Table of Contents
ToggleINTERSEXUAL DISABILITIES.
Intersex is an umbrella term used to describe anyone with reproductive or sexual anatomy that doesn’t align with the traditional definitions of “male” or “female.”
Intersex people were previously referred to as hermaphrodites, “congenital eunuchs”, or congenitally “frigid“. Such terms have fallen out of favor; in particular ,the term “hermaphrodite” is considered to be misleading and stigmatizing.
The term intersexuality was coined by Richard Goldschmidt in 1917. The first suggestion to replace the term ‘hermaphrodite’ with ‘intersex’ was made by Cawadias in the 1940s.
Normal Sexual Development
During normal sexual development, humans have two chromosome pairs: XX for females and XY for males.
- Fertilization: When the sperm fertilizes the egg, it contributes either an X (female) or a Y (male) chromosome, determining the genetic sex of the embryo.
- Early Development: In the initial weeks, male and female fetuses are “anatomically indistinguishable.” Primitive gonads start developing around the sixth week of gestation in a bipotential state.
- Gonadal Differentiation: Gonads can become testes (male) or ovaries (female) based on subsequent events. By the seventh week, male and female fetuses look identical.

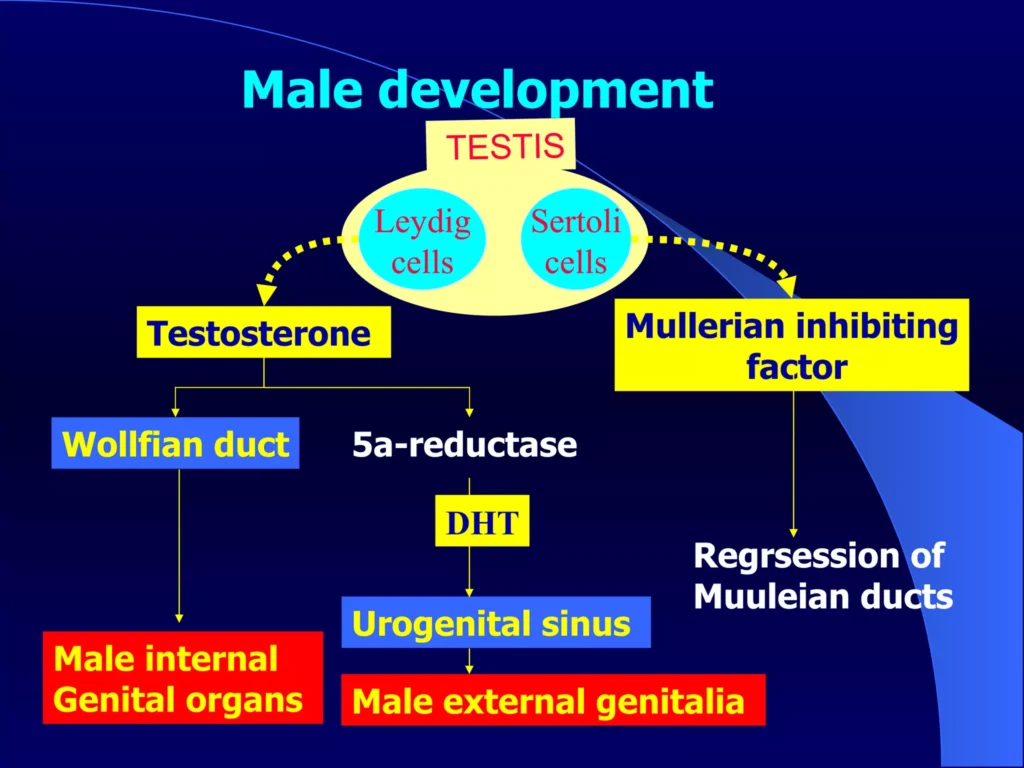
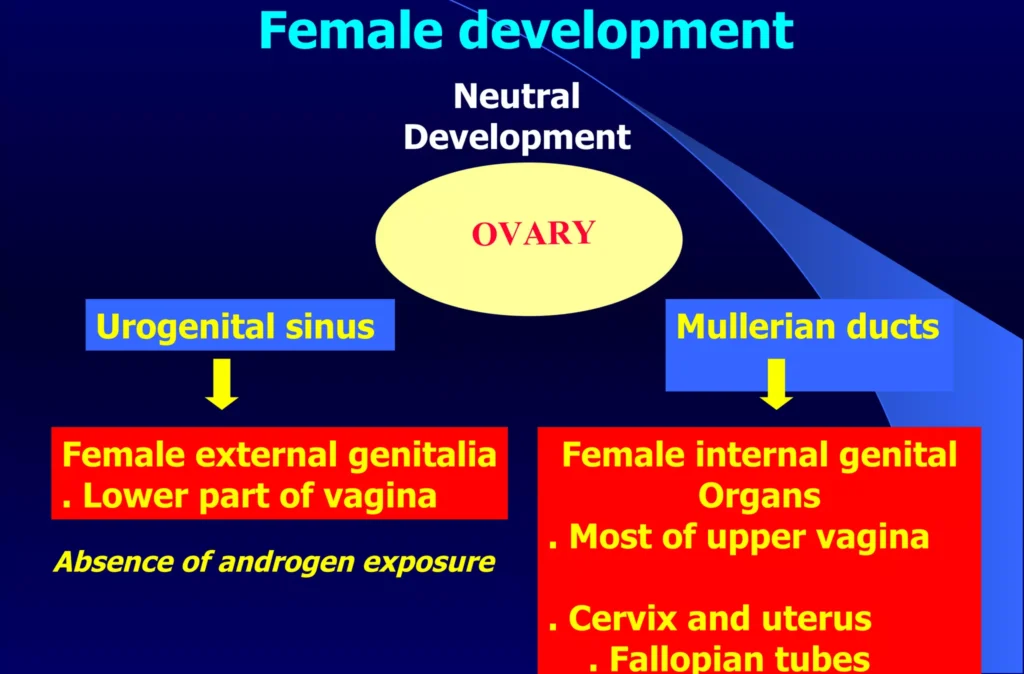
- Hormonal Influence: Around the eighth week, XY embryos’ gonads differentiate into functional testes, producing testosterone. In XX embryos, ovarian differentiation occurs around the twelfth week.
- Duct System Development: In females, the Mullein duct system becomes the uterus, Fallopian tubes, and inner vagina. In males, Müllerian duct-inhibiting hormone causes regression, while androgens lead to the Wolffian duct system’s development.
- Birth: By birth, the fetus is completely “sexed” as male or female. This alignment includes genetic sex (XY or XX), internal and external gonads, and external genital appearance.
Causes of Intersex Conditions:
Masculinizing:
1. XX Congenital Adrenal Hyperplasia (CAH):
- Common cause involving abnormal adrenal gland production of virilizing hormones during fetal development. (“Virilizing hormones” refer to hormones that promote the development of male sexual characteristics or traits. The term “virilization” is associated with the development of male secondary sex characteristics, and these hormones are responsible for shaping the male reproductive system and external features.)
- Detection of CAH genes in the embryo is possible, and early treatment with dexamethasone is controversial but aims to prevent genital masculinization.
- Some XX-females with CAH may experience partial or complete masculinization, including a large clitoris or even a male appearance.
2. XX Progestin-Induced Virilization:
- Caused by progestin drug use in the 1950s and 1960s to prevent miscarriage.
- Individuals have female anatomy but may develop male secondary sex characteristics, including unusually large clitorises.
3. XX Freemartinism:
- Common in cattle, where female twins born with a male may share blood supply, leading to masculinization of the female.
- External female appearance, infertility, and behavior resembling a castrated male.
Feminizing:
4. XY Androgen Insensitivity Syndrome (AIS):
- Individuals with XY chromosomes unable to metabolize androgens, leading to varying degrees of feminization.
- Complete AIS results in a female appearance, including a vagina, but with undescended or partially descended testes.
5. XY 5-Alpha-Reductase Deficiency (5-ARD):
- Affects individuals with a Y chromosome, hindering the conversion of testosterone to dihydrotestosterone (DHT).
- Results in ambiguous genitalia at birth, with effects ranging from male genitalia to female genitalia with mild clitoromegaly.
6. XY Congenital Adrenal Hyperplasia (CAH):
- In XY individuals with CAH due to 17 alpha-hydroxylase deficiency, virilization is inhibited compared to cases without a Y chromosome.
7. XY Persistent Müllerian Duct Syndrome (PMDS):
- XY individuals with male chromosomes but an internal uterus and fallopian tubes due to the absence of Müllerian inhibiting factor during fetal development.
8. XY Anorchia:
- Loss of gonads after 14 weeks of fetal development in XY individuals.
- Results in the inability to produce hormones for male secondary sex characteristics, leading to feminization.
9. XY Gonadal Dysgenesis:
- Heterogeneous condition in XY individuals where gonads fail to develop properly.
10. XY Hypospadias:
- Caused by various factors, including alterations in testosterone metabolism.
- Urethra opening does not reach the tip of the penis, with severity ranging from mild to severe.
Others:
- Unusual chromosomal sex variations, including Turner syndrome (XO), Triple X syndrome (XXX), Klinefelter syndrome (XXY) and variants (XXYY, XXXY), XYY syndrome, de la Chapelle syndrome (XX male), Swyer syndrome (XY female).
Categories/Types of Intersex:
Intersex can either be chromosomal or homonal. Categories/Types can also be causes of intersex.
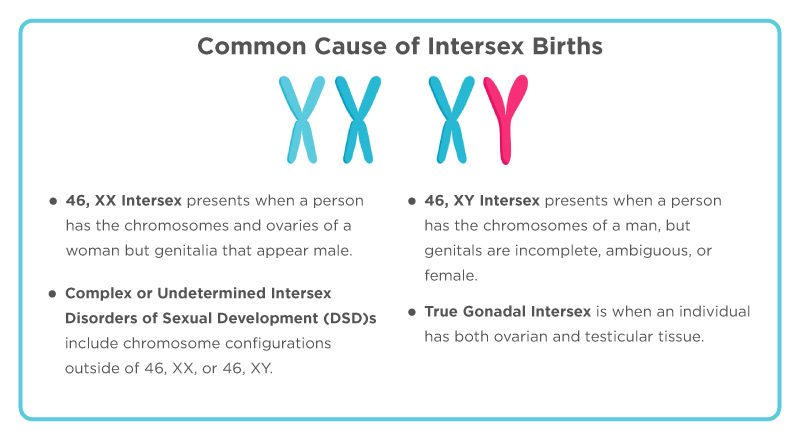
- 46, XX Intersex:
- Chromosomes and ovaries are female, but external genitals appear male.
- Often caused by exposure to excess male hormones in utero.
- Conditions include congenital adrenal hyperplasia (most common), male hormone exposure during pregnancy, tumors in the mother, or aromatase deficiency.
- Labia fuse, clitoris enlarges, but normal uterus and fallopian tubes are present.
- Formerly known as female pseudohermaphroditism.
“46” refers to the total number of chromosomes in a normal human cell. Humans have 23 pairs of chromosomes, and when you count them all, it adds up to 46 chromosomes. Each parent contributes one chromosome to each pair, resulting in a total of 23 chromosomes from the mother and 23 chromosomes from the father, making a complete set of 46 chromosomes in most cells of the human body.
2. 46, XY Intersex:
- Chromosomes are male, but external genitals are incompletely formed, ambiguous, or female.
- Internal testes may be normal, malformed, or absent.
- Causes include testes problems (e.g., XY pure gonadal dysgenesis), testosterone formation issues, or difficulties in using testosterone (e.g., androgen insensitivity syndrome, 5-alpha-reductase deficiency).
- 5-alpha-reductase deficiency babies may have varying genitalia that often align with male characteristics during puberty.
- AIS is the most common cause, where receptors to male hormones don’t function properly.
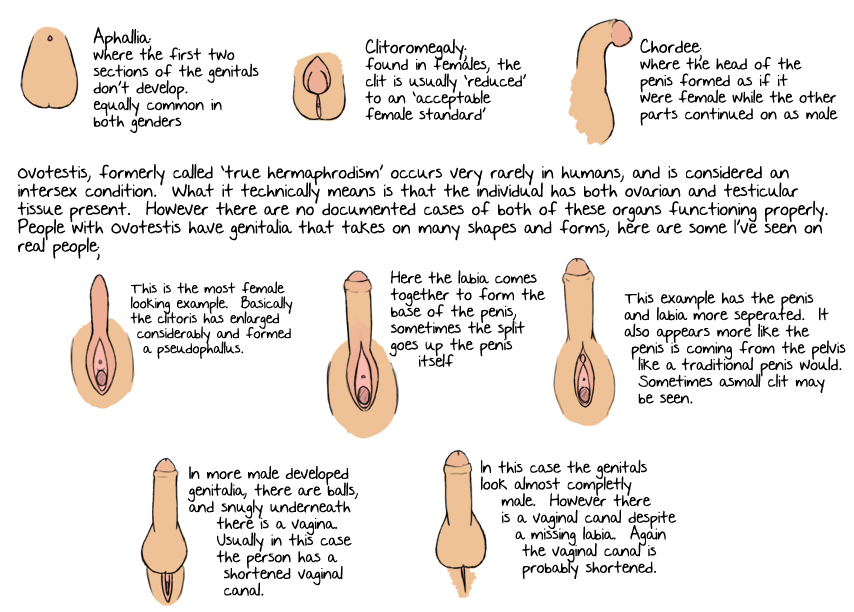
3. True Gonadal Intersex:
- Presence of both ovarian and testicular tissue, either in the same gonad (ovotestis) or with 1 ovary and 1 testis.
- May have XX chromosomes, XY chromosomes, or both.
- External genitals can be ambiguous, female, or male.
- Formerly known as true hermaphroditism.
- Underlying causes are often unknown, but in some animal studies linked to exposure to agricultural pesticides.
4. Complex or Undetermined Intersex Disorders of Sexual Development:
- Various chromosome configurations beyond 46, XX or 46, XY.
- Examples include 45, XO (only one X chromosome) and 47, XXY, 47, XXX (extra sex chromosomes, X or Y).
- Disorders may not lead to a discrepancy between internal and external genitalia but can affect sex hormone levels, overall sexual development, and the number of sex chromosomes.
SIGNS & SYMPTOMS OF INTERSEX CONDITIONS
The signs and symptoms of intersex conditions can vary based on their underlying causes.
- Ambiguous Genitalia at Birth: The external genitalia may not have the usual male or female appearance, making it challenging to assign a clear gender.
- Micropenis: A smaller than usual penis in males, which can be a result of hormonal imbalances or genetic factors.
- Clitoromegaly (Enlarged Clitoris): In females, the clitoris is larger than expected, possibly due to hormonal influences during fetal development.
- Partial Labial Fusion: In females, there may be a partial fusion of the labia, the folds of skin surrounding the vaginal opening.
- Apparently Undescended Testes (May Turn Out to Be Ovaries) in Boys: Testes that appear not to have descended may actually be ovaries, indicating a discrepancy between external appearance and internal structures.
- Labial or Inguinal Masses (May Turn Out to Be Testes) in Girls: Masses in the labial or inguinal (groin) area in females may turn out to be testes, highlighting the complexity of internal organ development.
- Hypospadias: The opening of the penis is not at the tip, and in females, the urethra opens into the vagina instead of its usual location.
- Otherwise Unusual-Appearing Genitalia at Birth: Genitalia may have features that deviate from the typical male or female appearance, leading to uncertainty in gender assignment.
- Electrolyte Abnormalities: Imbalances in electrolytes, essential for bodily functions, may be present and require monitoring and management.
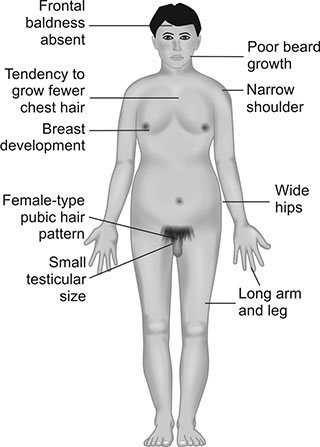
- Delayed or Absent Puberty: Puberty may be delayed or absent, affecting the development of secondary sexual characteristics such as breast development or facial hair growth.
- Unexpected Changes at Puberty: Some individuals may experience unexpected changes during puberty, further complicating the understanding of their sexual development.
- Underdeveloped Secondary Sexual Characteristics: Individuals may exhibit underdeveloped or atypical secondary sexual characteristics, such as minimal breast development in females or a lack of facial hair growth in males.
- Infertility: Some intersex conditions can lead to infertility due to irregularities in reproductive organ development or hormonal imbalances affecting gamete production.
- Atypical Pubic Hair Growth: Unusual patterns or absence of pubic hair growth may be observed, contributing to the complexity of sexual development.
- Urinary or Reproductive System Complications: Intersex conditions may be associated with complications in the urinary or reproductive systems, leading to issues like urinary tract abnormalities or difficulties in conceiving.
- Gender Dysphoria: Individuals may experience distress or discomfort with their assigned gender at birth, potentially leading to gender identity concerns and the need for psychological support.
- Hormonal Irregularities: Fluctuations in hormone levels can result in various symptoms, including mood swings, fatigue, or irregular menstrual cycles, depending on the specific intersex condition.
- Chromosomal Abnormalities: Some intersex variations involve chromosomal abnormalities beyond the typical XX or XY configurations, contributing to the diversity of intersex presentations.
- Psychosocial Challenges: Intersex individuals may face unique psychosocial challenges related to societal perceptions, self-identity, and acceptance, emphasizing the importance of supportive environments.
- Skeletal and Muscular Variances: Skeletal and muscular development may exhibit differences, affecting overall body structure and physical abilities.
- Emotional and Mental Health Factors: The emotional and mental well-being of intersex individuals may be influenced by societal attitudes, disclosure of their intersex status, and coping with unique challenges.
Diagnosis and Investigations
- Chromosome Analysis: This test examines the chromosomal composition, determining if there are variations from the normal XX (female) or XY (male) chromosome. It helps identify chromosomal intersex variations.
- Hormone Level Testing (e.g Testosterone): Measurement of hormone levels, such as testosterone, provides an overview into the endocrine system’s functioning. Deviations may indicate hormonal imbalances affecting sexual development.
- Hormone Stimulation Tests: These tests assess the body’s response to hormonal stimuli, helping evaluate the capacity of endocrine organs to produce and regulate hormones crucial for sexual development.
- Electrolyte Tests: Electrolyte tests assess the balance of minerals in the body, helping in the identification of potential abnormalities that may be associated with specific intersex conditions.
- Specific Molecular Testing: Molecular testing involves examining genetic material at the molecular level. This can reveal specific genetic variations or mutations associated with intersex conditions.
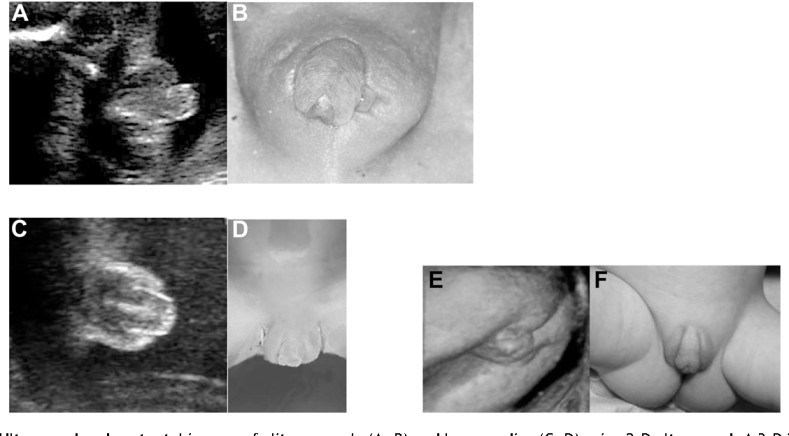
- Endoscopic Exam (Vaginal or Cervical Presence): An endoscopic examination is performed to visually confirm the absence or presence of a vagina or cervix.
- Ultrasound or MRI (Evaluation of Internal Organs): Imaging techniques, such as ultrasound or MRI, are used to visualize internal organs like the uterus. This helps determine the presence or absence of internal sex organs.

Challenges Faced by Intersex People:
I. Stigmatization: Intersex individuals face stigma due to misconceptions and lack of understanding about differences in sex development. Stigmatization can have an impact on mental health and well-being.
II. Discrimination from Birth or Discovery: Intersex individuals may experience discrimination immediately upon birth or when their intersex trait is discovered. Discrimination can be seen in many ways, affecting their sense of belonging and acceptance.
III. Infanticide: Unfortunately, some intersex infants face the risk of infanticide, due to cultural beliefs or misinformation surrounding intersex. This creates a severe threat to the lives of newborns with intersex traits.
IV. Abandonment: The discovery of intersex traits in a child may lead to parental distress, and in extreme cases, it can result in abandonment. This abandonment can have profound emotional and psychological effects on the individual.
V. Stigmatization of Families: Families with intersex members may also face stigma from society. The lack of awareness and understanding in communities can lead to judgment and isolation of the intersex.
VI. Unequal Treatment: Intersex individuals may face unequal treatment in many settings, including healthcare, education, and employment. Discrimination based on their intersex status can lead to unequal distribution opportunities and services.
VII. Mental Health Struggles: Coping with pressures from the community, discrimination, and potential medical interventions can contribute to mental health challenges for intersex individuals. Access to mental health support is very important for their well-being.
VIII. Lack of Inclusive Education: Educational systems may lack inclusivity in addressing intersex variations, leading to misunderstandings among peers and educators.
X. Inadequate Medical Care: Some intersex individuals may face challenges in accessing competent and sensitive healthcare. Inadequate medical care can result in physical and emotional distress, emphasizing the need for informed healthcare providers.
XI. Limited Awareness and Advocacy: Widespread ignorance about intersex variations contributes to the challenges faced. Increased awareness and advocacy are necessary to promote understanding, tolerance, and equal rights for intersex individuals.
XII. Isolation and Loneliness: The combination of stigma from society and limited understanding can lead to feelings of isolation and loneliness among intersex individuals.

Medical Management for Intersex Individuals:
1. Diagnosis and Evaluation:
- Chromosome Analysis: Conduct chromosomal analysis to determine the genetic composition (XX, XY, or other variations).
- Hormone Levels: Measure hormone levels, including testosterone, estrogen, and other relevant hormones.
- Imaging Studies: Utilize ultrasound or MRI to assess internal sex organs and identify any anomalies.
2. Hormone Therapy:
- Feminizing or Masculinizing Hormones: Administer prescribed hormones based on the individual’s gender identity, aiming to align secondary sex characteristics with their affirmed gender.
3. Psychological Support:
- Mental Health Counseling: Provide psychological support through counseling to address the emotional impact, to promote a positive self-image and coping mechanisms.
- Support Groups: Connect individuals with support groups to create peer support and shared experiences.
4. Prenatal Counseling:
- Genetic Counseling: Offer genetic counseling for parents to understand the intersex condition, potential issues, and available options.

Surgical Management for Intersex Individuals:
5. Genital Reconstruction Surgery:
- Feminizing Procedures: Include vaginoplasty, clitoroplasty, and labiaplasty for individuals assigned female.
- Masculinizing Procedures: Involve procedures like phalloplasty and scrotoplasty for individuals assigned male.
6. Gonadectomy:
- Removal of Gonads: Address concerns related to gonadal cancer risk or hormone imbalances by removing gonads. Determine the appropriate timing for gonadectomy based on individual health considerations.
7. Corrective Surgeries:
- Hypospadias Repair: For individuals with hypospadias, surgical correction to reposition the urethral opening may be performed.
- Vaginal or Penile Reconstruction: Tailored surgeries to address specific anatomical variations.
8. Breast Augmentation or Chest Reconstruction:
- Gender-Affirming Surgeries: Support individuals in achieving a physical appearance aligned with their gender identity.
Nursing Care for Intersex Individuals:
9. Communication and Education:
- Open Communication: Foster open dialogue, addressing concerns and providing information about medical procedures.
- Patient Education: Educate individuals and their families about the intersex condition, treatment options, and postoperative care.
10. Preoperative Care:
- Emotional Support: Offer emotional support before surgery, addressing anxieties and concerns.
- Physical Preparation: Ensure individuals understand preoperative instructions and are physically prepared for surgery.
11. Postoperative Care:
- Pain Management: Monitor and manage postoperative pain, ensuring individuals are comfortable.
- Wound Care: Provide wound care for surgical incisions to prevent infections and promote healing.
- Emotional Support: Offer psychological support during the recovery period, addressing body image concerns and promoting a positive self-image.
12. Long-Term Follow-Up:
- Hormone Monitoring: Regularly monitor hormone levels and adjust hormone therapy as needed.
- Psychosocial Support: Continue providing ongoing psychosocial support, addressing any evolving emotional needs.
13. Advocacy and Dignity:
- Advocacy: Advocate for the rights and dignity of intersex individuals, promoting inclusive and respectful care.
- Cultural Sensitivity: Ensure cultural competence and sensitivity in nursing care, respecting diverse identities and backgrounds.


well understood
Awesome
You are the best
Nice presentation
Good notes