COMMON COLD/CORYZA
Introduction
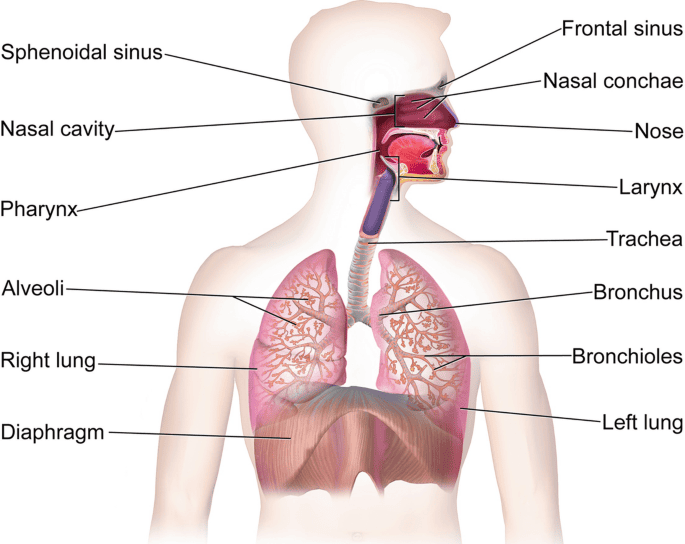
It is the acute inflammation of the upper respiratory tract; rhinitis (nasal mucosa) and rhinopharyngitis (nasal and pharyngitis).
Causes of common cold
- The most common virus is rhinovirus. Other viruses include the influenza virus, adenovirus, enterovirus, and respiratory syncytial virus.
- Bacteria may cause roughly 15% of sudden onset pharyngitis presentations. The most common is S. pyogenes, a Group A streptococcus.
Clinical manifestations
Manifestations of common cold infection typically appear after an incubation period of 12-72 hours and last 7-11 days, but may persist for longer.
Signs and symptoms include the following:
- Nasal dryness or irritation - May be first symptom
- Sore throat or throat irritation – Common and bothersome initial symptom
- Nasal discharge, nasal congestion, and sneezing – Intensify over 2-3 days
- Headache
- Facial and ear pressure
- Loss of sense of smell and taste
- Cough (30% of infected individuals)
- Hoarseness (20%)
- Irritability or restlessness
- Fever (unusual; when present, typically low grade)
- Tiredness with slight pyrexia
- General malaise
- Mild conjunctivitis
- Anorexia
- Loss of or swollen enlarged lymph nodes
Test and Diagnosis
History taking and physical examination – include the following:
- Inspection of the nose and ears to check for any other possible sites of infection.
- Inspection of the skin for any rash related to scarlet fever to rule out the condition.
- Palpation of the lymph nodes around the neck.
- Auscultation to listen to the patient’s breathing and heart sounds.
- In some cases, mononucleosis may be ruled out as it can also cause inflammation of the tonsils.
Other diagnostic tests may be performed as follow:
- Throat swab – a sterile swab rubbed over the throat will be sent to the lab to check for streptococcal bacteria and the need for antibiotics.
- Complete blood count – to show the presence of either a viral or bacterial infection depending on what blood cell is elevated.
- Because of the prolonged time to obtain positive culture findings, rhinovirus culture has rarely been found useful in clinical settings.
- PCR testing of respiratory specimens may be useful in evaluating severely immunocompromised patients.
DIFFERENTIAL DIAGNOSIS
- Rhinitis
- Early signs of measles
- An allergy
- Whooping cough
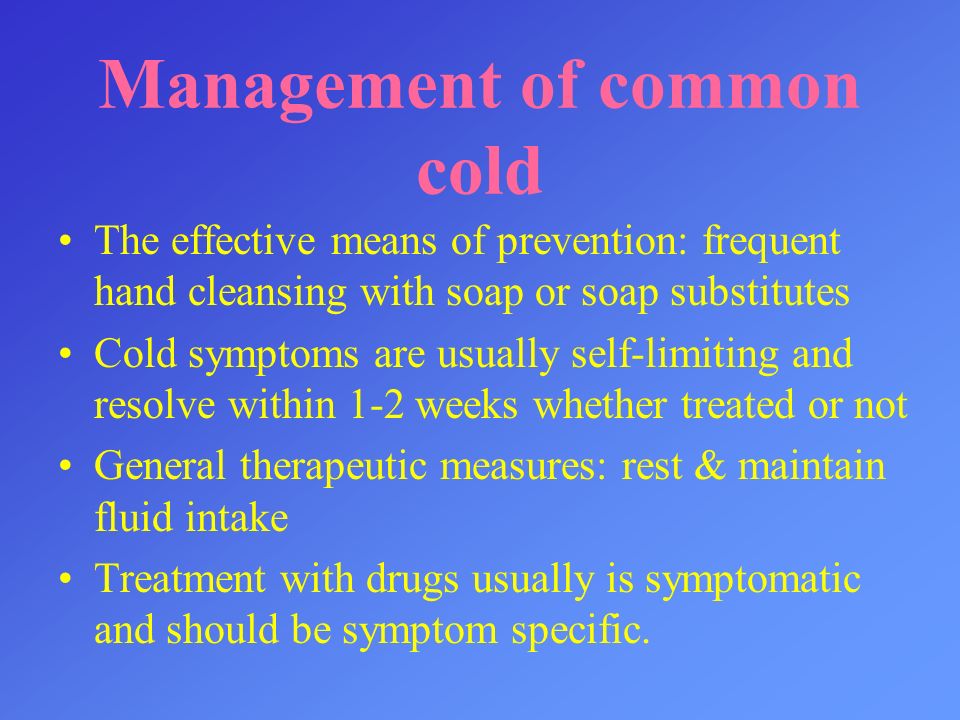
Management of Common Cold
The common cold is primarily a self-limiting viral infection, and treatment is mainly supportive, focusing on relieving symptoms.
Aims of management
Symptomatic Relief:
When to Seek Medical Attention:
While most common colds resolve on their own, it's important to seek medical advice if you experience any of the following:
- Symptoms that worsen or do not improve after 7-10 days.
- High fever (above 103°F or 39.4°C).
- Severe sore throat, especially if it's sudden and without other cold symptoms.
- Swollen glands in the neck or jaw.
- Significant sinus pain.
- Shortness of breath, wheezing, or difficulty breathing.
- Chest pain.
- Earache.
- New or worsening headache.
- Symptoms in infants (e.g., difficulty breathing, unusual drowsiness, refusal to feed).
- Weakened immune system due to other conditions (e.g., HIV, cancer treatment).
Medical Management
Common cold is a viral disease which needs only symptomatic treatment and no antibiotics are needed.
Antibiotics:
Antibiotics are ineffective against viral infections, including the common cold. They are only prescribed if a bacterial complication, such as a bacterial sinus infection or strep throat, is diagnosed.
Drug therapy
- NSAIDS
- Antihistamines
- Corticosteroids
- Nasal decongestants
Nursing interventions/management
1. Assessment of the patient
- a. Carrying out history of the presenting signs and symptoms e.g. fever, flue among others.
- b. Taking vital observation e.g. TPR/BP and general examination to exclude other diseases.
- c. Alerting the doctor who will order for investigations and admission, there the nurse will assist the patient throughout the process.
2. Managing fever
- a. Assess the patient’s vital signs at least every 4 hours.
- b. Remove excessive clothing, blankets, and linens. Adjust the room temperature.
- c. Administer the prescribed antibiotic and anti-pyretic.
- d. Offer a tepid sponge bath.
- e. Elevate the head of the bed.
3. To relieve headache, joint pains, flue and cough
- a. Assess the patient’s vital signs and characteristics of pain at least 30 minutes after administration of medication.
- b. Elevate the head of the bed and position the patient in semi Fowler’s.
- c. Encouraging patient to sneeze into the elbow not in the hand.
- d. Must were a mask most time.
- e. Should be isolated until he improves.
- f. Encouraging patients to take soothing fluids like warm water and honey or lemon.
- g. Administer cough suppressants, antibiotics and analgesics as prescribed.
- h. Encourage patients to verbalise feeling of pain.
- i. Measure the pain compliants of patients using a pain scale.
- j. Encourage patients to take more fluids at least 3 liters.
4. Prevention of complication
- a. Assess the patient’s vital signs and characteristics of respirations at least every 4 hours. Assess for signs of hypoxia.
- b. Place the patient on a side-lying or prone position.
- c. Suction secretions.
- d. Positioning the mattress at a 45° angle.
- e. Discontinuing smoking or using alcohol.
- f. Administer the prescribed medications (e.g. corticosteroids) and antibiotic medications.
5. To prevent infection
- a. Teach the patient
- i. Self isolation
- ii. Wearing masks while in public
- iii. Maintain social distance
- b. Assess vital signs and observe for any signs of infection as well as for any signs of respiratory distress.
- c. Perform a focused assessment on the oropharyngeal region, particularly checking for any collection of abscess.
- d. Teach the patient how to perform proper hand hygiene.
- e. Administer antibiotics as prescribed.
- f. Disinfecting the environment using phenol-alcohol–based compounds.
- g. Washing hands.
6. Health education of the patients
- a. Educating the patient about wearing mask, maintaining hand hygiene.
- b. Educating the patients about the disease.
7. Discharge advice
- a. Encourage proper hand hygiene, wearing masks.
- b. Encourage proper adherence to drugs.
- c. Inform the patient about the follow up date and encourage the patient to attend.
Prevention of Common Cold
While there is no vaccine for the common cold, certain measures can help prevent its spread:
- Frequent handwashing: Wash hands thoroughly with soap and water for at least 20 seconds, especially after coughing, sneezing, or blowing your nose, and before eating. Hand sanitizers with at least 60% alcohol can be used when soap and water are not available.
- Avoid touching face: Try to avoid touching your eyes, nose, and mouth, as viruses can enter the body through these routes.
- Stay away from sick people: Maintain distance from individuals who are ill with a cold.
- Clean and disinfect surfaces: Regularly clean and disinfect frequently touched surfaces, such as doorknobs, phones, and keyboards, especially when someone in the household is sick.
- Boost your immune system: A healthy lifestyle, including a balanced diet, regular exercise, adequate sleep, and stress management, can help strengthen your immune system.
- Use tissues: Cover your mouth and nose with a tissue when you cough or sneeze, then dispose of the tissue immediately. If a tissue isn't available, cough or sneeze into your elbow.
COMPLICATION
- Sinusitis
- Lower respiratory tract infection (LRTI) e.g pneumonia
- Deafness
- Otitis media
- Headache
- Acute tonsillitis
- Chronic bronchitis
- Exacerbations of reactive airway disease (e.g. asthma)
