Status Epilepticus (SE) is a neurological emergency characterized by prolonged or repetitive seizure activity without full recovery of consciousness between seizures.
Historically, the definition was fixed at 30 minutes, but more recent understanding emphasizes the need for earlier intervention due to the risk of neuronal injury and treatment refractoriness.
- Time-Based Definition:
- The most widely accepted operational definition, particularly for convulsive SE (CSE), defines it as a seizure lasting longer than 5 minutes, or two or more seizures occurring within a 5-minute period without return to baseline consciousness between them.
- This "5-minute rule" is crucial for prompt clinical intervention. It is an operational definition, meaning it's designed to prompt action, not necessarily to reflect the exact pathophysiological threshold for neuronal damage.
- For non-convulsive SE (NCSE), the time threshold is generally considered 10 minutes or more of continuous or intermittent non-convulsive seizure activity.
- Physiological/Pathophysiological Definition:
- This refers to the point at which prolonged seizure activity leads to a failure of the normal mechanisms that terminate seizures, and continuous seizure activity results in long-term neuronal injury.
- T1 (Clinical Stage): The first time point (e.g., 5 minutes for convulsive SE) at which continuous seizure activity is likely to be prolonged. This is the point at which treatment should be initiated.
- T2 (Neuronal Injury Stage): The second time point (e.g., 30 minutes for convulsive SE) at which continuous seizure activity may lead to long-term neuronal injury, neuronal death, and/or alteration of neuronal networks (epileptogenesis) and may become resistant to treatment.
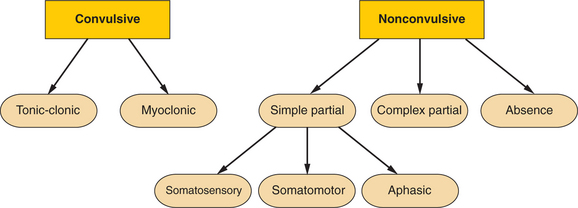
SE can be broadly classified based on its clinical presentation and electrographic features:
- Convulsive Status Epilepticus (CSE):
- Generalized Convulsive SE: Involves bilateral tonic-clonic motor activity. This is the most common and easily recognizable form of SE and carries the highest risk of systemic complications and mortality. It typically presents as continuous generalized tonic-clonic seizures or a series of such seizures without regaining consciousness.
- Focal Convulsive SE (or Epilepsia Partialis Continua - EPC): Characterized by continuous or repetitive focal motor activity (e.g., rhythmic jerking of a limb or facial twitching), which may remain localized or secondarily generalize. Consciousness may be preserved or impaired depending on the area of the brain involved.
- Non-Convulsive Status Epilepticus (NCSE):
- Characterized by continuous or fluctuating mental status changes and/or behavioral alterations due to ongoing non-convulsive seizure activity, without prominent motor manifestations. Diagnosis often requires Electroencephalography (EEG).
- Generalized NCSE (e.g., Absence Status, Atypical Absence Status): Presents as prolonged periods of unresponsiveness, confusion, staring, or subtle automatisms (e.g., lip-smacking). Common in patients with generalized epilepsy syndromes.
- Focal NCSE (e.g., Complex Partial Status): Can manifest with a wide range of symptoms, including confusion, aphasia, memory disturbances, bizarre behavior, or subtle focal neurological deficits. Often challenging to diagnose clinically without EEG.
- Subtle SE: A severe form of CSE where the prominent motor activity has subsided due to treatment or exhaustion, but continuous electrographic seizure activity persists, often with only minimal motor signs (e.g., subtle eye deviation, twitching of fingers). This is a particularly dangerous form as the ongoing brain injury may be missed without EEG monitoring.
This is considered as a complication of grand mal epilepsy rather than a certain type of epilepsy. It is both a medical and psychiatric emergency. This condition is life threatening and getting treatment started fast is vital.
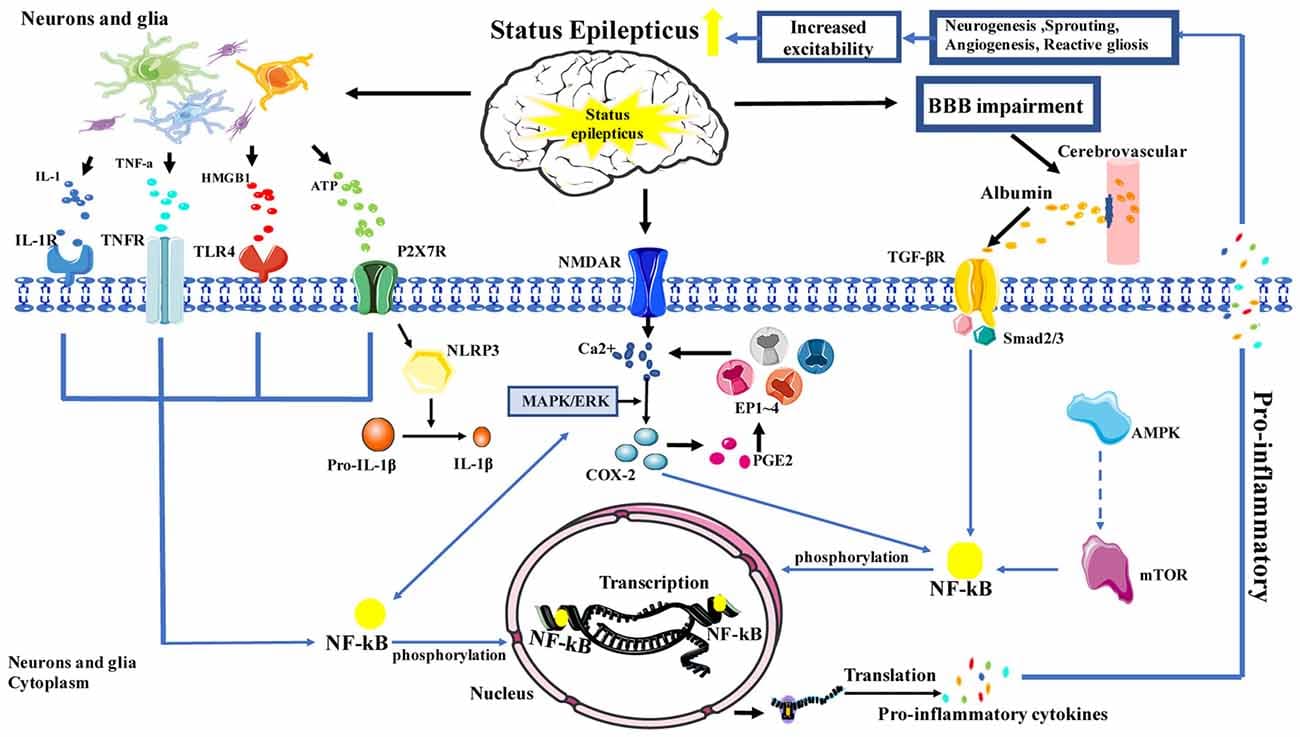
The pathophysiology of Status Epilepticus (SE) involves an interplay between excitatory and inhibitory neurotransmission, leading to a failure of normal seizure-terminating mechanisms.
Normally, a seizure is a self-limiting event. This self-termination is largely mediated by:
- GABAergic Inhibition: Gamma-aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the brain. When GABA binds to GABA-A receptors, it causes chloride influx, hyperpolarizing the neuron and making it less likely to fire. During normal seizures, there is an increase in GABA release and an upregulation of GABA-A receptor sensitivity to terminate the seizure.
- Ion Channel Modulation: As a seizure progresses, voltage-gated sodium channels in neurons undergo inactivation, reducing their ability to fire repeatedly. Potassium channels also open, leading to outward potassium current and neuronal hyperpolarization.
- Adenosine and Endocannabinoids: These neuromodulators also contribute to seizure termination by decreasing neuronal excitability.
In SE, these normal termination mechanisms fail or become overwhelmed:
- Internalization: Prolonged seizure activity leads to the internalization (endocytosis) of GABA-A receptors from the neuronal cell surface. This means fewer GABA-A receptors are available on the membrane to bind GABA, thus reducing inhibitory tone.
- Subunit Changes: There may be a shift in GABA-A receptor subunit composition, resulting in receptors that are less sensitive to GABA and benzodiazepines (a common first-line treatment for SE).
- Reduced GABA Synthesis/Release: In some cases, there may be reduced synthesis or release of GABA.
- Glutamate Hypersensitivity: Glutamate is the primary excitatory neurotransmitter. During SE, there is a sustained release of glutamate, which binds to N-methyl-D-aspartate (NMDA) and alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, leading to excessive calcium and sodium influx into neurons.
- NMDA Receptor Upregulation/Desensitization Failure: Unlike GABA-A receptors, NMDA receptors may be upregulated or fail to desensitize effectively during prolonged seizures, perpetuating excitotoxicity.
The pathophysiology of SE is often described in stages, highlighting the progressive nature of the failure of compensatory mechanisms and the increasing difficulty of treatment:
- Early Stage (Compensated Stage, 0-30 minutes):
- Seizure Onset: Initial compensatory mechanisms (GABA release, ion channel changes) are working but are overwhelmed by the underlying pathology (e.g., acute brain injury, electrolyte imbalance).
- Systemic Compensation: The body's autonomic nervous system responds to the increased neuronal activity. This includes increased heart rate, blood pressure, cardiac output, cerebral blood flow, and glucose utilization. Respiratory rate increases to maintain oxygenation.
- Drug Responsiveness: At this stage, seizures are generally responsive to first-line antiseizure medications, particularly benzodiazepines, which act on GABA-A receptors.
- Late Stage (Decompensated Stage, >30 minutes):
- Failure of Autoregulation: The initial systemic compensatory mechanisms begin to fail.
- Cerebral Edema & Ischemia: While initially cerebral blood flow increases, eventually, due to sustained metabolic demand, systemic hypotension, and increased intracranial pressure (from cerebral edema), cerebral blood flow becomes insufficient, leading to ischemia and hypoxia.
- Systemic Complications: Persistent muscle contractions (in CSE) lead to hyperthermia, lactic acidosis, rhabdomyolysis, respiratory failure, cardiac arrhythmias, and acute kidney injury.
- Neuronal Damage: Sustained excitotoxicity (due to excessive glutamate and calcium influx) leads to:
- Apoptosis and Necrosis: Neuronal cell death.
- Blood-Brain Barrier Breakdown: Can exacerbate cerebral edema and inflammation.
- Changes in Gene Expression: Leading to long-term alterations in neuronal excitability and increased risk of future seizures (epileptogenesis).
- Drug Refractoriness: Due to the internalization and subunit changes of GABA-A receptors, the brain becomes less responsive to benzodiazepines. Other antiseizure medications (which may work via different mechanisms, e.g., sodium channel blockade) may also become less effective.
Status Epilepticus (SE) can be caused by a wide variety of underlying conditions, ranging from acute brain injuries and systemic illnesses to chronic neurological disorders.
The causes of SE can be broadly categorized into acute, remote/chronic, and progressive, though many cases are multifactorial. The prevalence of different etiologies varies with age.
These are acute insults to the brain or severe systemic disturbances that directly trigger SE. They often carry a worse short-term prognosis.
- Acute Cerebrovascular Events:
- Stroke (Ischemic or Hemorrhagic): This is the most common cause in older adults.
- Subarachnoid Hemorrhage, Subdural Hematoma, Epidural Hematoma: Bleeding within or around the brain.
- Central Nervous System (CNS) Infections:
- Meningitis, Encephalitis, Brain Abscess: Inflammation or infection of the brain and its coverings.
- Acute Metabolic Derangements:
- Electrolyte Imbalances: Severe hyponatremia (low sodium), hypocalcemia (low calcium), hypomagnesemia (low magnesium), hypernatremia.
- Hypoglycemia/Hyperglycemia: Critically low or high blood sugar.
- Uremia, Hepatic Encephalopathy: Accumulation of toxins due to kidney or liver failure.
- Thyrotoxicosis: Severe hyperthyroidism.
- Traumatic Brain Injury (TBI):
- Severe head trauma can lead to immediate or delayed seizures.
- Toxic/Drug-Related Causes:
- Drug Withdrawal: Alcohol withdrawal (delirium tremens), benzodiazepine withdrawal, barbiturate withdrawal.
- Drug Intoxication: Cocaine, amphetamines, tricyclic antidepressants, isoniazid, penicillin, lithium, theophylline, organophosphates.
- Hypoxia/Anoxia:
- Severe oxygen deprivation to the brain (e.g., cardiac arrest, respiratory failure).
- Autoimmune and Inflammatory Conditions:
- Autoimmune Encephalitis: (e.g., NMDA receptor encephalitis, Hashimoto's encephalopathy).
- Systemic Lupus Erythematosus (SLE), Vasculitis.
These are pre-existing conditions that lower the seizure threshold. SE occurs either due to a breakthrough seizure or withdrawal of anti-seizure medication.
- Prior Brain Injury: Remote Stroke, Old TBI, Prior CNS Infection: Scars from previous insults can be epileptogenic.
- Developmental Brain Abnormalities: Cortical Dysplasia, Periventricular Heterotopia: Malformations of cortical development.
- Brain Tumors: Primary or metastatic brain tumors.
- Neurodegenerative Diseases: Alzheimer's disease, Creutzfeldt-Jakob disease (rarely).
- Genetic Epilepsy Syndromes: Certain genetic syndromes (e.g., Dravet syndrome, Lennox-Gastaut syndrome) are associated with a high risk of SE, particularly in children.
In a significant percentage of cases, especially in children, no specific cause can be identified despite thorough investigation.
Risk factors predispose an individual to developing SE, either by lowering their seizure threshold or increasing the likelihood of prolonged seizures.
- History of Epilepsy: This is the most significant risk factor. Patients with established epilepsy are at higher risk, especially if their seizures are poorly controlled.
- Non-compliance with Anti-Seizure Medications (ASMs): Abrupt discontinuation or irregular intake of prescribed ASMs is a very common and preventable cause of SE.
- Subtherapeutic ASM Levels: Due to poor absorption, drug interactions, or increased metabolism.
- Age: SE has a bimodal distribution, with the highest incidence in very young children (infants and toddlers) and the elderly.
- Children: Febrile seizures (prolonged febrile seizures can evolve into SE), CNS infections, hypoxic-ischemic encephalopathy, and genetic syndromes.
- Elderly: Acute stroke, neurodegenerative diseases, and systemic metabolic derangements are more common.
- Previous History of Status Epilepticus: Having experienced SE in the past significantly increases the risk of future episodes.
- Brain Pathology: Any pre-existing structural brain lesion (e.g., remote stroke, tumor, malformation) increases susceptibility.
- Alcoholism/Drug Abuse: Alcohol withdrawal is a major risk factor, as are intoxications with certain proconvulsant drugs.
- Systemic Illnesses: Severe medical conditions (e.g., sepsis, multi-organ failure) can create metabolic environments conducive to SE.
- Genetic Predisposition: Certain genetic factors can influence seizure susceptibility and the likelihood of developing SE.
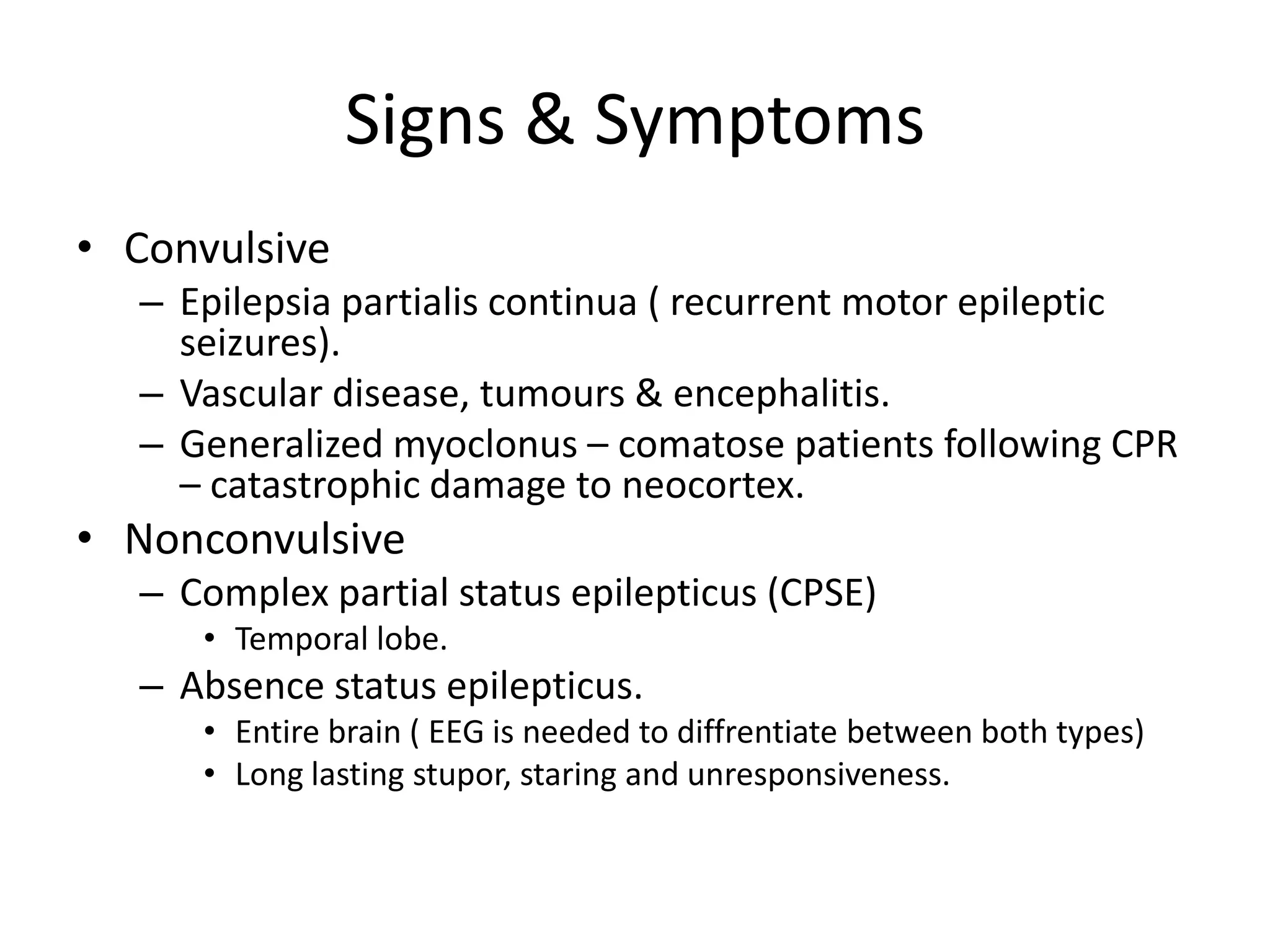
The presentation depends on whether it's convulsive or non-convulsive SE, its focal or generalized origin, and the duration of the activity.
CSE is the most easily recognizable and typically presents with prominent motor activity.
- Continuous or Repetitive Generalized Tonic-Clonic Seizures: This is the classic presentation.
- Tonic Phase: Sustained muscle contraction (stiffening) of the limbs, trunk, and face. The patient may arch their back, clench their jaw, and emit a cry or groan as air is forced past the vocal cords. Respiratory effort may cease (apnea), leading to cyanosis. Pupils are often dilated and unreactive.
- Clonic Phase: Rhythmic, jerky movements of the limbs and body, typically symmetrical. Breathing may be labored, and frothing at the mouth (sometimes blood-tinged if the tongue or cheek is bitten) may occur.
- Lack of Recovery: The defining feature is the absence of a return to baseline consciousness between individual seizures if they are repetitive, or the continuous nature of a single tonic-clonic seizure beyond 5 minutes.
- Autonomic Symptoms: Profound autonomic activation is common, especially early on:
- Tachycardia, Hypertension, Tachypnea: Increased heart rate, blood pressure, and respiratory rate.
- Hyperthermia: Elevated body temperature due to sustained muscle activity.
- Increased Secretions: Salivation, sweating.
- Pupil Dilation: Non-reactive pupils.
- Postictal Period (if seizures eventually terminate):
- Profound confusion, somnolence, headache, muscle aches, and sometimes transient focal neurological deficits (Todd's paralysis).
- Localized Motor Activity: Continuous or repetitive rhythmic jerking movements affecting only one part of the body (e.g., one limb, one side of the face, a finger). The patient may remain conscious or have impaired awareness depending on whether the seizure spreads.
- Spread (Secondary Generalization): The focal motor activity can sometimes spread to involve the entire body, becoming secondarily generalized tonic-clonic SE.
- Aura-like Symptoms (if conscious): Patients may report sensory phenomena (e.g., tingling, visual changes), autonomic symptoms (e.g., epigastric rising sensation), or psychological symptoms (e.g., fear, déjà vu) preceding or accompanying the motor activity if consciousness is preserved.
NCSE is often more challenging to diagnose clinically as it lacks the overt motor manifestations of CSE. It presents primarily as altered mental status or behavioral changes. A high index of suspicion and prompt EEG are often required for diagnosis.
- Generalized Non-Convulsive SE (e.g., Absence Status):
- Altered Consciousness: Prolonged periods of staring, blank expression, unresponsiveness, or reduced interaction with the environment.
- Subtle Motor Automatisms: May include slight eyelid fluttering, repetitive swallowing, lip-smacking, or minor head nodding. These are often brief and easily missed.
- Confusion/Disorientation: After resolution, patients may be confused or disoriented for a period.
- Amnesia: Patients may have no recollection of the event.
- Common in Patients with Generalized Epilepsy: Often seen in those with absence epilepsy.
- Focal Non-Convulsive SE (e.g., Complex Partial Status):
- Fluctuating or Sustained Altered Mental Status: Can range from mild confusion to coma.
- Behavioral Changes: Bizarre, agitated, or withdrawn behavior. Wandering, picking at clothes.
- Cognitive Deficits: Aphasia (difficulty with speech), memory disturbances, impaired attention, executive dysfunction.
- Affective Symptoms: Fear, anxiety, depression, unexplained crying or laughing.
- Autonomic Symptoms: Piloerection, flushing, heart rate changes.
- Sensory Symptoms: Persistent paresthesias, visual distortions, olfactory or gustatory hallucinations.
- Subtle Motor Signs: Twitching, eye deviation, or posturing that may be very minor.
- Rhythmic eye twitching or deviation.
- Nystagmoid eye movements.
- Facial twitching (e.g., corners of the mouth).
- Subtle finger or toe movements.
- Chewing or swallowing movements.
- Coma, unresponsiveness, or profound encephalopathy.
- Frequent or Clustering Seizures: Patients with epilepsy who experience an unusually high frequency of seizures over a short period may be at risk for progressing to SE.
- Prolonged Postictal State: A postictal period that is unusually long or severe after a typical seizure may indicate evolving SE or an underlying acute cause.
The overriding principle is expediency, as delays in diagnosis and treatment worsen outcomes.
- Time is Brain: The immediate priority is to recognize that SE is occurring based on the time-based definition (seizure > 5 minutes, or recurrent seizures without regaining consciousness).
- History (if available):
- Witness Accounts: Crucial for describing seizure semiology (movements, progression, duration, consciousness level), prior seizure history, presence of pre-existing epilepsy, medication adherence, recent illness, trauma, drug/alcohol use, and comorbidities.
- Emergency Personnel: Information from first responders about seizure duration and initial response to pre-hospital treatment.
- General Physical Examination:
- Vital Signs: Assess for hyperthermia, tachycardia, hypertension (initially), hypotension (later), tachypnea, oxygen saturation.
- Signs of Trauma: Head trauma, tongue lacerations, limb injuries.
- Signs of Systemic Illness: Rash, nuchal rigidity (meningitis), signs of liver/kidney disease.
- Neurological Examination:
- Assess level of consciousness (Glasgow Coma Scale), pupillary response, cranial nerve function, motor response (asymmetric weakness, posturing), and reflexes. Look for signs of Todd's paralysis after generalized seizures.
- Airway protection, breathing support, circulation maintenance.
- Administration of benzodiazepines (first-line treatment).
- Obtaining intravenous access.
- Initiating monitoring (cardiac, respiratory, oxygen saturation).
These are critical to identify underlying metabolic causes, assess for complications, and guide further management.
- Blood Glucose: ALWAYS the first lab to check due to the immediate need to correct hypoglycemia.
- Electrolytes: Sodium, potassium, calcium, magnesium, phosphate.
- Renal Function Tests: Blood Urea Nitrogen (BUN), Creatinine.
- Liver Function Tests: AST, ALT, Bilirubin (to rule out hepatic encephalopathy or assess liver injury).
- Arterial Blood Gas (ABG): To assess for metabolic acidosis (lactic acidosis is common), hypoxia, and hypercapnia.
- Full Blood Count (FBC): Look for signs of infection (leukocytosis), anemia, or thrombocytopenia.
- Toxicology Screen: For illicit drugs, alcohol, and potentially proconvulsant medications.
- Antiepileptic Drug (AED) Levels: If the patient is on chronic AEDs, check plasma levels to assess for subtherapeutic levels or non-adherence.
- Serum Creatine Kinase (CK): Elevated in rhabdomyolysis due to prolonged muscle activity.
- Lactate: Often elevated in convulsive seizures.
- Confirms SE: EEG definitively identifies continuous epileptiform activity. It is essential for diagnosing non-convulsive SE (NCSE), subtle SE, and for differentiating SE from non-epileptic seizures or other encephalopathies.
- Monitors Response to Treatment: Helps to determine if seizure activity has truly ceased, especially in patients who remain comatose after treatment.
- Prognostic Value: Certain EEG patterns (e.g., burst suppression) can indicate severity and help predict outcome.
- Types of EEG:
- Routine EEG: A standard recording (typically 20-30 minutes), often used as an initial assessment, but may miss intermittent activity.
- Continuous EEG (cEEG): Crucial in patients with altered mental status, unexplained coma, or when there is suspicion of NCSE or subtle SE. It allows for prolonged monitoring to capture seizure activity that might otherwise be missed.
Used to identify structural lesions or acute processes that are causing SE.
- Non-contrast Head CT:
- Often the first neuroimaging study performed, especially in the emergency setting.
- Rapidly identifies acute intracranial hemorrhage (stroke, trauma), large tumors, hydrocephalus, or signs of acute cerebral edema.
- May be normal in many cases of SE, especially those due to metabolic causes or remote lesions.
- Brain MRI with and without contrast:
- More sensitive than CT for detecting subtle structural lesions (e.g., cortical dysplasia, small tumors, encephalitis, remote ischemic injury) that may be the underlying cause of SE.
- Often performed after initial stabilization and if CT is non-diagnostic.
- Can show transient changes (e.g., T2/FLAIR hyperintensities) in cortical regions actively involved in prolonged seizure activity.
- Considered if there is suspicion of CNS infection (meningitis, encephalitis) or autoimmune encephalitis, especially if fever, nuchal rigidity, or altered mental status are prominent and other causes are ruled out.
- Should be performed after neuroimaging has excluded intracranial mass lesions or signs of increased intracranial pressure that would contraindicate LP.
- Cardiac Monitoring: To detect arrhythmias.
- Chest X-ray: To assess for aspiration pneumonia or pulmonary edema.
- Electrocardiogram (ECG): To rule out cardiac causes of syncope or evaluate for effects of electrolyte imbalances.
The emergency management of Status Epilepticus (SE) follows a structured, time-dependent approach often referred to as a "SE protocol."
The goal is to terminate seizure activity as quickly as possible, identify and treat the underlying cause, and prevent complications.
- Recognize SE: Seizure lasting > 5 minutes or recurrent seizures without regaining consciousness.
- Ensure Safety: Protect the patient from injury.
- ABCs: Airway, Breathing, Circulation – immediate priorities.
- Establish IV Access: Crucial for medication administration.
- Initial Monitoring: Vital signs, SpO2, cardiac rhythm.
- STAT Glucose Check: Treat hypoglycemia if present.
- Administer rapid-acting benzodiazepines.
- If seizures persist, initiate non-benzodiazepine antiseizure drugs (ASDs).
- If seizures continue, consider continuous EEG and transfer to ICU for aggressive third-line therapies (general anesthesia).
- Safety and Positioning:
- Move patient to a safe environment if possible.
- Protect head and extremities. Do NOT restrain. Do NOT insert anything into the mouth.
- Turn patient to the side (recovery position) to prevent aspiration if vomiting occurs.
- Airway Management:
- Assess airway patency. Clear secretions.
- Provide supplemental oxygen (e.g., non-rebreather mask at 10-15 L/min).
- Prepare for intubation if airway is compromised, respiratory depression occurs, or prolonged SE is anticipated.
- Breathing:
- Monitor respiratory rate and effort. Assess for hypoventilation or apnea.
- Bag-valve-mask (BVM) ventilation if needed.
- Circulation:
- Monitor heart rate, blood pressure, cardiac rhythm. Treat hypotension/hypertension as appropriate.
- Establish 2 large-bore IVs immediately.
- Rapid Assessment & Investigations:
- STAT Finger-stick Glucose: Administer 50 mL of D50W (dextrose 50%) IV if hypoglycemic (e.g., < 60 mg/dL). In children, give D25W (2-4 mL/kg) or D10W.
- Collect Blood Samples: For electrolytes, CBC, LFTs, renal function, toxicology, AED levels, ABG, lactate, CK.
- Lorazepam (Ativan): 0.1 mg/kg IV (max 4 mg) infused over 2-5 minutes. Can be repeated once in 5-10 minutes if seizures persist. Preferred IV benzodiazepine due to longer duration of action compared to diazepam.
- Diazepam (Valium): 0.15-0.2 mg/kg IV (max 10 mg) at 5 mg/min. Can be repeated once. Shorter duration of action than lorazepam, so often followed by a longer-acting AED.
- Midazolam (Versed): 0.2 mg/kg IM (max 10 mg) or intranasal/buccal (0.2-0.5 mg/kg, max 10 mg). Useful in pre-hospital or when IV access is not yet established.
- Levetiracetam (Keppra): 1000-3000 mg IV (typically 20-60 mg/kg, max 4500 mg) infused over 10-20 minutes. Minimal drug interactions, generally well-tolerated.
- Fosphenytoin (Cerebyx): 15-20 mg PE (phenytoin equivalents)/kg IV at 100-150 mg PE/min. Prodrug converted to phenytoin. Less risk of local irritation and hypotension than phenytoin.
- Valproate Sodium (Depakote): 20-40 mg/kg IV infused over 15-30 minutes. Contraindicated in liver disease or urea cycle disorders.
- Lacosamide (Vimpat): 200-400 mg IV infused over 15-30 minutes.
- Midazolam (Versed): Continuous IV infusion, titrate to EEG burst suppression.
- Propofol (Diprivan): Continuous IV infusion, titrate to EEG burst suppression. Requires intubation and mechanical ventilation due to profound respiratory depression. Risk of Propofol Infusion Syndrome with prolonged high doses.
- Pentobarbital/Phenobarbital: Continuous IV infusion, titrate to EEG burst suppression. Long half-life, significant hypotension, respiratory depression, and prolonged sedation.
- SE that continues for 24 hours or more after starting anesthetic therapy, or recurs after anesthetic withdrawal.
- Management often involves further escalation of therapies, including ketamine, inhaled anesthetics, therapeutic hypothermia, immunotherapy (for suspected autoimmune causes), ketogenic diet, magnesium, or even surgical interventions (e.g., vagal nerve stimulator, resective surgery) in specific cases.
- Hyperthermia: Cooling blankets, antipyretics.
- Rhabdomyolysis/AKI: Aggressive IV fluids, monitor renal function.
- Aspiration Pneumonia: Antibiotics if indicated.
- Metabolic Acidosis: Correct underlying cause, consider bicarbonate (rarely needed).
- Cerebral Edema: Osmotic agents (mannitol, hypertonic saline) if indicated.
- Risk for Ineffective Airway Clearance related to decreased level of consciousness, excessive secretions, tongue obstruction, and inability to clear airway as evidenced by noisy breathing, gurgling, snoring, or cyanosis.
- Risk for Ineffective Breathing Pattern related to neuromuscular impairment, central nervous system depression from seizure activity and/or antiepileptic medications, as evidenced by bradypnea, tachypnea, irregular breathing, shallow respirations, or apnea.
- Risk for Injury (Physical Trauma) related to uncontrolled motor activity during seizure, falls, or environmental hazards, as evidenced by potential for head trauma, lacerations, fractures, or aspiration.
- Risk for Decreased Cardiac Output related to altered electrical activity of the heart, increased metabolic demands, and/or adverse effects of antiepileptic medications, as evidenced by tachycardia, bradycardia, hypotension, or arrhythmias.
- Risk for Inadequate Fluid Volume related to hyperthermia, inadequate oral intake, increased metabolic rate, and medication effects, as evidenced by altered skin turgor, dry mucous membranes, changes in urine output, or electrolyte imbalances.
- Acute Confusion / Impaired Thought Processes related to ongoing seizure activity, postictal state, cerebral edema, and/or adverse effects of medications, as evidenced by disorientation, altered attention span, memory deficits, or impaired decision-making.
- Risk for Ineffective Cerebral Tissue Perfusion related to cerebral edema, increased intracranial pressure, systemic hypotension, or prolonged cerebral vasoconstriction, as evidenced by changes in neurological status, pupillary response, or motor function.
- Hyperthermia related to increased metabolic rate, sustained muscular activity, and hypothalamic dysfunction, as evidenced by elevated body temperature.
- Risk for Inadequate protein energy nutritional intake related to hypermetabolic state, decreased level of consciousness, and prolonged NPO status, as evidenced by potential for weight loss, muscle wasting, or inadequate caloric intake.
- Risk for Impaired Skin Integrity related to immobility, incontinence, hyperthermia, and prolonged pressure, as evidenced by potential for pressure ulcers, rashes, or skin breakdown.
- Excessive Anxiety (Patient/Family) related to the life-threatening nature of the condition, uncertain prognosis, lack of control, and complex medical environment, as evidenced by expressed concerns, restlessness, agitation, or questions about care.
Nursing interventions for a patient with Status Epilepticus (SE) are immediate, systematic, and continuous, reflecting the urgency and complexity of the condition..
- Stay calm and speak calmly if you are to give instructions or when reassuring bystanders
- Remove the person from danger or vice versa if the patient is safe, don’t move them.
- Note the time the seizure starts and continue checking if it does not stop in 5 minutes, call for an ambulance.
- Loosen ties, necklaces or any cloth around the neck that may make it hard to breathe
- Support the head with a soft flat material under like a folded jacket so as to protect it from injury during jerking
- Clear space to and minimise any form of crowdness such that the patient receives fresh air.
- As soon as the fit stops, Make the patient lie down in a lateral position so as to ensure he does not choke on his own saliva
- Check that breathing is returning to normal if their breathing sounds difficult after the seizure has stopped call for an ambulance
- Check gently to see that nothing is blocking their airway such as false teeth.
- Stay with the patient until when the patient is fully awake
- After recovery, reorient the patient and reassure incase he is embarrassed
- Positioning: Turn patient to the side (recovery position) to prevent aspiration and allow secretions to drain.
- Suctioning: Have suction readily available and clear the airway of secretions, vomit, or blood as needed.
- Oxygen Administration: Apply high-flow oxygen (e.g., non-rebreather mask at 10-15 L/min) immediately.
- Airway Adjuncts: Insert a nasopharyngeal or oropharyngeal airway if feasible and tolerated, but never force anything into the mouth during a tonic-clonic seizure.
- Prepare for Intubation: Have intubation equipment (laryngoscope, endotracheal tubes, Ambu bag, suction) at the bedside, anticipating the need for advanced airway management if respiratory compromise occurs or prolonged SE develops.
- Environmental Safety: Pad side rails, remove restrictive clothing, move furniture or objects away from the patient.
- Protection during Seizure: Gently support the head; do not restrain limbs during convulsive activity.
- Monitoring Environment: Maintain constant observation, either directly or via continuous monitoring.
- IV Access: Insert two large-bore IV catheters immediately for rapid fluid and medication administration.
- First-Line Medications: Administer prescribed benzodiazepines (e.g., lorazepam IV, diazepam IV/PR, midazolam IM/intranasal/buccal) as ordered, observing for therapeutic effects and adverse reactions (especially respiratory depression).
- Second-Line Medications: Prepare and administer prescribed non-benzodiazepine Antiepileptic Drugs (ASDs) if SE persists.
- Document: Meticulously record medication administration times, dosages, and patient response.
- Vital Signs: Continuous cardiac monitoring, pulse oximetry, blood pressure, and respiratory rate/effort.
- Neurological Assessment: Frequent assessment of level of consciousness (GCS), pupillary response, and motor activity.
- Seizure Activity: Document onset, duration, type of seizure, and any progression. Note exact start/end times.
- Capillary Blood Glucose: Perform STAT blood glucose check and administer D50W if hypoglycemic.
- Collect Blood for Labs: Obtain blood samples for all ordered labs (electrolytes, CBC, AED levels, toxicology, etc.).
- Continuous EEG (cEEG): Facilitate and monitor cEEG in collaboration with neurology, especially for suspected Non-Convulsive SE (NCSE) or Refractory SE (RSE). Ensure electrodes remain intact and alerts are promptly addressed.
- Serial Neurological Assessments: Continue frequent assessments to detect subtle changes in mental status, new focal deficits, or recurrence of seizure activity.
- Monitor Temperature: Regularly assess core body temperature.
- Manage Hyperthermia: Implement cooling measures if hyperthermic (e.g., antipyretics, cooling blankets, removal of excess clothing).
- IV Fluids: Administer IV fluids as prescribed to maintain hydration and electrolyte balance.
- Monitor I&O: Accurately record intake and output.
- Monitor Labs: Review daily electrolyte and renal function labs and notify provider of abnormalities.
- Pressure Injury Prevention: Implement a turning schedule (every 2 hours), use pressure-relieving devices (specialty mattresses), and maintain meticulous skin hygiene.
- Range of Motion: Perform passive range of motion exercises to prevent contractures once stable.
- DVT Prophylaxis: Apply sequential compression devices (SCDs) or administer subcutaneous heparin/LMWH as prescribed.
- Gastric Protection: Administer stress ulcer prophylaxis (e.g., proton pump inhibitors) as ordered.
- Nutrition: Once stable and seizure-free, assess readiness for oral intake. If prolonged NPO, anticipate need for enteral or parenteral nutrition.
- Patient: Provide reorientation and calm reassurance once consciousness returns.
- Family: Provide clear, concise, and frequent updates to family members. Allow family presence at the bedside as appropriate. Offer emotional support, address concerns, and explain procedures. Refer to social work or spiritual care as needed.
- Maintain thorough and accurate documentation of all assessments, interventions, medication administration, patient responses, and communication with the healthcare team. This is crucial for continuity of care and legal purposes.
- Disease Process: Explain SE, its causes, and management.
- Medications: Review prescribed ASDs, dosage, administration, side effects, and importance of adherence.
- Seizure Precautions: Discuss safety measures for future seizures.
- Follow-up Care: Emphasize the importance of neurology follow-up.
- When to Seek Emergency Care: Review signs and symptoms that warrant immediate medical attention.
The following should be taught to the patient and the community at large
- Status epilepticus is an illness just like any other illness and on treatment a person gets better
- People with status epilepticus should be encouraged to enjoy as much as possible
- Isolating, stigmatizing and labelling an epileptic patient is very traumatizing to the patient, family and clan members so they should be avoided
- Children with status epilepticus are encouraged to attend school
- Teachers, school children and other school personnel should be educated about the illness so that they are enlightened
- Adults with status epilepticus can marry and should be encouraged to do so
- Persons with epilepsy should avoid dangerous activities such as driving, climbing height, operating heavy machines, swimming
- People have to be taught that Status epilepticus is not contagious so patients should be treated fairly like other people
- Epileptic seizures can effectively be controlled if drugs are taken as prescribed.
- The person has never had a seizure before
- The person has difficulty breathing or walking after the seizure
- The seizure lasts longer than 5 minutes
- The person has another seizure soon after the first one
- The person is hurt during the seizure
- The seizure happens in water
- The person has a health condition like diabetes, heart disease or is pregnant
- Prevent head injury by wearing seat belts and bicycle helmets.
- Seek medical help Immediately after suffering a first seizure.
- Mothers should be encouraged to get good prenatal care to prevent brain damage to a developing fetus
- Treatment of hypertension
- Avoid excess alcohol abuse and alcohol intake
- Treating high fevers in children
- Treatment of any infections and proper nutrition including adequate vitamin intake

I love this work 👊👊
Good notes but am requesting for the specific nursing interventions for a patient with status epilepticus
Added
Thx for the good work
Good Waka so far but Nursing diagnosis missing….. otherwise am happy for the Waka and it’s helping me
So palatable
Very good book