supplementation.
3. Aplastic Anaemia: A rare and serious condition characterized by the suppression of bone marrow activity, resulting in reduced production of all blood cell types, including RBCs. The most common cause being Bone Marrow Failure, The bone marrow, responsible for blood cell production, becomes unable to generate enough RBCs. This can be caused by various factors, including:
- Drug-induced: Prolonged use of certain medications like chloramphenicol can suppress bone marrow function.
- Radiation Exposure: Exposure to ionizing radiation can suppress bone marrow function, since they can damage bone marrow cells.
- Diseases: Conditions like leukemia, cancer, and autoimmune diseases can affect bone marrow activity.
- Toxins: Exposure to toxic chemicals can damage bone marrow cells.
- Aplastic anaemia can be life-threatening. It requires immediate medical attention and may necessitate bone marrow transplantation or other intensive treatments.
4. Hemorrhagic anaemia: Anaemia resulting from excessive blood loss, leading to a reduction in circulating RBCs. This type results from excessive blood loss, which can occur due to a variety of reasons:
- Frequent Childbearing: Closely spaced pregnancies can deplete iron stores and increase the risk of blood loss during delivery.
- Worm Infestations: Hookworm infestation can lead to chronic blood loss from the intestines.
- Abortions, PPH, and APH: These conditions can lead to significant blood loss.
- Ruptured Ectopic Pregnancy: A ruptured ectopic pregnancy can cause internal bleeding.
- Trauma and Accidents: Trauma or accidents can cause severe blood loss.
- Gastrointestinal Bleeding: Conditions like ulcers, gastritis, and esophageal varices can cause internal bleeding.
- Acute Blood Loss: Sudden and significant blood loss, often due to trauma, surgery, or internal bleeding, causes a rapid decrease in RBCs.
- Chronic Blood Loss: Persistent, slow blood loss, often from gastrointestinal bleeding or heavy menstrual periods, gradually depletes the body’s iron stores and reduces RBC production.
- Hemorrhagic anaemia can be severe, particularly in cases of acute blood loss. Treatment focuses on stopping the bleeding and replacing lost blood.
5. Hemolytic anaemia: Anaemia caused by the premature destruction of RBCs (hemolysis), leading to a shortage of healthy RBCs in circulation. This may be due to,
Intrinsic Defects: Hemolysis can be caused by abnormalities within the RBCs themselves, such as:
- Sickle Cell Disease: This genetic disorder leads to the production of abnormal red blood cells that are easily destroyed. An inherited disorder where RBCs adopt a sickle shape, making them fragile and prone to destruction.
- Thalassemia: Genetic disorders that impair haemoglobin production, leading to weakened RBCs.
Extrinsic Factors: Factors outside the RBC can also trigger hemolysis:
- Infections: Infections like septicemia, pyelonephritis, and bacterial streptococcal infections can destroy red blood cells.
- Diseases: Malaria is a common cause of hemolytic anaemia due to its destruction of red blood cells.
- Mismatched Blood Transfusion: Receiving mismatched blood can lead to an immune reaction that destroys red blood cells.
- Immune Reactions: Antibodies against RBCs, often due to blood transfusions or autoimmune disorders, can cause hemolysis.
- Drugs: Certain medications like primaquine can cause hemolytic anaemia.
6. Pernicious anaemia: A specific type of megaloblastic anaemia caused by a deficiency in vitamin B12, usually due to a lack of intrinsic factor, a protein produced in the stomach that helps the body absorb vitamin B12. Pernicious anaemia is less common during childbearing years, but can occur due to:
- Autoimmune Destruction of Parietal Cells: In most cases, pernicious anaemia is caused by an autoimmune attack on the parietal cells in the stomach, leading to a deficiency of intrinsic factor.
- Diseases of the Stomach: Conditions like stomach cancer can interfere with intrinsic factor production.
- Hyperemesis Gravidarum: Severe morning sickness can lead to vitamin B12 deficiency due to poor absorption.
- Gastrectomy or Gastric Bypass Surgery: These procedures can reduce intrinsic factor production, impairing vitamin B12 absorption.
- Other Causes: Conditions like Crohn’s disease and celiac disease can also interfere with vitamin B12 absorption.

Signs and Symptoms of Anaemia in Pregnancy
Anaemia’s signs and symptoms can vary depending on the severity and underlying cause.
On History Taking
- General Body Weakness: This is usually the most common symptom, resulting from the body’s reduced oxygen-carrying capacity.
- Dizziness and Faintness: Reduced blood flow to the brain can cause lightheadedness and a feeling of faintness.
- Palpitations: The heart may beat faster to compensate for the reduced oxygen supply.
- Loss of Appetite (Anorexia): A decrease in appetite can be associated with anaemia.
- Headaches: Headaches can be caused by reduced oxygen to the brain.
- Breathlessness: The lungs may work harder to deliver oxygen to the body’s tissues.
- Shortness of Breath: Increased effort for the heart to pump oxygenated blood.
- History of Heavy Bleeding: A history of significant blood loss, such as from trauma, surgery, or gastrointestinal bleeding, can be a contributing factor.
On Examination
- Pale Mucous Membranes and Conjunctiva: This refers to the paleness of the gums, lips, tongue, soles of the feet, and palms of the hands, which are visible indicators of reduced haemoglobin.
- Distention of the Jugular Veins: This can be seen in severe cases of anaemia due to a decrease in blood volume.
- Edema (Swelling): Swelling of the ankles, feet, or even generalized edema can occur in severe cases.
- Enlarged Spleen and Liver: Palpation of the abdomen might reveal an enlarged spleen and liver, indicating an increase in red blood cell destruction or storage.
- Jaundice: Yellowing of the skin and whites of the eyes can occur in some types of anaemia, particularly those related to red blood cell breakdown.
- Cold Hands and Feet: Poor blood flow can lead to cold extremities.
Laboratory Tests
- Haemoglobin Level: The most crucial test for anaemia, measuring the amount of haemoglobin in the blood. Levels below 12.5 g/dL are generally considered anaemic.
- Increased Susceptibility to Infections: A weakened immune system makes pregnant women more prone to infections.
Diagnosis
Anaemia diagnosis relies on a combination of factors:
- History: A detailed history of the patient’s symptoms, diet, medical history, medications, and potential exposures helps narrow down the possible causes.
- Physical Examination: Careful assessment for physical signs like pallor, edema, and enlarged organs provides further clues.
- Laboratory Investigations:
- Haemoglobin Estimation: Confirming a low haemoglobin level.
- Packed Cell Volume (PCV): Measures the percentage of red blood cells in the blood.
- Blood Film: Examining the shape, size, and maturity of red blood cells, identifying specific features like:
- Microcytosis and Hypochromia: Small, pale red blood cells (iron deficiency)
- Megaloblastic Cells: Large, immature red blood cells (vitamin B12 and folate deficiency)
- Sickle Cells: Abnormal, crescent-shaped red blood cells (sickle cell anaemia)
- Target Cells: Red blood cells with a bullseye appearance (thalassemia)
- Reticulocytes: Immature red blood cells (indicating red blood cell production)
- Blood Sugar (BS) for Malarial Parasites: To rule out malaria, a common cause of anaemia in certain regions.
- Sickling Test: To confirm the presence of sickle cells in cases of suspected sickle cell disease.
- Coombs Test: To detect antibodies against red blood cells, suggesting autoimmune hemolytic anaemia.
- Bone Marrow Examination: To assess the bone marrow’s ability to produce red blood cells and identify any abnormalities.
- Urinalysis: To check for protein, indicating kidney damage, and to examine for red blood cells or other abnormalities.
- Stool Examination: To identify intestinal parasites like hookworms, which can cause anaemia.
- Haemoglobin Electrophoresis: To confirm sickle cell disease.
Iron Requirements During Pregnancy
- Increase in Maternal Haemoglobin (400-500 mg): The mother’s blood volume expands significantly during pregnancy, requiring an increased production of red blood cells, which in turn need iron to carry oxygen.
- The Fetus and Placenta (300-400 mg): The growing fetus requires iron for its own red blood cell production and development. The placenta also needs iron for its own functioning and to support fetal growth.
- Replacement of Daily Loss (250 mg): Iron is lost daily through urine, stool, and skin. This loss needs to be replenished to maintain adequate iron stores.
- Replacement of Blood Lost at Delivery (200 mg): Labour and delivery can involve significant blood loss, requiring iron replenishment afterwards.
Total Iron Needs: These factors contribute to a total iron requirement of approximately 1,500 mg during pregnancy.
Other Essential Nutrients:
- Elemental Iron: Recommended daily intake is 30 mg to 60 mg for pregnant women.
- Folic Acid: Recommended daily intake is 400 µg (0.4 mg) to prevent neural tube defects in the fetus.
Effects of anaemia on pregnancy and labour
Effects on Pregnancy:
General Body Fatigue: Anaemia leads to decreased oxygen carrying capacity, causing widespread fatigue, breathlessness, palpitations, and headaches.
Placental Insufficiency: Reduced oxygen delivery to the placenta can lead to:
- Intra-Uterine Fetal Death (IUFD): The fetus may not receive enough oxygen to survive.
- Small for Dates (SFD): The fetus may not grow at the expected rate due to insufficient nutrient and oxygen supply.
- Neonatal Death: anaemia can increase the risk of death in the newborn.
- Abortion and Premature Labour: Anaemia can increase the risk of both.
Increased Risk of Complications:
- Postpartum Haemorrhage: Anaemia can impair blood clotting, making mothers more susceptible to excessive bleeding after delivery.
- Heart Failure: The heart works harder to compensate for lower oxygen levels, increasing the risk of heart failure.
- Venous Thrombosis: Anaemia can increase blood viscosity, leading to blood clots in the veins.
- Infections: A weakened immune system due to anaemia makes mothers more vulnerable to infections.
- Poor Lactation: Anaemia can impact milk production and quality.
Effects on Labour:
- Stress of Labour: Anaemic women may struggle to tolerate the stress of labour, and even minor blood loss can be life-threatening.
- Fetal and Maternal Distress: Low oxygen levels can lead to fetal and maternal distress, potentially necessitating an instrumental delivery (e.g., forceps or vacuum extraction).
- Increased Risk of Complications: Anaemia can increase the risk of complications during labor, including postpartum haemorrhage, infection, and prolonged labor.
Management of anaemia in Pregnancy
Management of anaemia in pregnancy depends on the severity of the anaemia, stage of gestation, and underlying cause.
Early Pregnancy with Mild or Moderate anaemia in a Maternity Center and Hospital:
Outpatient Management:
- Put the mother in bed.
- Take a history from the mother concerning diet, lifestyle, and surroundings to determine the cause of anaemia.
- Conduct a general examination to assess the degree of anaemia using a Tallquist book.
- The midwife can treat mild and moderate anaemia in early pregnancy.
- Manage the condition according to the underlying cause.
- Refer the mother to the hospital for further investigations if haemoglobin is found to be below 60%.
Active Treatment for haemoglobin of 60% and Above:
- Administer three doses of Fansidar 960 mg tablets where malaria is common.
- Administer Mebendazole 200 mg twice daily for three days for hookworm.
- Provide iron therapy with ferrous sulfate (200 mg twice daily) and folic acid (5 mg once daily). Review after 2 months.
Note: In the maternity centre, refer moderate anaemia in late pregnancy to the hospital.
In the Hospital:
- Admit the mother to the antenatal ward.
- Take a history about diet, environment, and hygiene.
- Monitor observations: temperature, pulse, respirations, and blood pressure.
- Treat any underlying cause accordingly.
- Provide routine nursing care.
- Ensure proper hygiene.
- Provide a high-protein diet.
Severe anaemia in Early and Late Pregnancy:
In a Maternity Center:
- Refer to the hospital.
In the Hospital:
- Admit the mother and take a history.
- Conduct observations and investigations.
- Resuscitate immediately with:
- Blood transfusion or parenteral iron dextran (Inferon) infusion if blood is unavailable. Note: Total dose of Inferon is given slowly, only in severe anaemia close to delivery. After delivery, transfuse with packed cells under Lasix.
- Administer diuretics, e.g., Lasix 120 mg IV.
- Nurse the patient with severe anaemia propped up in bed and provide comprehensive care.
- Pay special attention to mouth care, as stomatitis and glossitis are common in anaemia patients.
- Provide a high-protein diet with green vegetables and fresh fruit.
- Maintain a strict fluid balance chart and observe for signs of impending cardiac failure, such as increasing pulse and respirations. Report breathlessness, especially if the patient has tuberculosis.
- Note: IV Inferon: 5 ampoules of 250 mg each in 100 ml of dextrose 5% or normal saline 500 ml.
Management During Labor:
1st Stage:
- Comfortable Positioning: Ensure the mother is in a comfortable position on the bed.
- Light Analgesia: Consider light pain relief measures as needed.
- Oxygenation: Administer oxygen to increase maternal blood oxygenation and prevent fetal hypoxia.
- Strict Asepsis: Maintain strict sterile practices to minimize infection risk.
2nd Stage:
- Usually No Specific Issues: This stage typically proceeds without major issues related to anaemia.
- Methergin or Oxytocin Administration: Administer 0.2 mg of Methergin or 20 units of oxytocin in 500 ml of Ringer’s Lactate intravenously, followed by 10 units intramuscularly, to prevent postpartum haemorrhage.
3rd Stage:
- Good management of the 3rd stage of labour to prevent much blood loss.
- Intensive Observation: Closely monitor for postpartum haemorrhage and other complications.
- Blood Replacement: Replace any significant blood loss with fresh packed red blood cells.
- Avoid Overloading: Be cautious not to exceed the amount of blood loss replaced to avoid fluid overload.
Puerperium (Postpartum Period):
- Bed Rest: Encourage bed rest to allow for recovery.
- Infection Monitoring and Treatment: Monitor for signs of infection and treat promptly.
- Continuation of Iron Therapy: Continue iron supplementation until haemoglobin levels return to normal.
- Dietary Guidance: Continue to promote a healthy, iron-rich diet.
- Counselling: Provide education and support to the mother and family regarding baby care and household chores.
Prevention of anaemia:
- Good Antenatal Care: Detect and treat anaemia and malaria early.
- Health Education: Teach about diet, personal hygiene, and environmental sanitation, including proper use of latrines.
- Malaria Protection: Take preventive measures against malaria.
- Blood Loss Reduction: Manage all stages of labour to reduce blood loss in the third stage.
- Protein Replacement: Provide extra protein during lactation.
- Folic Acid Supplementation: Administer as needed.
- Routine Blood Examinations: Monitor haemoglobin levels regularly.
- Avoidance of Frequent Childbirths: Spacing pregnancies adequately allows the body time to recover iron stores.
- Dietary Advice: Encourage a diet rich in iron-rich foods like red meat, fish, beans, lentils, and leafy green vegetables.
- Supplementary Iron Therapy: Prescribe iron supplements as needed, based on individual needs and blood tests.
- Treatment of Underlying Illnesses: Address any underlying medical conditions that may contribute to anaemia, such as infections, parasitic infestations, or chronic diseases. Early diagnosis and treatment are crucial.
Advice to the Mother:
- Tell the mother to report immediately when they become pregnant in order to receive appropriate prophylactic treatment of iron therapy.
- Explain the cause of anaemia, its dangers, and how to prevent it.
- Advise rest to avoid overworking.
- Discuss diet and types of food.
- Encourage taking any prescribed treatment regularly.
- Stress the importance of preventing mosquito bites to avoid malaria.
- Advise on family planning to avoid frequent childbearing.
- Recommend delivery in the hospital.
Complications of Anaemia in Pregnancy
Maternal Complications | Fetal Complications |
Increased risk of PPH | Premature birth |
Increased risk of infection | Low birth weight |
Increased risk of heart failure | Fetal growth restriction |
Fatigue and weakness | Stillbirth |
Shortness of breath | Cerebral palsy |
Increased risk of preeclampsia | Congenital anomalies |
Increased risk of delayed wound healing | Cognitive impairment |
Increased risk of death | Delayed development |


The notes are so good and easy to understand.
Thanks
Thanks a lot for the notes , it’s easy to understand
I hv learnt something,,
Thanks for compiling
Wow so easy to understand thanks for compiling
The notes is simple to understand thanks
Thanks for the work it’s summarised to understand
nice work we appreciate
The notes can be of help during health education since some mothers don’t like to take ferrous and folic,that it causes nausea.
Thanks
I want to know the pathophysiology of anemia