MENSTRUAL DISORDERS
Menstrual Disorders
Menstrual disorders are abnormalities in menstruation during reproductive life.
Common disorders associated with menstruation are as follows;
- Amenorrhoea
- Dysmenorrhoea
- Menorrhagia
- Metrorrhagia
- Polymenorrhoea (epimenorrhoea)
- Dysfunctional uterine bleeding
- Endometriosis
AMENORRHOEA
Amenorrhoea refers to absence of menstruation which occurs in female during their reproductive age.
Types of Amenorrhoea
- Primary amenorrhoea. This is the failure of menses to occur by 16 years of age. It could be due to imperforated hymen when she has been menstruating but when blood does not come out.
- Secondary amenorrhoea. This is the cessation of menses in a woman who has previously menstruated. It is regarded as secondary when she takes a period of 6 month and above without seeing her menses.
Causes of Amenorrhoea
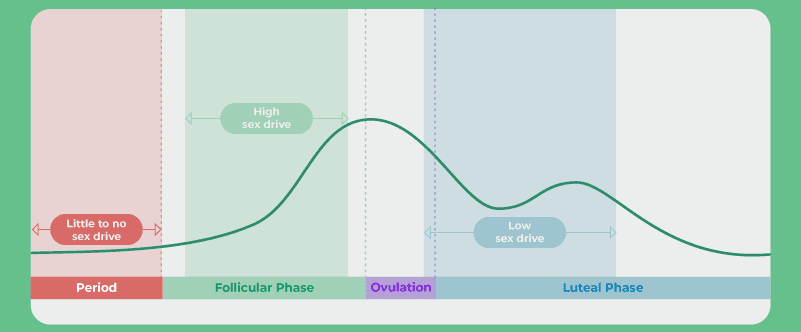
- Physiological like pregnancy and lactation, during pregnancy the levels of oestrogen and progesterone remains high thus ensuring the integrity of the endometrium resulting into amenorrhoea.
- During lactation– soon after delivery prolactin is secreted in large quantities by the anterior pituitary. There is partial suppression of LH production so that the ovarian follicles may grow but ovulation does not occur resulting into amenorrhoea.
- Hypothalamic dysfunction-such kind of patients have lower levels of follicle stimulating hormone(FSH) and luteinizing hormone (LH). Several congenital syndromes associated with abnormal hypothalamic- gonadal function have been described and these conditions present with primary amenorrhoea and absence of secondary sex characteristics. It is also due to failure to the development of central structures of hypothalamus.
- Pituitary disorder, this is associated with elevated levels of prolactin (hyperplolactinemia).
- Congenital abnormalities , like imperforated hymen, vaginal septum, no uterus, no endometrium but with uterus, absence of ovaries, cervical stenosis, and absence of hypothalamus (kallmann’s syndrome). This is a congenital hypogonadotrophic hypogonadism disorder characterized by absence of secondary sex characteristics.
- Change of environment or occupation.
- Fear, anxiety or excitement
- Pseudoamenorrhoea, pseudo means false. Here a woman psychologically thinks that she is pregnant yet she is not.
- After hysterectomy or bilateral removal of ovaries
- Full doses of radiation
- Drugs ,like contraceptives especially hormonal methods
- Debilitating diseases like, TB, HIV/AIDS, DM etc
- Tumours of the pituitary gland, hypothalamus, ovaries and uterus
- Early onset of menopause
- Idiopathic
Diagnosis and investigation
- A detailed history taking (history of change in weight, presence of stress, questions about excessive weight, presence of excessive body or facial hair) and physical examination.
- Urine for HCG to rule out pregnancy
- Ultra sound scans of the pelvis to visualize the contents or organs of the pelvic cavity.
- Blood for hormone analysis to rule out hormonal imbalance.
- Computerized tomography (CT) scans to visualize the organs.
Management of Amenorrhoea
This will depend on the cause. It may be medical, surgical, or psychological.
Nursing Management:
- Assessment: Conducting a comprehensive evaluation of the woman\’s medical and menstrual history, as well as performing a physical examination to identify the underlying cause of amenorrhea.
- Emotional Support: Offering empathetic and non-judgmental support to address any emotional distress associated with the condition.
- Education: Providing information on menstrual health, reproductive anatomy and physiology, and the potential causes and treatment options for amenorrhea.
- Lifestyle Modifications: Encouraging women to adopt a healthy lifestyle, including regular exercise, balanced nutrition, stress reduction, and sufficient sleep, as these factors can contribute to hormonal balance regulation.
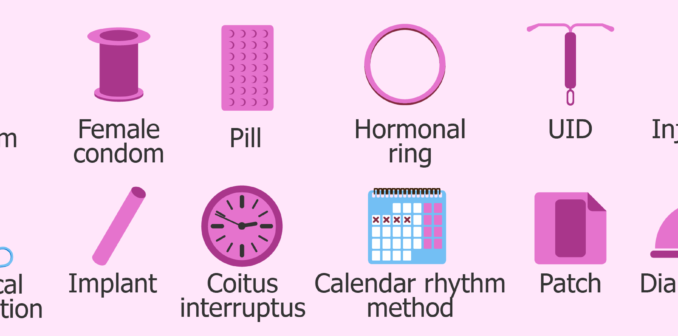
- Contraception Counseling: Discussing contraceptive methods and family planning options to prevent unintended pregnancies.
Medical Management:
Medical management of amenorrhea encompasses treating the root cause identified through investigations done. Various medical management options include:
- Hormone Therapy: If hormonal imbalance, such as polycystic ovary syndrome or hypothalamic dysfunction, is determined as the cause of amenorrhea, hormone therapy may be prescribed to regulate hormone levels and restore menstruation.
- Medications: Certain medications like progestins or combined oral contraceptives may be prescribed to induce menstruation or regulate the menstrual cycle.
- Treatment of Underlying Conditions: If amenorrhea is a result of an underlying medical condition, such as a thyroid disorder or a pituitary tumor, appropriate medical treatment will be initiated to address the specific condition.
- Hyperprolactinaemia is treated by administration of bromocriptine. This is an ergot alkaloid which directly opposes prolactin secretion. Radiotherapy is reserved for those patients who fails to respond to medical therapy.
Surgical Management:
Surgical management is rarely required for the treatment of amenorrhea. However, in certain cases, surgery may be necessary to address structural abnormalities or correct anatomical issues contributing to the condition. For example:
- Hysteroscopic Surgery: This minimally invasive procedure involves the insertion of a thin, illuminated tube called a hysteroscope through the vagina and cervix to visualize and treat abnormalities within the uterus, such as polyps or adhesions.
- Imperforated hymen is treated by incision and drainage. Very large amount of blood may be released, and if the septum is particularly thick, some form of plastic operation may be required.
- Surgical Intervention: In some instances, surgical intervention may be essential to correct structural abnormalities in the reproductive organs or to remove tumors or cysts that are interfering with normal menstruation.
Psychological Management:
Psychological management plays a crucial role in providing support for women with amenorrhea, as it significantly impacts their emotional well-being. It involves:
- Counseling: Offering psychological counseling or referring women to mental health professionals who can assist them in coping with the emotional distress associated with amenorrhea.
- Support Groups: Suggesting participation in support groups or facilitating connections with other women who have faced similar challenges to foster a sense of community and validation.
- Body Image and Self-esteem: Addressing concerns related to body image and promoting a positive self-image by emphasizing that amenorrhea does not define femininity or a woman\’s worth.
DYSMENORRHOEA
Dysmenorrhea is a medical term used to describe painful menstrual cramps that occur just before or during menstruation (the monthly shedding of the uterine lining). OR These are painful menstrual periods.
Nearly 50% of all women have some degree of pain associated with their periods. About 10% are unable to perform their normal activities because of this pain. Dysmenorrhoea can occur at any age, though uncommon in the first 6 months after the onset of menses and relatively uncommon in the years prior to menopause. The most common ages for this problem to occur are in the late teens and early twenties.
Cause
The exact cause of primary dysmenorrhea is not fully understood, but it is believed to be related to the release of certain chemicals called prostaglandins in the uterus. This is due to release of a chemical substance called prostaglandins from the lining cells of the uterus at the time of menstrual period. The prostaglandin causes contractions of the muscle wall of the uterus, that are called menstrual cramps.
Types of dysmenorrhoea
Primary dysmenorrhoea.
This refers to painful menstruation that starts few years after puberty and usually no exact cause can be identified.
Pre-disposing factors
- Narrow cervical OS (stenosis) ,which results into tension during contraction of muscles.
- Reduced blood supply to the endometrium (ischaemia)
- Hormonal imbalance
- Retroverted uterus, that is , when the uterus leans backwards resulting into tension.
- Psycological or social stress, fear or anxiety
Signs and symptoms
Dysmenorrhea is cyclic with pain most often occurring just before or during the first few days of each period.
- Lower abdominal pain (LAP) that varies in severity among individuals, ranging from mild to colicky or crampy, extending to the back, thighs and legs.
- Nausea and vomiting
- Constipation or diarrhea
- Fainting, headache, malaise
- Irritability, nervousness, depression
Diagnosis
- History taking: It is through history taking, ask about the nature of pain, duration and when it occurs. This is often confirmatory.
- Physical examination: It is also through physical examination to rule out pelvic tumours, endometriosis which is often absent.
Treatment
Treatment options for dysmenorrhea depend on the severity of symptoms and the underlying cause.
- For primary dysmenorrhea, Non steroidal anti inflammatory drugs (NSAIDS) like Iboprufen, mefenamic acid, diclofenac and others. These prevent the formation of prostaglandins in the uterine lining cells. They are more effective if taken before the onset of cramps.
- Antispasmodics like Buscopan
- Antiemetics like Phenegan for nausea and vomiting.
- Heat therapy in the form of a hot water bottle or heating pad applied to the abdomen can also provide relief.
-
- Drugs
- Mild analgesics to relieve pain eg ibuprofen 400mg tds.
- Prostaglandin synthetase inhibitors eg. Mefenamic acid 250-500mg tds or Flufenamic acid 100-200mg tds
- Oral contraceptives eg COCs. These decrease endometrial proliferation.
- Progesterones. Eg dydrogesterone 10mg b.d taken from day 5 of the cycle for 20 days. Mechanism of action is presumably myometrial relaxation.
NOTE
- Begin treatment 2 days before menstruation periods begins and continue until 2 days after the period has stopped.
- Avoid additive drugs since this treatment is for long period.
- Contraceptive drugs like COCs may be given to suppress ovulation and relieve pain. Usually given for 4-6 months and many get permanent relief after this treatment has been stopped.
- Dilatation and Curettage (D&C) may be of help to remove necrotic tissue of endometrium, but usually not encouraged since it increases the risk of infections.
- Cervical stenosis can be treated by surgical widening of the canal.
- Effective counseling is important since pain is usually psychological to avoid drug dependence and abuse.
- Delivery or with age will finally treat pain since there will be relaxation of uterine muscles and reduce ischaemia.
- Encourage enough rest and sleep as well as exercises, hygiene and good diet.
- Other management options may include hypnotherapy and acupuncture.
Secondary dysmenorrhoea
This refers to painful periods which start many years following normal and well established menstrual periods. It is more of pathological occurrence and on investigations the cause is easily established.
Causes
- Pelvic inflammatory diseases (PID)
- Uterine fibroids. This results into the partial contraction of the uterus resulting into pain.
- Endometriosis: This is the growth of the endometrial tissue in other area rather than the uterus.
- Endometritis: This is the inflammation of the endometrium.
Signs and symptoms
In addition to signs and symptoms found in primary dysmenorrhoea, there is;
- Lower abdominal pain (LAP) usually happens 3-4 days or even a week before menstruation and either pain becomes better or worsens with menstruation.
- There may be backache
- Signs and symptoms of menorrhagia
- Painful coitus
- Inability to conceive.
Management
Investigate and treat the cause.
NURSING MANAGEMENT
Nursing diagnosis
- Acute pain related to increased uterine contractility evidenced by verbalization of the girl or woman.
Nursing interventions
- Warm the abdomen, this causes vasodilation and reduces the spasmodic contractions of the uterus.
- Massage the abdominal area that feels pain, this reduces pain due to the stimulus of therapeutic touch.
- Perform light exercises ,to blood flow to the uterus and improves muscle tone.
- Perform relaxation techniques to reduce pressure to get relaxed.
- Administer analgesics as prescribed to block nociceptive receptors
- Ineffective individual coping related to emotional stress evidenced by patient’s verbalization.
Nursing interventions
- Assess patient’s understanding of the condition. This is because patient’s anxiety of the pain is greatly influenced by knowledge.
- Provide an opportunity to discuss how the pain is. Help the patient identify coping mechanisms.
- Provide the patient with periods of sleep or rest. Ensures relaxation of the body and mind.
- Risk for imbalanced nutrition less than body requirements related to nausea and vomiting.
Nursing interventions
- Provide the patient with periods of sleep or rest ,this is to ensure relaxation of the body.
- Encourage small frequent feeds. These are easily tolerated by the patient.
- Administer anti-emetic drugs like promethazine. This blocks the emetic centres.
Nursing Concerns:
- Assessing the severity and characteristics of the pain, including its location, intensity, and duration.
- Monitoring vital signs and assessing for any signs of complications or worsening symptoms.
- Assessing menstrual patterns, including the duration and heaviness of bleeding.
- Evaluating the impact of dysmenorrhea on the patient\’s quality of life, emotional well-being, and ability to carry out daily activities.
- Assessing for any associated symptoms or complications, such as nausea, vomiting, headaches, or anemia.
Nursing Interventions:
- Providing pain management: Administering prescribed pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), as ordered by the healthcare provider. Monitoring the effectiveness of pain relief and reassessing pain levels after medication administration.
- Applying heat therapy: Instructing the patient on the use of heat therapy, such as a hot water bottle or heating pad, to relieve pain. Educating the patient on the proper technique and duration of heat application.
- Assisting with relaxation techniques: Teaching relaxation techniques, deep breathing exercises, and guided imagery to help the patient manage pain and reduce stress.
- Promoting rest and comfort: Encouraging the patient to rest in a comfortable position during painful episodes. Providing supportive pillows, blankets, or cushions to enhance comfort.
- Educating the patient about the condition: Providing information about the underlying cause of secondary dysmenorrhea, its management, and treatment options. Answering any questions or concerns the patient may have.
- Collaborating with the healthcare team: Communicating and collaborating with the healthcare provider, gynecologist, or other specialists involved in the patient\’s care to ensure appropriate management of the underlying condition.
- Offering emotional support: Acknowledging and validating the patient\’s pain and emotional distress. Providing a supportive environment for the patient to express her feelings and concerns. Referring to counseling or support groups if needed.
MENORRHAGIA
Menorrhagia is a condition characterized by abnormally heavy or prolonged menstrual bleeding. Can be heavy or prolonged menstrual bleeding or both.
Causes
- Hormonal imbalances: Fluctuations in estrogen and progesterone levels can disrupt the normal menstrual cycle and lead to excessive bleeding.
- Uterine fibroids: These noncancerous growths in the uterus can cause heavy menstrual bleeding.
- Adenomyosis: The condition where the inner lining of the uterus (endometrium) grows into the muscular wall of the uterus can result in heavy bleeding.
- Polyps: Small, benign growths on the lining of the uterus can contribute to menorrhagia.
- Endometrial hyperplasia: Abnormal thickening of the uterine lining can cause heavy bleeding.
- Inherited bleeding disorders: Certain inherited conditions, such as von Willebrand\’s disease, can lead to excessive bleeding during menstruation.
- PID (pelvic inflammatory disease)
- Retroverted uterus
- Cancers like cancer of the cervix and endometrial cancer
Signs and symptoms
- Menstrual bleeding lasting longer than seven days.
- Soaking through one or more sanitary pads every hour for several consecutive hours.
- Passing large blood clots during menstruation.
- Fatigue and tiredness due to excessive blood loss.
- Shortness of breath or rapid heart rate caused by anemia.
- Feeling lightheaded or dizzy.
- Menstrual periods that disrupt daily activities.
Investigations
- Complete medical history and physical examination.
- Blood tests to assess blood count, iron levels, and hormonal imbalances.
- Transvaginal ultrasound to evaluate the structure of the uterus and detect any abnormalities.
- Endometrial biopsy to examine a sample of the uterine lining for abnormalities or cancer.
- Hysteroscopy, a procedure using a thin, lighted tube inserted into the uterus, to directly visualize the uterine cavity.
- Bleeding time to test for coagulopathy
- Prothrombin time to test for coagulopathy.
- Clotting time to test for availability of platelets.
- In the above three tests, results will be abnormal.
- Full haemoglobin levels and hormone analysis to rule out hormonal imbalance.
MANAGEMENT
The best management is to investigate and treat the cause
Medical Management of Menorrhagia:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and bleeding. Hormonal contraceptives, such as birth control pills or hormonal intrauterine devices (IUDs), can regulate menstrual cycles and decrease bleeding.
- Iron supplementation: If anemia is present due to excessive bleeding, iron supplements may be recommended to restore iron levels.
- Endometrial ablation: A minimally invasive procedure that destroys the lining of the uterus to reduce menstrual bleeding.
- Uterine artery embolization: A procedure in which small particles are injected into the blood vessels supplying the uterus to reduce blood flow and control bleeding.
Nursing management
- Symptom management: Assisting patients in managing pain and discomfort during heavy bleeding episodes.
- Emotional support: Acknowledging the emotional impact of menorrhagia and providing a safe space for patients to express their concerns.
- Education: Providing information on menstrual hygiene, use of sanitary products, and available treatment options.
- Lifestyle modifications: Advising patients to maintain a healthy lifestyle, including a balanced diet and regular exercise, to promote overall well-being.
Nursing diagnosis
Ineffective tissue perfusion related to excessive bleeding evidenced by pallor.
Nursing interventions
- Assess patient’s vital signs. To obtain baseline data.
- Lift the foot of the bed. To allow blood flow to vital centres of the body like brain, kidneys, lungs, heart and liver.
- Administer intravenous fluids. To maintain the circulatory volume of fluids.
- Administer vitamin k as prescribed to reduce bleeding. Vitamin k activates coagulation factors.
- Administer whole blood as prescribed. To maintain circulatory volume of blood.
METRORRHAGIA
Metrorrhagia is a medical term used to describe irregular or abnormal uterine bleeding that occurs between menstrual periods. Can also be defined as cyclic bleeding at normal intervals, the bleeding is either excessive in amount (>80 ml) or duration or both.
This is a symptom of some underlying pathology which may be organic or functional.
Causes
- Fibroid uterus
- Adenomyosis (A disorder of the glands that secrete cervical mucus and fluids)
- Pelvic endometriosis(The presence of endometrium elsewhere than in the lining of the uterus causing premenstrual pain and dysmenorrhea)
- Chronic tubo-ovarian mass
- Retroverted uterus-due to congestion
- Uterine polyp. This is due to vast blood supply to the polyp which makes it bleed easily.
- Cervical erosions. This is due to the presence of a wound and an increase in blood supply resulting into bleeding.
- Cancer of the cervix or endometrial cancer.
- Chronic threatened abortion or incomplete abortion
- Retained pieces of placenta. This interferes with contraction of the uterus to seal off blood vessels after birth.
- Mole pregnancy. This is due to an abnormal uterine mass which grows after fertilization and is supplied with a lot of blood capillaries resulting into bleeding.
- Ovulation bleeding
- Short cycles like polymenorrhoea.
Signs and symptoms
- Bleeding between menstrual periods.
- Irregular menstrual cycles.
- Heavier or lighter bleeding than usual during menstrual periods.
- Prolonged bleeding that lasts longer than normal.
- Pelvic pain or discomfort.
- Fatigue or tiredness due to excessive blood loss.
- Anemia symptoms, such as shortness of breath, dizziness, or weakness.
Investigations
- Medical history and physical examination: A detailed history of menstrual cycles, symptoms, and any relevant medical conditions is obtained. A pelvic examination may be performed to assess the reproductive organs.
- Hormone level assessment: Blood tests may be conducted to evaluate hormone levels, including estrogen, progesterone, and thyroid hormones.
- Transvaginal ultrasound: This imaging test can provide visualization of the uterus, ovaries, and any structural abnormalities.
- Endometrial biopsy: A sample of the uterine lining may be obtained for microscopic evaluation to check for abnormalities or cancer.
- Hysteroscopy: A procedure in which a thin, lighted tube is inserted into the uterus to visualize the uterine cavity and detect any abnormalities.
- Digital and speculum examination, to visualize the cervix for any abnormality.
- Pelvic scan, to visualize pelvic organs and rule out any abnormality.
Management
The best management to investigate and treat the cause.
Medical and Nursing Management of Metrorrhagia:
- Hormonal therapy: Depending on the underlying cause, hormonal medications, such as birth control pills or progestin therapy, may be prescribed to regulate the menstrual cycle and reduce abnormal bleeding.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications can help manage pain and reduce bleeding during episodes of metrorrhagia.
- Treatment of underlying conditions: If metrorrhagia is caused by conditions such as fibroids, polyps, or infections, appropriate treatment strategies will be implemented to address the specific cause.
- Surgical interventions: In some cases, surgical procedures may be necessary to remove uterine abnormalities or address the underlying cause of metrorrhagia.
- Supportive care: Nursing management focuses on providing emotional support, educating patients about menstrual hygiene and symptom management, and promoting overall well-being.
- Monitoring and follow-up: Nurses play a vital role in monitoring patients\’ response to treatment, assessing the effectiveness of interventions, and ensuring appropriate follow-up care.
POLYMENORRHOEA/ EPIMENORRHPEA
Polymenorrhea, also known as epimenorrhoea, is a medical condition characterized by frequent menstrual periods that occur more frequently than the normal menstrual cycle. Also refers to menstruation periods that occurs at shorter intervals than usual (14-21 days), but they are frequent and regular.
Causes of Polymenorrhea/Epimenorrhoea:
- Hormonal imbalances: Fluctuations in estrogen and progesterone levels can disrupt the normal menstrual cycle and result in more frequent periods.
- Thyroid disorders: Overactive thyroid (hyperthyroidism) or underactive thyroid (hypothyroidism) can affect hormone production and menstrual regularity.
- Polycystic ovary syndrome (PCOS): This condition is characterized by hormonal imbalances, enlarged ovaries with cysts, and irregular menstrual cycles.
- Uterine abnormalities: Conditions such as uterine fibroids, polyps, or adenomyosis can cause abnormal bleeding and frequent periods.
- Stress and lifestyle factors: Chronic stress, excessive exercise, drastic weight changes, and poor nutrition can disrupt the hormonal balance and contribute to polymenorrhea.
Signs and Symptoms of Polymenorrhea/Epimenorrhoea:
- Menstrual cycles shorter than 21 days.
- More frequent periods, with menstrual bleeding occurring every two weeks or less.
- Lighter or heavier bleeding than usual.
- Increased menstrual discomfort or pain.
- Fatigue or tiredness due to frequent blood loss.
- Emotional and psychological impact, such as anxiety or mood swings.
Investigations for Polymenorrhea/Epimenorrhoea:
- Medical history and physical examination: A thorough evaluation of the menstrual patterns, symptoms, and any underlying medical conditions is conducted. A pelvic examination may be performed to assess the reproductive organs.
- Hormone level assessment: Blood tests may be done to measure hormone levels, including estrogen, progesterone, thyroid hormones, and other relevant hormones.
- Pelvic ultrasound: This imaging test can provide visual information about the ovaries, uterus, and any structural abnormalities.
- Endometrial biopsy: A sample of the uterine lining may be obtained and examined to rule out any abnormalities or cancer.
Medical and Nursing Management of Polymenorrhea/Epimenorrhoea:
- Hormonal therapy: Depending on the underlying cause, hormonal medications, such as oral contraceptives or hormone-regulating medications, may be prescribed to regulate the menstrual cycle and reduce the frequency of periods.
- Treatment of underlying conditions: If polymenorrhea is caused by conditions such as PCOS or uterine abnormalities, appropriate treatment strategies will be implemented to address the specific cause. Carry out dilatation and curettage (D&C) to remove retained products if its the cause.
- Lifestyle modifications: Stress reduction techniques, maintaining a balanced diet, regular exercise, and adequate sleep can help regulate hormonal balance and promote overall well-being.
- Supportive care: Nursing management focuses on providing emotional support, educating patients about menstrual hygiene, symptom management, and lifestyle modifications.
- Monitoring and follow-up: Monitoring patients\’ response to treatment, assessing the effectiveness of interventions, and ensuring appropriate follow-up care should be put into considerations.
DYSFUNCTIONAL UTERINE BLEEDING
Dysfunctional uterine bleeding (DUB) refers to abnormal uterine bleeding that occurs in the absence of organic causes or underlying medical conditions. It is typically characterized by irregular, prolonged, or heavy menstrual bleeding. Can also refers to abnormal bleeding resulting from hormonal changes rather than from trauma, inflammation, pregnancy or a tumour.
Incidence
The prevalence varies widely but an incidence 10% among patients attending the outpatient seems logical. The bleeding may be abnormal in frequency ,amount or duration or combination of both.
Causes
- It is due to sustained levels of oestrogen leading to thickening of the endometrium which shed incompletely and irregularly.
Pathophysiology
- In most cases, abnormal bleeding is caused by local causes in the endometrium.
- However,there is some disturbance of the endometrial blood vessels and capillaries and coagulation of blood in and around these vessels.
- These are caused by alteration in the ratio of endometrial prostaglandins which are delicately balanced in hemostasis of menstruation and may be related to incoordination in the hypothalamo-pituitary –ovarian axis.
Signs and Symptoms of Dysfunctional Uterine Bleeding:
- Irregular menstrual cycles: Menstrual periods may occur more frequently or infrequently than usual.
- Prolonged bleeding: Menstrual bleeding may last longer than the typical duration.
- Heavy menstrual bleeding: Excessive or abnormally heavy bleeding during menstrual periods.
- Intermenstrual bleeding: Bleeding that occurs between menstrual cycles.
- Fatigue or tiredness due to excessive blood loss.
- Anemia symptoms: Weakness, lightheadedness, shortness of breath, or pale skin.
NOTE : A diagnosis of dysfunctional uterine bleeding is made only when all other possibilities of causes of bleeding have been excluded.
Investigations
- Ultra sound scan to rule out new growth
- Blood analysis for hormonal imbalance
- Biopsy for histology
MANAGEMENT
- Treatment depends on various factors like age, condition of the uterine lining and the woman’s plans regarding pregnancy.
- Total hysterectomy is indicated if the woman is over 35 years, uterine lining thickened and contains abnormal cells and she does not want to become pregnant.
- When the uterine lining is thickened but contains normal cells, heavy bleeding may be treated with high dose of oral contraceptive oestrogen and progestin(COC) or oestrogen alone usually intravenously, then followed by a progestin given by mouth. Bleeding generally stops within 12-24 hours and then low doses of oral contraceptives may be given in usual manner for atleast 3 months.
- Women who have lighter bleeding may be given low doses from the start.
- If a woman has contraindications to oestrogen containing drug, progestin only pills may be given by mouth for 10-14 days each month.
- D&C may be used if response or hormonal therapy proves ineffective.
- If a woman wants to become pregnant, clomiphene drug may be given orally to induce ovulation.
ENDOMETRIOSIS
Endometriosis is a chronic and often painful condition in which tissue similar to the lining of the uterus, called the endometrium, grows outside the uterus. This abnormal tissue growth can occur in various areas of the reproductive system, such as the ovaries, fallopian tubes, and pelvic lining.
Can also refer to growth or presence of endometrial tissue outside the uterus. It may be referred to as a misplaced endometrial tissue.
Incidence
- 10-15% of women between 25 and 45 years. 25-50% in infertile women.
Common sites that may be affected
Abdominal organs, ovaries, ligaments, intestines, ureters, urinary bladder, vagina, vulva, naval, lungs, nose, conjunctiva and rarely on normal skin.
Cause
The actual cause is not known. But has the following predisposing factors.
- Retrograde menstruation: One possible cause is the backward flow of menstrual blood into the fallopian tubes and pelvic cavity, allowing endometrial tissue to implant and grow outside the uterus.
- Hormonal imbalance: Estrogen may play a role in promoting the growth of endometrial tissue outside the uterus.
- Genetic factors: Having a close relative with endometriosis increases the risk of developing the condition.
- Immune system dysfunction: A weakened immune response may allow the abnormal growth and survival of endometrial tissue outside the uterus.
- Environmental factors: Exposure to certain chemicals and toxins may contribute to the development of endometriosis.
- Surgery involving the uterus like C/S, D&C.
- Too late prime para (over 30 years)
- Genetic makeup (tend to run in families) especially first degree relatives like mother, sister, daughter.
- Race-common in Caucasians
- Abnormal uterus like retroverted uterus
Signs and symptoms
- Some are asymptomatic
- Lower abdominal pain
- Irregular periods like spotting before periods
- Infertility
- Painful coitus (dyspareunia)
- Pain during bowel opening
- Rectal bleeding during menstruation. This is due to the presence of endometrial tissue in the rectum.
- Bleeding from the site during menstruation
- Palpable mass (endometrioma)
- Adhesions
Diagnosis / investigations
- Presence of endometrial tissue in the site after microscopic examinations confirms the disease (biopsy)
- To view the tubes and ovaries for the presence of endometrial tissue.
- Ultra sound scan. To visualize pelvic organs for any abnormality.
- Barium enema with x-ray. To locate the site of the tissue.
- Computerized Tomography (CT ) scan. To visualize the tissue.
- Magnetic Resonance Imaging (MRI ).
- Blood for marker cell (CA-125 ) and antibodies to endometrial tissue.
- Medical history and symptom assessment: The healthcare provider will discuss the patient\’s symptoms, menstrual patterns, and medical history.
- Pelvic examination: A pelvic exam may be performed to check for abnormalities or areas of tenderness.
- Imaging tests: Transvaginal ultrasound or MRI may be used to visualize the pelvic organs and detect the presence of endometrial growths.
- Laparoscopy: This minimally invasive surgical procedure allows for direct visualization and biopsy of the abnormal tissue, confirming the diagnosis of endometriosis.
Nursing, Medical, and Surgical Management of Endometriosis:
- Pain management: Provide education on pain management strategies, including the use of over-the-counter pain relievers or prescribed medications.
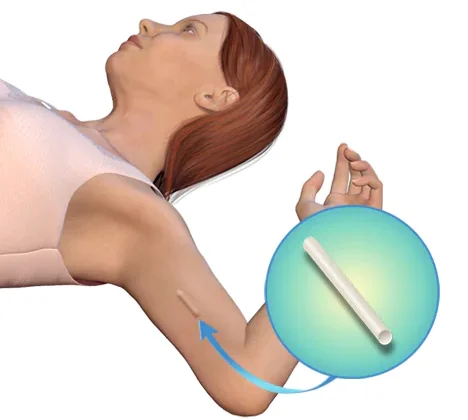
- Hormonal therapy: Medications such as birth control pills, hormonal patches, or progestin-only therapies may be prescribed to regulate the menstrual cycle and reduce symptoms.
- Drugs that suppress the activity of ovaries and slow the growth of endometrial tissue like COCs, progestin and GnRH agonists.
- Surgical intervention: In cases of severe pain or infertility, laparoscopic surgery may be performed to remove or destroy endometrial growths. Surgical intervention is primarily to remove as much of the misplaced endometrium tissue as possible
- Combination of drugs and surgery or Total hysterectomy when all other treatments fail.
- Fertility treatments: Assisted reproductive technologies, such as in vitro fertilization (IVF), may be recommended for individuals experiencing infertility due to endometriosis.
- Supportive care: Provide emotional support, educate patients about the condition, and help individuals cope with the physical and emotional challenges associated with endometriosis.
Complications of Endometriosis:
- Infertility: Endometriosis can affect fertility by causing scarring, adhesions, and structural abnormalities in the reproductive organs.
- Ovarian cysts: Endometriomas, also known as \”chocolate cysts,\” can form on the ovaries and may require surgical removal.
- Adhesions: Endometriosis can lead to the formation of scar tissue, causing organs and tissues to stick together.
- Chronic pain: Severe and persistent pelvic pain can significantly impact a person\’s quality of life.
MENSTRUAL DISORDERS Read More »