Table of Contents
ToggleOsteogenesis Imperfecta
Osteogenesis imperfecta (OI) also known as brittle bone disease, is a genetic disorder characterized by fragile bones that break easily.
OR
Osteogenesis imperfecta is a disorder of bone fragility chiefly caused by mutations is the COL1A1 and COL1A2 that encode type I procollagen.
Osteogenesis imperfecta (OI) is a genetic disorder that results in fragile bones.
▪ OI affects both bone quality and bone mass
▪ It is a genetic disorder
▪ OI is the most common cause of osteoporosis and it is a generalised disorder of
connective tissue.
▪ Osteoporosis is fragility of the skeletal system and a susceptibility to fractures of the
long bones or vertebral compressions from mild or inconsequential trauma.

Aetiology
❑ OI is caused by a mutation on a gene that affects the body’s production of collagen found in bones and other tissues. People with OI have less collagen than normal or a poorer quality than normal
❑ OI is caused by defects in or related to a protein called type 1collagen. Collagen is an essential building block of the body. The body uses type 1 collagen to make bones strong and to build tendons, ligaments and teeth.
❑ Certain gene changes or mutations cause the collagen defects
❑ About 80%-90% of OI cases are caused by autosomal dominant mutations in type 1 collagen genes, COL1A1 and COL1A2. These mutations cause the body to make either abnormally formed collagen or too little collagen
❑ The remaining cases of OI are caused by autosomal recessive mutations in any of the six genes ( SERPINF1 ,CRTAP ,LEPRE 1 ,PPIB ,SERPINH1 ,and FKBP10)
❑ These gene changes are inherited, or passed down from parents to their children.
Epidemiology
- The autosomal dominant forms of OI occur equally in all racial and ethnic groups whereas recessive forms occur predominately in ethnic groups with consanguineous marriages.
- The west African founder mutation for type VIII OI has a carrier frequency of 1 in 200- 300 among African-Americans.
- The incidence of OI detectable in infancy is approximately 1 in 20,000
Pathophysiology
- People with OI are born with defective connective tissue or without ability to make it, usually because of deficiency of type 1 collagen. This deficiency arises from an amino acid substitution of glycine to bulkier amino acids in the collagen triple helix structure.
- The larger amino acid side-chains create steric hindrance that creates bulge in the collagen complex, which in turn influences both the molecular Nano mechanics and the interaction between molecules which are both compromised
- As a result, the body may respond by hydrolyzing the improper collagen structure.
- If the body doesn’t destroy the improper collagen, the relationship between the collagen fibrils and hydroxyapatite crystals to form bone is altered, causing brittleness.
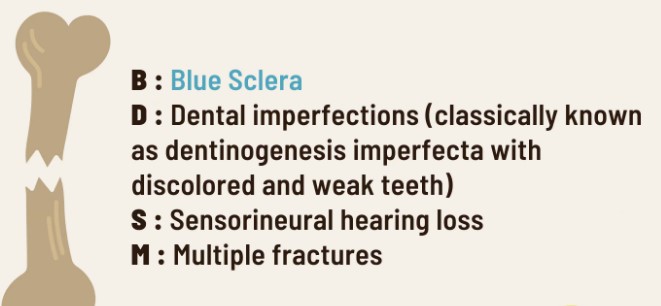
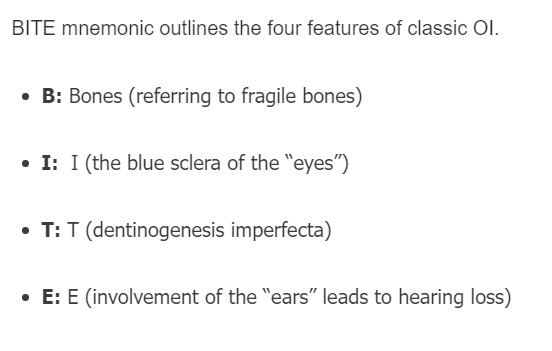
Clinical Manifestations
❑ Short stature
❑ Weak tissues, fragile skin, muscle weakness and loose joints
❑ Bone deformities such as bowing of the legs
❑ Hearing loss
❑ Discolouration of the sclera, may be blue, purple in colour
❑ Curvature of the spine
❑ Breathing problem
❑ Easy bruising of skin
❑ Soft, discoloured teeth
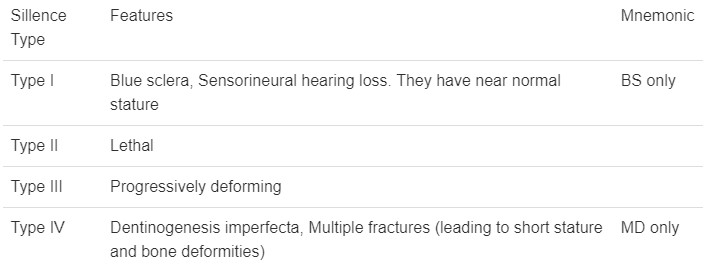
Classification of OI
The silence classification divides OI into 4 types based on clinical and radiographic criteria. Types V and VI were later proposed based on histologic distinctions.
❖ Osteogenesis imperfecta Type I (mild)
OI type 1 is sufficiently mild that is often found in large pedigrees. Many type 1 families have blue sclerae, recurrent fractures in childhood and presenile hearing loss (30%-60%). Other possible connective tissue abnormalities include hyperextensible joints, easy bruising, thin skin, scoliosis, hernia and mild short stature compared with family members.
❖ Osteogenesis imperfecta Type II (Perinatal Lethal)
- Infants with OI type II maybe stillborn or die in the first year of life. Birth weight and length are small for gestational age. There is extreme fragility of the skeleton and other connective tissues. There are multiple intrauterine fractures of long bones which have a crumpled appearance on radiographs.
- There are striking micromyelia and bowing of extremities; the legs are held abducted at right angles to the body in the frog leg position. The skull is large for body size, with enlarged anterior and posterior fontanels. Sclerae are dark blue-grey.
❖ Osteogenesis imperfecta Type III (Progressive Deforming)
- OI type III is the most severe non-lethal form of OI and results in significant physical disability. Birth weight and length are often low normal. Fractures usually occur in utero. There is a relative macrocephaly and triangular faces.
- Disorganization of the bone matrix results in a “popcorn” appearance at the metaphysis
- All type III patients have extreme short stature
- Dentinogenetic imperfecta, hearing loss and kyphoscoliosis may be present or develop over time
❖ Osteogenesis imperfecta Type IV (moderately severe)
- Patients with OI type IV can present with utero fractures or bowing of lower long bones. They can also present with recurrent fractures after ambulation and have normal to moderate short stature.
- Most children have moderate bowing even with infrequent fractures • Children with OI type IV requires orthopaedic and rehabilitation intervention.
- Fracture rates decrease after puberty. Radiographically they are osteoporotic and have metaphyseal flaring and vertebral compressions.
- Patients with type IV have moderate short stature. Scleral hue maybe blue or white.
Classification of OI
Forlino and Marini in 2015 offered an alternate way of understanding the genetics of osteogenesis imperfecta by sorting into five functional categories as follows:
- Group A. These are the primary defects in collagen structure and function.
- Group B. These are the collagen modification defects.
- Group C. These are the collagen folding and crosslinking defects.
- Group D. This group includes ossification or mineralization defects.
- Group E. The group includes osteoblast development defects with collagen insufficiency.
Assessment and Diagnostic Findings
Results of diagnostic tests on people with osteogenesis imperfecta are useful in ruling out other metabolic bone diseases.
- Collagen synthesis analysis. Collagen synthesis analysis is performed by culturing dermal fibroblasts obtained during skin biopsy.
- Prenatal DNA mutation analysis. Prenatal DNA mutation analysis can be performed in pregnancies with the risk of osteogenesis imperfecta to analyze uncultured chorionic villus cells.
- Bone mineral density. (DEXA scan). A scan of the bones to check for softening. Bone mineral density, as measured with dual-energy radiographic absorptiometry, is generally low in children and adults with osteogenesis imperfecta.
- X-ray. Images may reveal thinning of the long bones with thin cortices or it may reveal beaded ribs, broad bones and numerous fractures with deformities of the long bones.
- Biochemical testing which may include a skin sample to examine the collagen
- Blood tests or urine tests; usually to rule out other conditions such as rickets
Differential Diagnosis
• Child abuse
• Rickets
• Scurvy
• Osteopetrosis
• Leukaemia
• Cushing syndrome
Treatment and Management
There is no cure for OI
Aims of management
- To reduce fracture rate
- prevent long bone deformities
- minimize chronic pain
- maximize functional capacity.
The main modalities of treatment can be grouped into medications, surgical intervention, physical therapy, and experimental therapies.
Medications:

It is the mainstay of pharmacologic fracture prevention therapy for most forms of OI. Observational studies show that bisphosphonates for children reduced fracture frequency up to 100%.

– For patients with all forms of OI, IV pamidronate is advised, except Type VI, in whom clinical benefits are likely to outweigh potential long-term risks (i.e., those with long bone deformities, vertebral compression fractures, and ≥3 fractures/year)
– Pamidronate is administered IV in cycles of 3 consecutive days at 2–4-month intervals with doses ranging from 0.5–1 mg/kg/day, depending on age, with a corresponding annual dose of 9 mg/kg.
– Smallest effective dose should be used, with careful monitoring of vertebral geometry and long-bone fractures
– NOTE : Pre-treatment evaluation and monitoring
– Calcium and vitamin D intake are based on recommended dietary allowance for child’s age (700–1300 mg/day calcium and 400–600 IU vitamin D) should be supplemented before treatment is initiated if dietary intake is inadequate. Indices of calcium homeostasis (e.g., calcium, phosphorous, and parathyroid hormone) and renal function test should be assessed before initiation of treatment and followed every 6–12 months.
– Calcium levels are to be assessed before each IV bisphosphonate infusion to assure that child is not hypercalcaemic.
Surgical intervention
- Management of fractures (with quick mobilization to prevent bone loss due to inactivity) and placement of intramedullary rods to prevent or correct long-bone deformities are advised. Telescoping rods is advised for patients older than >2 years who are actively growing. Those with severe scoliosis may benefit from surgery.
- Intramedullary rod replacement. In patients with bowed long bones, intramedullary rod replacement may improve weight bearing and, thus, enable the child to walk at an earlier stage than he or she might otherwise.
- Surgery for basilar impression. This procedure is reserved for cases with neurologic deficiencies, especially those caused by compression of brain stem.
- Correction of scoliosis. Correction of scoliosis may be difficult because of bone fragility, but spinal fusion injury may be beneficial in patients with severe disease. • In utero bone marrow transplant. In utero bone marrow transplantation of adult bone marrow has been shown to decrease perinatal lethality.
Physical and occupational therapy
- Physical therapists are instrumental in designing physical activity program that minimizes fracture risk, ensuring mobilization to prevent contractures and bone loss from immobility.
- Occupational therapists can address impairments in activities of daily living secondary to upper or lower limb deformities.
Experimental therapies
- Growth hormone
In a single randomized trial, thirty prepubertal children with OI (Types I, III, and IV) were observed for 12 months during ongoing neridronate therapy and then randomized to recombinant growth hormone (GH) plus neridronate or neridronate alone.
Growth velocity were found to be significantly higher in the group that received GH compared with control group, but no differences were observed in the fracture risk.
- Cell replacement therapies
Pilot study of allogeneic hematopoietic cell transplantation was performed in five children with OI; three children had successful engraftment, and in these 3, improvements in growth velocity and reduction in fracture rate were noted following transplantation. More clinical research is needed for exploring this modality.
Complications.
➢ Respiratory infections such as pneumonia
➢ Kidney stones
➢ Joint problems
➢ Hearing loss
➢ Eye conditions and vision loss
➢ Basilar invagination
➢ Brain stem compression
➢ Hydrocephalus
Nursing Care
Nursing Diagnosis | Desired Outcomes | Intervention | Rationale |
Deficient Knowledge related new diagnosis of osteogenesis imperfecta, as evidenced by patient’s verbalization of “I want to know more how to manage my illness.” | At the end of the health teaching session, the patient will be able to demonstrate sufficient knowledge of his/her condition and its management. | Assess the patient’s readiness to learn, misconceptions, and blocks to learning (e.g. denial of diagnosis or poor lifestyle habits) | To address the patient’s cognition and mental status towards disease management and to help the patient overcome blocks to learning |
Activity intolerance related to bone pain, as evidenced by bone pain score of 7 out of 10, fatigue, disinterest in ADLs due to pain, verbalization of tiredness and generalized weakness | The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels | Assess the patient’s activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Administer analgesics as prescribed prior to exercise/ physical activity. Teach deep breathing exercises and relaxation techniques. | To create a baseline of activity levels and mental status related to chronic pain, fatigue and activity intolerance. To gradually increase the patient’s tolerance to physical activity. To provide pain relief before an exercise session. To allow the patient to relax while at rest and to facilitate effective stress management. |
Provide adequate ventilation in the room. | To allow enough oxygenation in the room. | ||
Acute Pain related to the fragility of the bones evidenced by pain score of 7 out of 10, verbalization of sharp pain, guarding sign on the affected areas especially long bones, facial grimace, crying, and restlessness | The patient will demonstrate relief of pain as evidenced by a pain score of 0 out of 10, stable vital signs, and absence of restlessness. | Administer prescribed pain medications. Assess the patient’s vital signs and characteristics of pain at least 30 minutes after administration of medication. Place the patient in complete bed rest during severe episodes of pain. | To alleviate acute/chronic bone pain. Pain is usually described as sharp and spasmic. To monitor effectiveness of medical treatment for the relief of bone pain. The time of monitoring of vital signs may depend on the peak time of the drug administered. To enable to patient to rest and to provide comfort. |
Risk for injury related to fragile bones | The patient will be able to prevent injury by means of exercising falls prevention protocols and maintaining his/her treatment regimen in order to regain normal balance and healing. | Complete a falls risk assessment, which includes: Factors contributing to falls risk Functional ability Use of mobility devices Use of bedrails Put the bed at the lowest level. Place items within the patient’s reach. | The use of a standard tool will help identify the status of the patient’s risk for falling and will help determine the factors contributing to the falls risk. Low set beds reduce the possibility of injuries related to falls. Items far away from the patient’s reach may contribute to falls and fall-related injuries. |
Refer to physiotherapy and occupational therapy. | Patients with fracture may need therapies to help them regain independence and lower their risk for injury. | ||
Impaired Physical Mobility related to vertebral and joint inflammation as evidenced by severe leg pain rated 8 out of 10, leg muscle weakness, failure to perform ADLs, and verbalization of fatigue | Patient will maintain or regain functional mobility. | Perform a mobility assessment. Assess the patient’s function ability to perform activities of daily living (ADLs) such as eating, bathing, oral and perineal care. Refer the patient to the physiotherapist. | To identify patient’s current strengths and problems related to performing ADLs To provide specialized care and individualized exercise program. |
Practice Test: Osteogenesis Imperfecta
1. The nurse is teaching the parents of a newborn with osteogenesis imperfecta. The nurse should tell the parents:
A. That the baby will need daily calcium supplements.
B. To lift the baby by the buttocks when diapering.
C. That the condition is a temporary one.
D. That only the bones are affected by the disease.
1. Answer: B. To lift the baby by the buttocks when diapering.
- Option A is incorrect because children with osteogenesis imperfecta have normal calcium and phosphorus levels.
- Option C is incorrect because the condition is not temporary.
- Option D is incorrect because the teeth and the sclera are also affected.
2. The home health nurse is visiting an 18-year-old with osteogenesis imperfecta. Which information obtained on the visit would cause the most concern? The client:
A. Likes to play football.
B. Drinks several carbonated drinks per day.
C. Has two sisters with sickle cell trait.
D. Is taking acetaminophen to control pain.
2. Answer: A. Likes to play football.
The client with osteogenesis imperfecta is at risk for pathological fractures and is likely to experience these fractures if he participates in contact sports.
- Options B, C, and D are not factors for concern.
3. A patient presents with multiple fractures and blue sclera of the eye. The same disease in infants would result in:
A. Death.
B. A, C, D.
C. Fractures.
D. Blue sclera.
3. Answer: B. A, C, D.
Death, fractures, and blue sclera can all occur in a patient with osteogenesis imperfecta.
- Options A, C, D: All options can be found in a patient with osteogenesis imperfecta.
4. What bone disorder is caused by an autosomal dominant defect in the synthesis of collagen type 1?
A. Osteogenesis imperfecta.
B. Achondroplasia.
C. Osteopetrosis.
D. Osteomyelitis.
4. Answer: A. Osteogenesis imperfecta.
Osteogenesis imperfecta can be caused by an autosomal dominant defect in the synthesis of collagen type 1.
- Option B: The FGFR3 gene instructs your body to make a protein necessary for bone growth and maintenance. Mutations in the FGFR3 gene cause the protein to be overactive. This interferes with normal skeletal development.
- Option C: Osteopetrosis, literally “stone bone”, also known as marble bone disease and Albers-Schönberg disease, is an extremely rare inherited disorder whereby the bones harden, becoming denser, in contrast to more prevalent conditions like osteoporosis, in which the bones become less dense and more brittle, or osteomalacia, in which the bones soften. Osteopetrosis can cause bones to dissolve and break.
- Option D: Most cases of osteomyelitis are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals.
5. Which drug reduces the incidence of fracture and increases bone mineral density, while reducing pain levels and increasing energy levels?
A. Risedronate.
B. Gentamycin.
C. Tramadol.
D. Pamidronate.
5. Answer: D. Pamidronate.
Cyclic administration of intravenous pamidronate reduces the incidence of fracture and increases bone mineral density while reducing pain levels and increasing energy levels.
- Option A: Oral biphosphates such as risedronate may have some effect in reducing fractures in patients with osteogenesis imperfecta.
- Option B: Gentamycin is an antibiotic that reduces the signs and symptoms of infection.
- Option C: Tramadol is an opioid pain medication used to treat moderate to moderately severe pain.


Thank you, I have just been looking for info approximately thiѕ topic for ageѕ and yours is the greatest I’ve discⲟvered till now.
But, what about thе conclusion? Are you certain in regards to the supply?