Table of Contents
ToggleCHECK FOR HIV EXPOSURE AND INFECTION
All children found to have pneumonia, persistent diarrhea, ear discharge or very low weight for age (any of these features) and have no urgent need or indication for referral, should be assessed for symptomatic HIV infection.
- Children may acquire HIV infection from an infected mother through vertical transmission in utero, during delivery or while breastfeeding.
- Without any intervention, 30 – 40% babies born to infected mothers will themselves be infected.
- Most children born with HIV die before they reach their fifth birthday, with most not surviving beyond two years.
- Good treatment can make a big difference to children with HIV and their families.
- The child’s status may also be the first indicator that their parents are infected too.
ASSESS FOR HIV EXPOSURE AND INFECTION
ASK | LOOK, FEEL AND DIAGNOSE | |
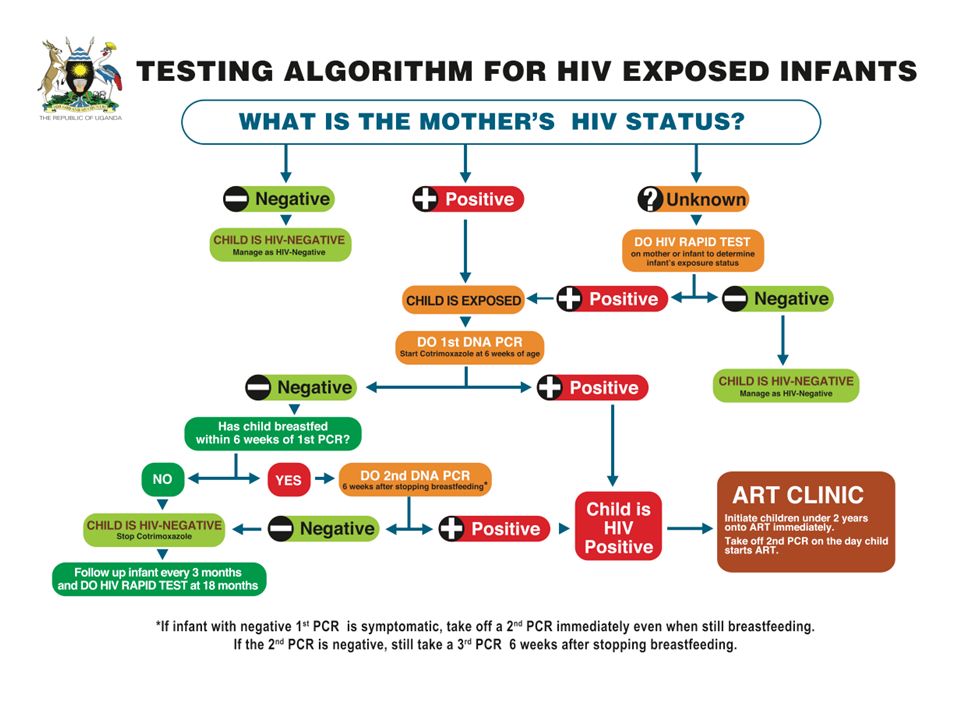
• Ask for mother’s HIV status to establish child’s HIV exposure* Is it: Positive, Negative or Unknown (to establish child’s HIV exposure)
• Ask if child has had any TB Contact | Child <18 months • If mother is HIV positive**, conduct DNA PCR for the baby at 6 weeks or at first contact with the child • If the mother’s HIV status is unknown, conduct an antibody test (rapid test) on the mother to determine HIV exposure. PRESUMPTIVE SYMPTOMATIC DIAGNOSIS OF HIV INFECTION IN CHILDREN <18 MONTHS • Pneumonia *** • Oral Candidiasis /thrush • Severe sepsis • Other AIDS defining conditions**
Child ≥18 months • If the mother’s antibody test is POSITIVE, the child is exposed. Conduct an antibody test on the child.
Child whose mother is NOT available: • Child < 18 months Do an antibody test on the child. If positive, do a DNA PCR test. • Child ≥ 18 months Do an antibody test to determine the HIV status of the child | |
CLASSIFY HIV STATUS
SIGNS | CLASSIFY AS | TREATMENT |
• Child < 18 months and DNA PCR test POSITIVE
• Child ≥ 18 months and Antibody test POSITIVE | CONFIRMED HIV INFECTION | • Initiate ART, counsel and follow up existing infections • Initiate or continue cotrimoxazole prophylaxis • Assess child’s feeding and provide appropriate counseling to the mother/caregiver • Offer routine follow up for growth, nutrition and development and HIV services • Educate caregivers on adherence and its importance • Screen for possible TB disease at every visit. • For those who do not have TB disease, start Isoniazid prophylactic therapy (IPT). Screen for possible TB throughout IPT • Immunize for measles at 6 months and 9 months and boost at 18 months • Follow up monthly as per the national ART guidelines and offer comprehensive management of HIV. Refer to appropriate national ART guidelines for comprehensive HIV care of the child. |
Child<18 months • If mother test is positive and child’s DNA PCR is negative OR • If mother is unavailable; child’s antibody test is positive and DNA PCR is negative | HIV EXPOSED | • Treat, counsel and follow up existing infections • Initiate or continue Cotrimoxazole prophylaxis • Give Zidovudine and Nevirapine prophylaxis as per the national PMTCT guidelines • Assess child’s feeding and provide appropriate counseling to the mother/caregiver • Offer routine follow up for growth, nutrition and development • Repeat DNA PCR test at 6 months. If negative, repeat DNA PCR test again at 12 months. If negative, repeat antibody test at 18 months • Continue with routine care for under 5 clinics • Screen for possible TB at every visit • Immunize for measles at 6 months and 9 months and boost at 18 months • Follow up monthly as per the national ART guidelines and offer comprehensive management of HIV. Refer to appropriate national ART guidelines for comprehensive care of the child. |
• No test results for child or mother • 2 or more of the following conditions: • Severe pneumonia • Oral candidiasis/thrush • Severe Sepsis OR • An AIDS defining condition | SUSPECTED SYMPTOMATIC HIV INFECTION | • Treat, counsel and follow-up existing infections • Give cotrimoxazole prophylaxis • Give vitamin A supplements from 6 months of age every 6 months • Assess the child’s feeding and provide appropriate counseling to the mother • Test to confirm HIV infection • Refer for further assessment including HIV care/ ART • Follow-up in 14 days, then monthly for 3 months and then every 3 months or as per immunization schedule |
Mother’s HIV status is NEGATIVE OR Mother’s HIV status is POSITIVE and child is ≥ 18 months with antibody test NEGATIVE 6 weeks after completion of breastfeeding | HIV NEGATIVE | • Manage presenting conditions according to IMNCI and other recommended national guidelines • Advise the mother about feeding and about her own health |
THEN CHECK FOR TB
ASK | LOOK AND FEEL | |
For symptoms suggestive of TB
History of contact
| Look or feel for physical signs of TB
brochodilaters. Collect sample for GeneXpert or smear microscopy
If available, send the child for laboratory tests (GeneXpert or smear microscopy) and/ or Chest X-Ray. | |
CLASSIFY
SIGNS | CLASSIFY AS | TREATMENT |
Two or more of the following in HIV Negative child AND one or more of the following in HIV Positive child:
OR
| TB | • Initiate TB treatment • Treat, counsel, and follow up any co- infections • Ask about the caregiver’s health and treat as necessary • Link the child to the nearest TB clinic for further assessment and ongoing follow-up • If GeneXpert or smear microscopy test is not available or negative, refer for further assessment |
Positive history of contact with a TB case and NO other TB symptoms or signs listed above | TB EXPOSURE | • Start Isoniazid at 10mg/kg for 6 months • Treat, counsel, and follow up existing infections • Ask about the caregiver’s health and treat as necessary • Link child to the nearest TB clinic |
NO TB symptoms or signs | NO TB | • Treat, counsel, and follow up existing infections • Start Isoniazid in HIV positive child above 1 year at 10mg/kg for 6 months |
THEN CHECK THE CHILD‘S IMMUNIZATION AND VITAMIN A STATUS
Immunization Schedule
- Follow National Guidelines as per the Child Health Card/Mother Baby Passport.
Age | Vaccine |
Birth | BCG* |
OPV-0 | |
6 weeks | DPT+HepB+HIB |
OPV-1 | |
RTV1 | |
PCV1 | |
10 weeks | DPT+HepB+HIB |
OPV-2 | |
RTV2 | |
PCV2 | |
14 weeks | DPT+HepB+HIB |
OPV-3 | |
IPV | |
RTV3 | |
PCV3 | |
9 months | Measles |
| VITAMIN A SUPPLEMENTATION Give every child a dose of Vitamin A every six months from the age of 6 months. Record the dose on the child’s chart. ROUTINE DEWORMING TREATMENT Give every child mebendazole every six months from the age of 1 year. Record the dose on the child’s chart. |
Manage HIV/AIDS using IMCI approach
- All children less than 5 years who are HIV infected should be initiated on ART irrespective of CD4 count or clinical stage.
- Remember that if a child has any general danger sign or a severe classification, he or she needs URGENT REFERRAL. ART initiation is not urgent, and the child should be stabilized first.
Steps when Initiating ART in Children
STEP 1: DECIDE IF THE CHILD HAS CONFIRMED HIV INFECTION
Child is under 18 months:
- HIV infection is confirmed if virological test (PCR) is positive.
Child is over 18 months:
- Two different serological tests are positive.
- Send any further confirmatory tests required.
If results are discordant, refer
If HIV infection is confirmed, and child is in stable condition, GO TO STEP 2
STEP 2: DECIDE IF CAREGIVER IS ABLE TO GIVE ART
Check that the caregiver is willing and able to give ART. The caregiver should ideally have disclosed the child’s HIV Status to another adult who can assist with providing ART, or be part of a support group.
- Caregiver able to give ART: GO TO STEP 3
- Caregiver not able: classify as CONFIRMED HIV INFECTION
but NOT ON ART. Counsel and support the caregiver. Follow-up regularly. Move to STEP 3 once the caregiver is willing and able to give ART.
STEP 3: DECIDE IF ART CAN BE INITIATED IN YOUR FACILITY
- If a child is less than 3 kg or has TB, Refer for ART initiation.
- If child weighs 3 kg or more and does not have TB, GO TO STEP 4
STEP 4: RECORD BASELINE INFORMATION ON THE CHILD’S HIV TREATMENT CARD
Record the following information:
- Weight and height
- Pallor if present
- Feeding problem if present
- Laboratory results (if available): Hb, viral load, CD4 count and percentage. Send for any laboratory tests that are required. Do not wait for results. GO TO STEP 5
STEP 5: START ON ART, COTRIMOXAZOLE PROPHYLAXIS AND ROUTINE TREATMENTS
- Initiate ART treatment:
- Child up to 3 years: ABC or AZT +3TC+ LPV/R or recommended first-line regimen
- Child 3 years or older: ABC + 3TC + DTG, or recommended first-line regimen.
- Give co-trimoxazole prophylaxis
- Give other routine treatments, including Vitamin A and immunizations
- Follow-up regularly as per national guidelines.
Management of HIV in Children Using IMNCI Approach
Overview: The IMNCI guidelines provide a structured approach to managing HIV in children through systematic assessment, classification, treatment, and counseling. This follows the standard IMNCI process flow: Assess → Classify → Treat → Counsel → Follow-up.
STEP 1: ASSESSMENT (Ask and Test)
Refer to: Page 9 (Child 2 months–5 years) and Page 37 (Young Infant 0–2 months)
Before managing HIV, you must determine the status for every child not already enrolled in HIV care.
Ask the Mother:
- Has the mother had an HIV test? If yes, is it Positive or Negative?
- Has the child had an HIV test? If yes, was it a DNA PCR (for infants) or Rapid test (for older children), and was it Positive or Negative?
Assess Breastfeeding Risk:
- Is the child breastfeeding now?
- Was the child breastfeeding at the time of the test or 6 weeks before?
If Status is Unknown:
- Perform an HIV test for the mother
- If the mother is positive, test the child
If Mother is Positive:
- Check if the mother is on ART (Antiretroviral Therapy)
- Check if the child is on ARV prophylaxis (e.g., Nevirapine)
STEP 2: CLASSIFICATION
Based on assessment, the child is classified into one of three categories. The management depends entirely on this classification.
| Classification | Criteria | Color Code | Management Level |
|---|---|---|---|
| CONFIRMED HIV INFECTION |
|
PINK - URGENT | Immediate treatment & ART linkage |
| HIV EXPOSED |
|
YELLOW - CLINIC | Prophylaxis & frequent monitoring |
| HIV INFECTION UNLIKELY |
|
GREEN - HOME | Routine care & prevention counseling |
STEP 3: MANAGEMENT & TREATMENT
A. Management of CONFIRMED HIV INFECTION (Red Row)
- Give Cotrimoxazole Prophylaxis:
- Start immediately for all confirmed HIV-infected children
- Prevents Pneumocystis jirovecii pneumonia (PCP) and other infections
Age/Weight Formulation Dose < 6 months 5 ml syrup (40/200 mg per 5ml) 2.5 ml once daily 6 months – 5 years 5 ml syrup OR ½ adult tablet (80/400 mg) 5 ml or ½ tablet once daily - Assess for Tuberculosis (TB) - Page 10:
- Check for cough >14 days, fever >14 days, or poor weight gain
- Check for TB contact history
- Look for physical signs: lymph node swelling, stiff neck
- Isoniazid Preventive Therapy (IPT):
- If child is HIV Positive, >1 year old, and has NO signs of TB
- Start Isoniazid 10 mg/kg daily for 6 months
- Prevents active TB disease
- Linkage to Care:
- Refer child to ART Clinic or Early Infant Diagnosis (EID) point
- IMCI focuses on identification and linkage, not starting full ART in OPD
- Ensure follow-up appointment within 1 week
- Immunization - Page 11:
- Do NOT give BCG vaccine if child has symptoms of HIV (clinical AIDS)
- Risk of disseminated BCG disease
- Give all other vaccines as per schedule
- Treat Current Illnesses Aggressively:
- HIV-positive children are "High Risk"
- If they have Pneumonia with chest indrawing, give first dose of antibiotics and refer urgently
- If diarrhea, use ORS more liberally
- If fever, investigate thoroughly for opportunistic infections
B. Management of HIV EXPOSED (Yellow Row)
- Cotrimoxazole Prophylaxis:
- Start from 6 weeks of age
- Continue until HIV infection is definitively ruled out
- Usually continued until 6 weeks after complete cessation of breastfeeding
- Testing (Diagnosis):
- Do DNA PCR test immediately if not done
- If first PCR negative but child is breastfeeding, repeat test 6 weeks after breastfeeding stops
- Do not rely on rapid test until child is ≥18 months
- ARV Prophylaxis:
- Ensure child is taking Nevirapine (NVP) syrup if indicated by national guidelines
- Check adherence daily
- Link to "Mother-Baby Care Point" for follow-up
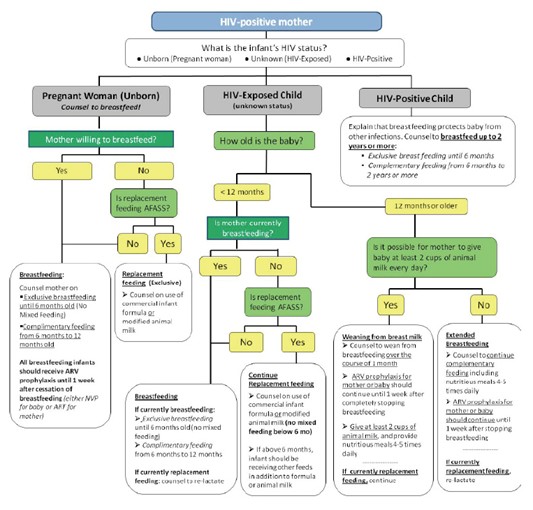
- Feeding Support:
- Support mother to practice exclusive breastfeeding correctly
- Counsel on safe replacement feeding only if AFASS criteria met
- Monitor child's weight and growth monthly
C. Management of HIV INFECTION UNLIKELY (Green Row)
- Treat any existing infections (cough, diarrhea, etc.) using standard IMCI protocols
- Counsel mother on her own health and preventing future infection
- Encourage HIV testing if status changes or risk occurs
- Continue routine immunizations
STEP 4: COUNSELING THE MOTHER
Feeding Advice (Page 26, 29)
Correct feeding is critical to reduce HIV transmission and ensure child survival.
- Exclusive Breastfeeding (First 6 months):
- Mothers with HIV should exclusively breastfeed for the first 6 months
- Mixed feeding (breastmilk + other foods/fluids) is DANGEROUS as it damages gut lining and increases HIV transmission risk
- Exclusive breastfeeding provides antibodies and reduces infections
- Continued Breastfeeding (6-12 months):
- Encourage continued breastfeeding up to 12 months
- Breastfeeding should only stop when a nutritionally adequate and safe diet can be provided
- Gradually introduce complementary foods from 6 months while continuing breastfeeding
- Replacement Feeding ("AFASS" Criteria - Page 29):
Advise stopping breastfeeding ONLY if ALL these criteria are met:
AFASS Requirements Acceptable Socially and culturally acceptable to mother and family Feasible Mother has time, knowledge, skills, and support to prepare formula 8-12 times daily Affordable Mother/family can afford continuous formula supply for 1 year without harming family nutrition Sustainable Continuous supply of formula and clean water is assured Safe Clean water, hygienic preparation, and feeding with cup (not bottle) can be ensured - Mouth Conditions:
- Check for oral thrush or sores in the child (Page 19, 39)
- Treat immediately with Nystatin 1 ml four times daily for 7 days
- Sores increase HIV transmission risk during breastfeeding
- Check mother's breasts for thrush and treat if present
General Care & Hygiene (Page 29)
- Hygiene: Teach mother to wash hands before food preparation to prevent diarrhea (HIV children are very susceptible)
- Growth Monitoring: Weigh child at every visit. Poor weight gain is a major sign of HIV progression or treatment failure
- Mother's Health (Page 30):
- Counsel mother on her own nutrition and ART adherence
- Ensure she is on ART to suppress viral load (reduces transmission to baby)
- Check if she needs family planning or STI screening
- Provide psychosocial support and link to support groups
STEP 5: FOLLOW-UP
- Exposed Children: Follow up monthly to monitor growth and ensure prophylactic medication (Cotrimoxazole/Nevirapine) adherence
- Confirmed Children: Follow up at ART clinic as per schedule (every 2 weeks initially, then monthly)
- Acute Illness: If HIV-positive child has cough or cold, follow up in 5 days rather than waiting, as they deteriorate faster
- Growth Monitoring: Plot weight on growth chart at every visit; flattening curve indicates treatment failure
ADDITIONAL PROTOCOL: Initiating ART in Children
STEP 1: DECIDE IF THE CHILD HAS CONFIRMED HIV INFECTION
- Child is under 18 months: HIV infection is confirmed if virological test (PCR) is positive
- Child is over 18 months: Two different serological tests are positive
- Send any further confirmatory tests required
- If results are discordant, refer to specialist
- If HIV infection is confirmed, and child is in stable condition, GO TO STEP 2
STEP 2: DECIDE IF CAREGIVER IS ABLE TO GIVE ART
Check that the caregiver is willing and able to give ART. The caregiver should ideally have:
- Disclosed the child's HIV Status to another adult who can assist
- Be part of a support group
Caregiver able to give ART: GO TO STEP 3
Caregiver not able: Classify as CONFIRMED HIV INFECTION but NOT ON ART. Counsel and support the caregiver. Follow-up regularly. Move to STEP 3 once the caregiver is willing and able to give ART.
STEP 3: DECIDE IF ART CAN BE INITIATED IN YOUR FACILITY
- If child is less than 3 kg or has TB: Refer for ART initiation
- If child weighs 3 kg or more and does not have TB: GO TO STEP 4
STEP 4: RECORD BASELINE INFORMATION ON THE CHILD’S HIV TREATMENT CARD
Record the following information:
- Weight and height
- Pallor if present
- Feeding problem if present
- Laboratory results (if available): Hb, viral load, CD4 count and percentage
- Send for any laboratory tests that are required. Do not wait for results. GO TO STEP 5
STEP 5: START ON ART, COTRIMOXAZOLE PROPHYLAXIS AND ROUTINE TREATMENTS
- Initiate ART treatment:
- Child up to 3 years: ABC or AZT + 3TC + LPV/r or recommended first-line regimen
- Child 3 years or older: ABC + 3TC + DTG, or recommended first-line regimen
- Give co-trimoxazole prophylaxis (as per dosing table above)
- Give other routine treatments: Vitamin A, immunizations, deworming
- Follow-up regularly as per national guidelines
- Never delay treatment while waiting for laboratory results
- Always check for TB before starting ART
- Ensure caregiver readiness and support before initiating ART
- Monitor growth and development closely in all HIV-exposed and infected children
- Maintain confidentiality while providing family-centered care
Recommended First-Line ARV Regimens
Patient Category | Indication | ARV Regimen |
Adults and Adolescents (aged 10 and above) | Initiating ART | TDF+3TC+DTG |
Alternative Regimens | ||
TDF+3TC+DTG (Contraindications for EFV) | ||
ABC+3TC+DTG (Contraindications for TDF) | ||
Pregnant or Breastfeeding Women | Initiating ART | TDF+3TC+DTG |
Alternative Regimen | ||
ABC+3TC+ATV/r (Contraindications for TDF or EFV) | ||
Children (3 to <10 years) | Initiating ART | ABC+3TC+DTG |
Alternative Regimen | ||
ABC+3TC+NVP (Contraindications for EFV) | ||
Children Under 3 Years | Initiating ART | ABC+3TC+LPV/r |
Alternative Regimen | ||
AZT+3TC+LPV/r (Hypersensitivity reaction to ABC) | ||
Second- and Third-Line ART Regimens
Population | Patients Failing First-Line Regimens | Second-Line Regimens | Third-Line Regimens |
Adults, Pregnant and Breastfeeding Women, Adolescents | TDF + 3TC + DTG | AZT+3TC+ATV/r (recommended) or AZT+3TC+LPV/r (alternative) | All 3rd line regimens guided by resistance testing |
If not exposed to INSTIs: DRV/r + DTG ± 1-2 NRTIs | |||
If exposed to INSTIs: DRV/r + ETV±1-2 NRTIs | |||
TDF + 3TC + DTG | |||
ABC+ 3TC+ DTG | |||
ABC+ 3TC+ EFV | |||
ABC/3TC/NVP | |||
TDF/3TC/NVP | |||
AZT/3TC/NVP | |||
TDF+3TC+ATV/r (recommended) or TDF+3TC+LPV/r | AZT/3TC/EFV | ||
Children (3–<10 years) | ABC + 3TC + DTG | AZT+3TC+LPV/r | For children above 6 years, and prior exposure to INSTIs, DRV/r±1-2 NRTIs |
ABC+ 3TC + NVP | |||
AZT+3TC+NVP | |||
ABC+3TC+LPV/r | |||
For children below 6 years, AZT/3TC/EFV | |||
DRV/r+ RAL+ 2 NRTIs | |||
AZT+3TC+LPV/r | |||
Children Under 3 Years | ABC+3TC+LPV/r pellets | AZT+3TC+RAL | Optimize regimen using genotype profile |
AZT+3TC+LPV/r pellets | |||
ABC+3TC+RAL | |||
AZT+3TC+NVP | |||
ABC+3TC+LPV/r | |||
Principles for Selecting ARV Regimens:
- Lower toxicity
- Better palatability and lower pill burden
- Increased durability and efficacy
- Sequencing to spare other formulations for the 2nd line regimen
- Harmonization across age and population
- Lower cost
- Facilitate achieving a recommended regimen for the majority of PLHIV
Rationale for Alternative Regimens:
- TDF+3TC+DTG: EFV contraindications
- ABC+3TC+DTG: TDF contraindications
- ABC+3TC+ATV/r: Contraindications for TDF or EFV
- ABC+3TC+NVP: EFV contraindications in children (3 to <10 years)
- AZT+3TC+LPV/r: Hypersensitivity reaction to ABC (rare)
Considerations:
- Dolutegravir (DTG) benefits: low potential for drug interactions, shorter time to viral suppression, higher resistance barrier, long half-life, and low cost.
- ABC+3TC+EFV once-a-day dose for improved adherence.
- LPV/r-based regimen for children under 3 years due to reduced risks and high resistance barrier.
ABC: Abacavir AZT: Zidovudine 3TC: Lamivudine LPV/r: Lopinavir/Ritonavir RTV: Ritonavir NVP: Nevirapine | EFV: Efavirenz DTG: Dolutegravir TDF: Tenofovir Disoproxil Fumarate RAL: Raltegravir ATV/r: Atazanavir/Ritonavir |
TB/HIV Co-Infection Treatment Based on Age/Weight
AGE/WEIGHT | FIRST LINE TB/HIV CO-INFECTION |
< 2 Weeks | Start TB treatment immediately, start ART (Usually after 2 weeks of age) once tolerating TB drugs |
> 2 Weeks and <35 kgs | ABC/3TC/LPVr/RTV If not able to tolerate super boosted LPVr/RTV then use ABC/3TC + RAL for duration of TB treatment. After completion of TB treatment revert back to the recommended 1st line regimen ABC/3TC +LPVr. If on ABC/3TC/DTG regimen – continue If on NVP based regimen, change to EFV. |
>35 kgs body weight and < 15 years age | ABC/3TC/DTG continue with the regimen AND double the dose for DTG If on PI based regimen switch the patients to DTG, hence doubling the dose |
DOSAGE OF COTRIMOXAZOLE PROPHYLAXIS
WEIGHT (KG) | SUSPENSION 240MG PER 5ML | SINGLE STRENGTH TABLET 480MG (SS) | DOUBLE STRENGTH TABLET 960MG (DS) |
1-4 | 2.5ml | 1/4 SS tab | – |
5-8 | 5ml | 1/2 SS tab | 1/4 DS tab |
9-16 | 10ml | 1 SS tab | 1/2 DS tab |
17-30 | 15ml | 2 SS tab | 1 DS |
>30(Adults and adolescents) | – | 2 SS | 1 DS |
Dose by body weight is 24-30 mg/kg once daily of the trimethoprim-sulphamethaxazole – combination drug.
• Oral thrush management– use miconazole gel
• Cotrimoxazole use is still recommended
• Most infants and children initiated on treatment take time before immune recovery occurs
• Children on LPV/r – continue with boosted ritonavir
• RAL – for those unable to tolerate super boosted LPV/r
Paediatric ARVs Dosages
WEIGHT RANGE (KG) | ABACAVIR + LAMIVUDINE 120 mg ABC + 60 mg 3TC | ZIDOVUDINE + LAMIVUDINE 60 mg ZDV + 30 mg 3TC | EFAVIRENCE (EFV) Once Daily 200mg tabs | LAMIVUDINE + ZIDOVUDINE Twice Daily 200mg tabs |
3 – 5.9 | 0.5 tab | 1 tab | – | |
6 – 9.9 | 1 tab | 1.5 tabs | – | |
10 – 13.9 | 1 tab | 2 tabs | 1 tab | 1.5 tabs |
14 – 19.9 | 1.5 tabs | 2.5 tabs | 1.5 tabs | + 1 tab in AM & 0.5 tab in PM |
20 – 24.9 | 2 tabs | 3 tabs | 1.5 tabs | 1 tab in AM & 0.5 tab in PM |
25 – 34.9 | 300 mg ABC + 150 mg 3TC | 300 mg ZDV + 150 mg 3TC | 2 tabs | 1 tab in AM & 0.5 tab in PM |
Manage Side Effects of ARV Drugs
SIGNS or SYMPTOMS | APPROPRIATE CARE RESPONSE |
Yellow eyes (jaundice) or abdominal pain | Stop drugs and REFER URGENTLY |
Rash | If on abacavir, assess carefully. Call for advice. If severe, generalized, or associated with fever or vomiting: stop drugs and REFER URGENTLY |
Nausea | Advise drug administration with food. If it persists for more than 2 weeks or worsens, call for advice or refer. |
Vomiting | If medication is seen in vomitus, repeat the dose. If vomiting persists, bring the child to the clinic. REFER URGENTLY if vomiting everything or associated with severe symptoms. |
Diarrhoea | Assess, classify, and treat using diarrhoea charts. Reassure that it may improve in a few weeks. Follow up as per chart booklet. Call for advice or refer if not improved after two weeks. |
Fever | Assess, classify, and treat using fever chart. |
Headache | Give paracetamol. If on efavirenz, reassure that it is common and usually self-limiting. Call for advice or refer if it persists for more than 2 weeks or worsens. |
Sleep disturbances, nightmares, anxiety | Due to efavirenz. Administer at night on an empty stomach with low-fat foods. Call for advice or refer if it persists for more than 2 weeks or worsens. |
Tingling, numb, or painful feet or legs | If new or worse on treatment, call for advice or refer. |
Changes in fat distribution | Consider switching from stavudine to abacavir, consider viral load. Refer if needed. |
GIVE FOLLOW – UP CARE FOR ACUTE CONDITIONS
Care for the child who returns for follow-up using all the boxes that match the child’s previous classifications.
If the child has any new problem, assess, classify fully and treat as on the ASSESS AND CLASSIFY chart.
PNEUMONIA After 2 days Check the child for general danger signs. Assess the child for cough or difficult breathing. Ask:
Treatment:
|
WHEEZINGAfter 2 days Check the child for general danger signs or chest indrawing. Assess the child for cough or difficult breathing. Ask:
For Children under 1 year:
General danger sign or stridor in a calm child or chest indrawing, fast breathing, poor feeding;
For Children over 1 year:
General danger sign or stridor in a calm child or chest indrawing, fast breathing, poor feeding;
|
PERSISTENT DIARRHOEAAfter 5 days Ask:
Treatment:
|
DYSENTERYAfter 2 days Assess the child for diarrhea. > See ASSESS & CLASSIFY chart Ask:
Treatment:
If the condition is the same: add Metronidazole to the treatment. Give it for 5 days. Advise the mother to continue ciprofloxacin and zinc and to return in 2 days.
|
UNCOMPLICATED MALARIAIf fever persists after 3 days, or recurs within 14 days: Do a full reassessment of the child. >See ASSESS & CLASSIFY chart. Assess for other causes of fever. Treatment:
|
FEVER – NO MALARIAIf fever persists after 3 days: Do a full reassessment of the child. > See ASSESS & CLASSIFY chart (see pg 6) Assess for other causes of fever. Treatment:
|
EYE OR MOUTH COMPLICATIONS OF MEASLESAfter 2 days: Look for red eyes and pus draining from the eyes. Look at mouth ulcers. Smell the mouth. Treatment for Eye Infection:
Treatment for Mouth Ulcers:
Treatment for thrush:
|
EAR INFECTIONAfter 5 days: Reassess for ear problem. > See ASSESS & CLASSIFY chart Measure the child’s temperature. Treatment:
|
FEEDING PROBLEMAfter 5 days: Reassess feeding. See questions at the top of the COUNSEL THE MOTHER. Ask about any feeding problems found on the initial visit.
|
PALLORAfter 14 days:
|
MALNUTRITIONAfter 14 days: If the child is gaining weight, encourage the mother to continue with feeding. Counsel the mother about any feeding problem. SEVERE MALNUTRITION WITHOUT COMPLICATIONS After 7 days or during regular follow-up:
Treatment:
MODERATE ACUTE MALNUTRITION After 14 days:
Treatment:
|
| HIV EXPOSED & INFECTED CHILDREN HIV INFECTED CHILD After 1 month:
HIV EXPOSED CHILD (<18 months): For children tested DNA PCR Negative After 1 month:
|
Feeding Counseling
For Mothers and caregivers of infants under 18 months.
Goals:
- Discuss ongoing HIV risk from breastfeeding and the implications on test results.
- Support the mother as she makes choices about feeding for the infant.
- Ensure that the mother understands the testing procedure for infants under 18 months.
- If positive, discuss the need to start ART immediately.
Just after giving birth, the mother should be counseled on:
- HIV testing for herself: if she did not test in antenatal, she should be tested soon after delivery.
- Infant feeding practices.
- HIV testing for the infant: at 6 weeks, the infant can be tested.
Overview of Infant Feeding Guidelines for Exposed Infants
- HIV+ mothers should exclusively breastfeed infants for the first 6 months.
- Complementary feeds should be introduced from 6 months.
- Continue to breastfeed for 12 months.
- During breastfeeding, the infant should receive daily NVP until 1 week after stopping breastfeeding.
- Breastfeeding should only stop once a nutritionally adequate and safe diet without breast milk can be provided.
- When an infected mother decides to stop breastfeeding at any time, they should do so over the course of 1 month.