Table of Contents
ToggleCONGESTIVE CARDIAC FAILURE (CCF), OR HEART FAILURE (HF)
Introduction to Heart Failure
Heart failure (HF), often referred to as congestive heart failure (CHF) particularly when fluid retention is prominent, is a complex clinical syndrome resulting from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. Essentially, the heart cannot pump enough blood to meet the metabolic demands of the body's tissues for oxygen and nutrients.
- It is not that the heart has "failed" or stopped working, but rather that it is not working as efficiently as it should.
- HF is a progressive condition that can worsen over time.
- The term "congestive" reflects the common symptom of fluid accumulation (congestion) in the lungs and/or other body tissues when the heart's pumping action is inefficient.
- While "CCF" specifically points to the congestion, "Heart Failure" is the more encompassing and commonly used term in modern medical practice, as not all forms of heart failure present with overt congestion initially.
- It is a syndrome, meaning it is a collection of signs and symptoms, rather than a single disease, often the end-stage of many cardiovascular diseases.
Types of Heart Failure
Heart failure can be classified based on which side of the heart is primarily affected, the ejection fraction, and its onset.
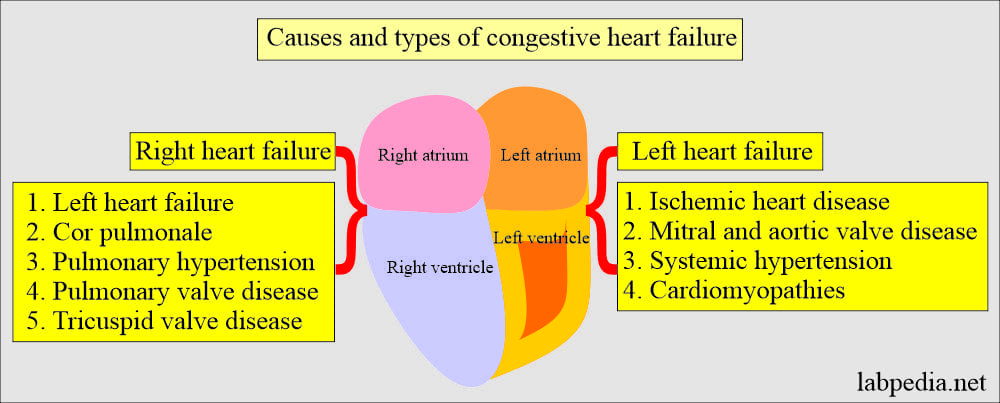
I. Based on Affected Side:
Heart failure can affect the left side, right side, or both.
A. Left-Sided Heart Failure:
Occurs when the left ventricle fails to pump blood effectively to the body. This leads to blood backing up into the lungs.
- Systolic Heart Failure (HFrEF - Heart Failure with reduced Ejection Fraction): The left ventricle loses its ability to contract normally. The heart muscle becomes weak and enlarged, and it can't pump enough blood into circulation. Characterized by an ejection fraction (EF) of <40-50%.
- Diastolic Heart Failure (HFpEF - Heart Failure with preserved Ejection Fraction): The left ventricle becomes stiff and cannot relax or fill properly during diastole (the resting phase between beats). Although the pumping ability (ejection fraction) may be normal, the heart cannot fill with enough blood, leading to reduced cardiac output. Characterized by an EF of ≥50% but with evidence of diastolic dysfunction.
B. Right-Sided Heart Failure:
Occurs when the right ventricle fails to pump blood effectively to the lungs. This causes blood to back up into the systemic circulation.
- Mechanism: The right ventricle's inability to effectively pump blood into the pulmonary artery leads to increased pressure in the right atrium and systemic veins. This increased pressure causes fluid to accumulate in the body's tissues.
- Causes: Most commonly caused by left-sided heart failure (as the increased pressure in the lungs eventually overworks and weakens the right ventricle). Other causes include chronic lung diseases (e.g., COPD leading to cor pulmonale), pulmonary hypertension, and specific right ventricular pathologies.
- Key Symptom: Fluids may back up in the abdomen (ascites), liver (hepatomegaly), legs, and feet causing swelling (peripheral edema).
C. Biventricular Heart Failure:
Occurs when both the left and right ventricles are impaired. This is a common progression of heart failure, as failure of one side often places increased strain on the other. It presents with a combination of symptoms from both left and right-sided heart failure.
II. Based on Onset:
- Acute Heart Failure: Rapid onset or worsening of heart failure symptoms. Can be a first presentation or an acute decompensation of chronic HF. Often triggered by an acute event (e.g., myocardial infarction, arrhythmia, severe infection).
- Chronic Heart Failure: A long-term condition with ongoing symptoms that may gradually worsen over time, often managed with medication and lifestyle changes. Patients may experience acute exacerbations (decompensations).
Causes and Risk Factors of Heart Failure
Heart failure is often the result of other chronic conditions that damage or overwork the heart. It's important to differentiate between primary causes and aggravating factors.
A. Primary Causes (Conditions that directly damage the heart or increase its workload):
- CAD: Narrowing of the arteries supplying the heart muscle reduces blood flow, leading to ischemia and chronic damage.
- MI (Heart Attack): Sudden blockage of a coronary artery causes death of heart muscle tissue. The scarred tissue cannot pump effectively.
- Sustained high blood pressure increases the workload on the heart, causing the heart muscle (especially the left ventricle) to thicken and become stiff (hypertrophy). Over time, this can lead to the heart becoming less efficient and eventually failing.
- Stenosis (Narrowing): A valve doesn't open fully, forcing the heart to pump harder to push blood through (e.g., Aortic Stenosis).
- Regurgitation (Leakage/Insufficiency): A valve doesn't close completely, allowing blood to flow backward, increasing the heart's workload (e.g., Mitral Regurgitation).
- Diseases of the heart muscle itself, often genetic or idiopathic. These can cause the heart muscle to become dilated (stretched and thin), hypertrophic (abnormally thick), or restrictive (stiff). HF due to cardiomyopathy is usually chronic and progressive.
- Hyperthyroidism: Overactive thyroid can make the heart beat too fast and too hard.
- Hypothyroidism: Underactive thyroid can slow metabolism and contribute to other risk factors.
B. Aggravating Factors (Can precipitate or worsen heart failure):
- Smoking (Tobacco Use): Damages blood vessels and contributes to CAD and hypertension.
- Obesity: Increases the workload on the heart and is associated with hypertension, diabetes, and sleep apnea.
- Excessive Alcohol Consumption: Can directly damage heart muscle (alcoholic cardiomyopathy).
- High Sodium Diet: Leads to fluid retention, increasing blood volume and heart workload.
- Lack of Physical Activity.
Clinical Manifestations / Signs and Symptoms of Heart Failure
Symptoms vary depending on whether left or right-sided failure predominates, the severity, and the acuteness of the condition. They generally result from inadequate cardiac output and/or compensatory fluid retention.
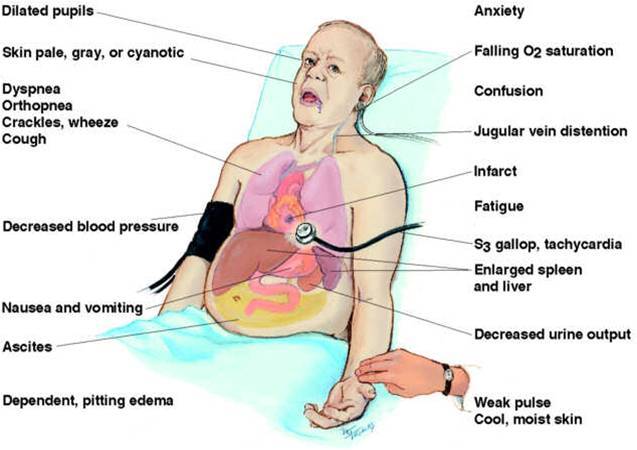
I. Symptoms of Left-Sided Heart Failure (Pulmonary Congestion):
- Dyspnea (Shortness of Breath):
- Exertional Dyspnea: Occurs with activity, initially mild, progresses to severe.
- Orthopnea: Difficulty breathing when lying flat, relieved by sitting up (requires extra pillows to sleep).
- Paroxysmal Nocturnal Dyspnea (PND): Sudden awakening at night with severe shortness of breath, relieved by sitting upright or standing.
- Dyspnea at Rest: In advanced stages.
- Cough: May be initially dry and irritating, later becoming productive of frothy, sometimes pink-tinged (blood-stained) sputum due to pulmonary edema. Worse at night or when lying down.
- Crackles (Rales): Heard on auscultation of the lungs, indicative of fluid in the alveoli.
- Wheezing: Can occur due to bronchial edema.
- Tachypnea: Increased respiratory rate.
- S3 Gallop: An extra heart sound heard on auscultation, indicative of rapid ventricular filling in a dilated ventricle.
- Reduced Exercise Tolerance/Activity Intolerance: Due to insufficient oxygen delivery to muscles.
- Fatigue and Weakness: Due to decreased cardiac output and poor tissue perfusion.
- Nocturia: Increased urination at night, as supine position improves renal perfusion.
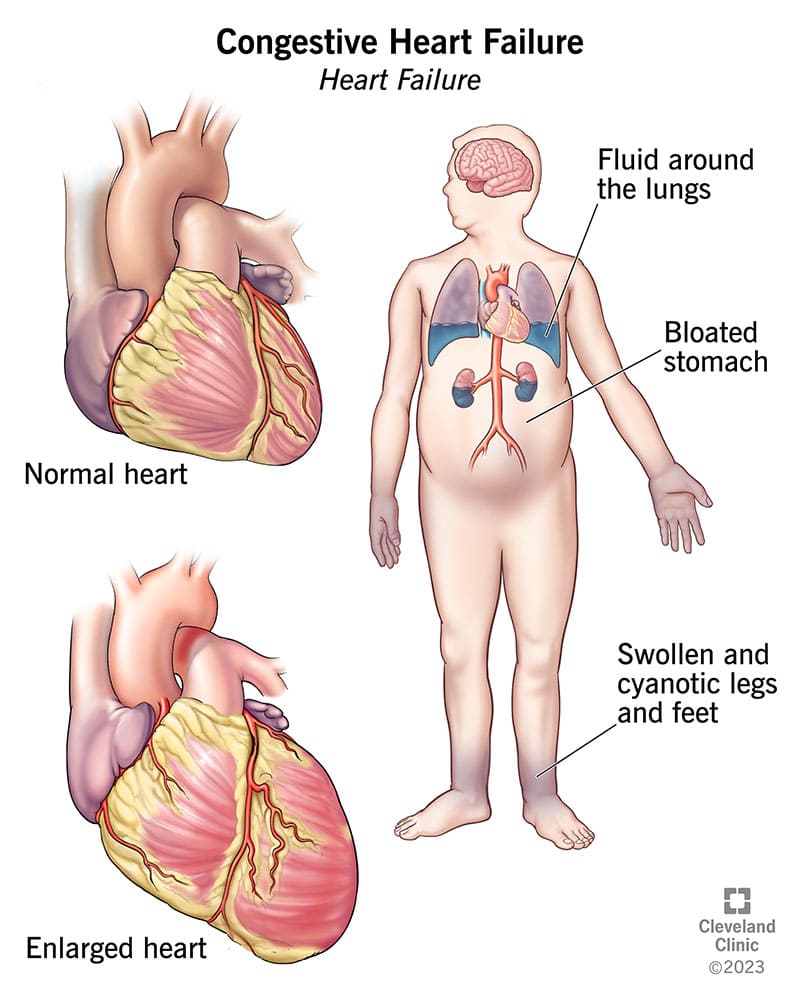
- Pulmonary Edema: Severe accumulation of fluid in the lungs, leading to acute respiratory distress (medical emergency).
- Cyanosis: Bluish discoloration of skin, lips, and nail beds in severe cases due to poor oxygenation.
II. Symptoms of Right-Sided Heart Failure (Systemic Congestion):
- Peripheral Edema: Swelling, mainly of the lower limbs (ankles, feet, sacrum if bedridden), often pitting. Worse at the end of the day.
- Jugular Venous Distension (JVD): Visible swelling and pulsation of the jugular veins in the neck due to increased pressure in the right atrium.
- Hepatomegaly: Enlargement of the liver due to venous congestion, leading to right upper quadrant pain or tenderness.
- Ascites: Fluid accumulation in the peritoneal space, causing abdominal distension and discomfort.
- Anorexia, Nausea, and Vomiting: Due to congestion of the gastrointestinal tract and liver, leading to feeling of fullness and impaired digestion.
- Weight Gain: Due to fluid retention, despite potential muscle wasting.
- Splenomegaly: Less common than hepatomegaly, but spleen can also enlarge due to congestion.
- Heartburn and Feeling of Indigestion: Non-specific, but can be related to GI congestion.
- Constipation: Can be related to reduced activity, dietary changes, or medication side effects.
III. General Symptoms (Can occur in both or biventricular failure):
- Fatigue and Weakness: As mentioned, common in all types due to reduced cardiac output.
- Activity Intolerance: Difficulty performing daily activities like walking, climbing stairs, digging, carrying.
- Anxiety and Restlessness: Often due to dyspnea or general discomfort.
- Irritability: Can be a consequence of chronic illness and discomfort.
- Rapid or Irregular Pulse Rate (Tachycardia/Arrhythmias): Heart tries to compensate by beating faster.
- Palpitations: Awareness of heart beats.
- Oliguria (Reduced Urine Output) / Anuria (Total Urine Absence): During the day due to decreased renal perfusion, but often followed by nocturia as renal perfusion improves at rest.
- Confusion or Memory Impairment: In severe cases, due to reduced cerebral perfusion.
- Weight Loss (Cardiac Cachexia): In advanced, chronic HF, despite fluid retention, due to metabolic derangements and protein-calorie malnutrition, leading to prominent ribs.
- Anemia: Can be a co-morbidity or contribute to worsening HF.
- Chest Pain: While more typical of ischemia, can occur with severe heart failure due to increased myocardial oxygen demand.
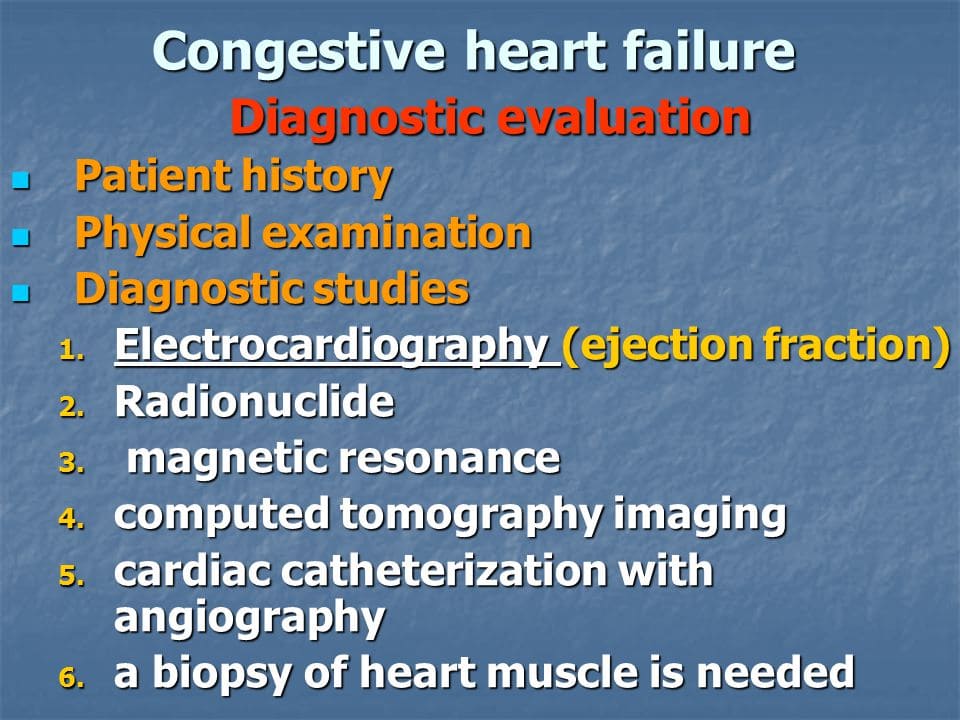
Investigations and Diagnosis of Heart Failure
Diagnosis of heart failure is a clinical diagnosis based on symptoms, physical examination, and confirmed by objective tests.
A. Clinical Assessment:
- Assessment of vital signs (tachycardia, tachypnea, hypotension or hypertension).
- Presence of edema (pitting, non-pitting).
- JVD.
- Lung auscultation (crackles, wheezes, diminished breath sounds if pleural effusion).
- Heart auscultation (murmurs, S3 gallop, irregular rhythm).
- Abdominal examination (hepatomegaly, ascites).
- Skin turgor, color (pallor, cyanosis).
B. Laboratory Tests:
- Complete Blood Count (CBC): To check for anemia, infection.
- Serum Electrolytes (Na, K, Mg): To assess for imbalances, especially if on diuretics.
- Renal Function Tests (Creatinine, BUN): To assess kidney function, which can be affected by HF or medications.
- Liver Function Tests (LFTs): To assess for hepatic congestion.
- Thyroid-Stimulating Hormone (TSH): To rule out thyroid dysfunction as a cause or contributing factor.
- B-type Natriuretic Peptide (BNP) or N-terminal pro-BNP (NT-proBNP):
- Purpose: Hormones released by the heart ventricles in response to stretching and increased pressure.
- Significance: Elevated levels are highly suggestive of heart failure and correlate with its severity. Useful for diagnosis, prognosis, and monitoring treatment effectiveness.
- Cardiac Biomarkers (Troponins): May be elevated in acute heart failure due to myocardial stress, or if underlying ischemic event.
- Fasting Blood Glucose/HbA1c: To check for diabetes.
- Lipid Profile: To assess for risk factors of CAD.
- Blood for Culture and Sensitivity: If infection is suspected as a precipitating factor.
C. Imaging and Other Diagnostic Tests:
- Purpose: To check heart rhythm, identify previous heart attacks, signs of chamber enlargement, or ischemia.
- Findings: May show arrhythmias (e.g., atrial fibrillation), signs of past MI (Q waves), ventricular hypertrophy, conduction abnormalities. While not diagnostic of HF itself, it provides valuable information about underlying causes.
- Purpose: To visualize the size and shape of the heart and check for pulmonary congestion.
- Findings: May reveal cardiomegaly (enlarged heart), pulmonary vascular congestion, interstitial edema, pleural effusions (fluid around the lungs). These images show the condition of the heart and lungs.
- Purpose: The most crucial diagnostic test for heart failure. It uses sound waves to create moving images of the heart.
- Information Provided:
- Ejection Fraction (EF): Measures the percentage of blood pumped out of the ventricle with each beat, differentiating HFrEF from HFpEF.
- Chamber Size and Function: Assesses ventricular and atrial dimensions, wall thickness, and contractility.
- Valvular Function: Identifies structural or functional abnormalities of heart valves (stenosis, regurgitation).
- Pericardial Effusions.
- Estimates Pulmonary Artery Pressure.
- Purpose: To evaluate for underlying ischemic heart disease, especially if the cause of HF is unclear. Determines how the heart responds to exertion.
- Purpose: Provides highly detailed images of the heart's structure and function, particularly useful for evaluating cardiomyopathies, scar tissue, or complex congenital heart disease.
- Purpose: Invasive procedure to directly measure pressures within the heart chambers and identify blockages in the coronary arteries.
- Indications: Considered if CAD is suspected as a cause, or before surgical interventions.
Management:
Aims:
- To rest the patient- mentally and physically
- To relieve symptoms
- To prevent complications
Nursing Interventions / Management
- Admit patient on a medical ward in a well-ventilated room which is quiet near the nurse's station for close monitoring.
- Give a complete bed rest to rest the heart.
- Position the patient in a sitting up position to aid breathing, to relieve pressure of fluids in the lungs (fluid gravity).
- Loosen anything of constrictive nature from the patient's body to aid breathing and promote comfort.
- Use a bed cradle to lift the weight of beddings off the patient.
- Observations - vital observations i.e. Pulse, respirations, temperature, and blood pressure must be measured 4 hourly and accurately recorded in the patient's file. Pulse may be done more frequently. Observe assess patient for oedema, respiratory status and signs of cyanosis. Continuous pulse oximetry is needed.
- Provide a cardiac table to help the patient relax.
- Administer oxygen 2-5 litres to support breathing and correct cyanosis.
- Psychotherapy - patient and patient's relative are reassured to allay anxiety. This is started right from the time of admission up to discharge, always attend to patient's queries/questions and if possible stay with the patient.
- Support the patient's feet with a foot rest (small pillows) to prevent foot drop.
- Place a soft cushion beneath the oedematous sacral area to relieve pressure.
- Daily weighing of the patient to assess oedema and Ascites improvement.
- Provide a loose jacket or shawl to cover the patient in order to keep him/her warm.
- Hygiene - in acute phase of CCF, everything is done for the patient like bed bath, mouth care regular pressure area treatment especially the oedematous areas. Provide a sputum mug with disinfectant for expectoration, which must be regularly emptied, cleaned and kept covered.
- Diet - provide a highly nutritious diet with less sugar and carbohydrates (starch) which require a lot of energy metabolism. Provide a salt and fat free diet; give plenty of fruits, and vegetables/roughages to prevent constipation. Give little food at a time but frequently to avoid a distended stomach or abdomen.
- Restrict fluids in oedema; however give adequate amount of fluids.
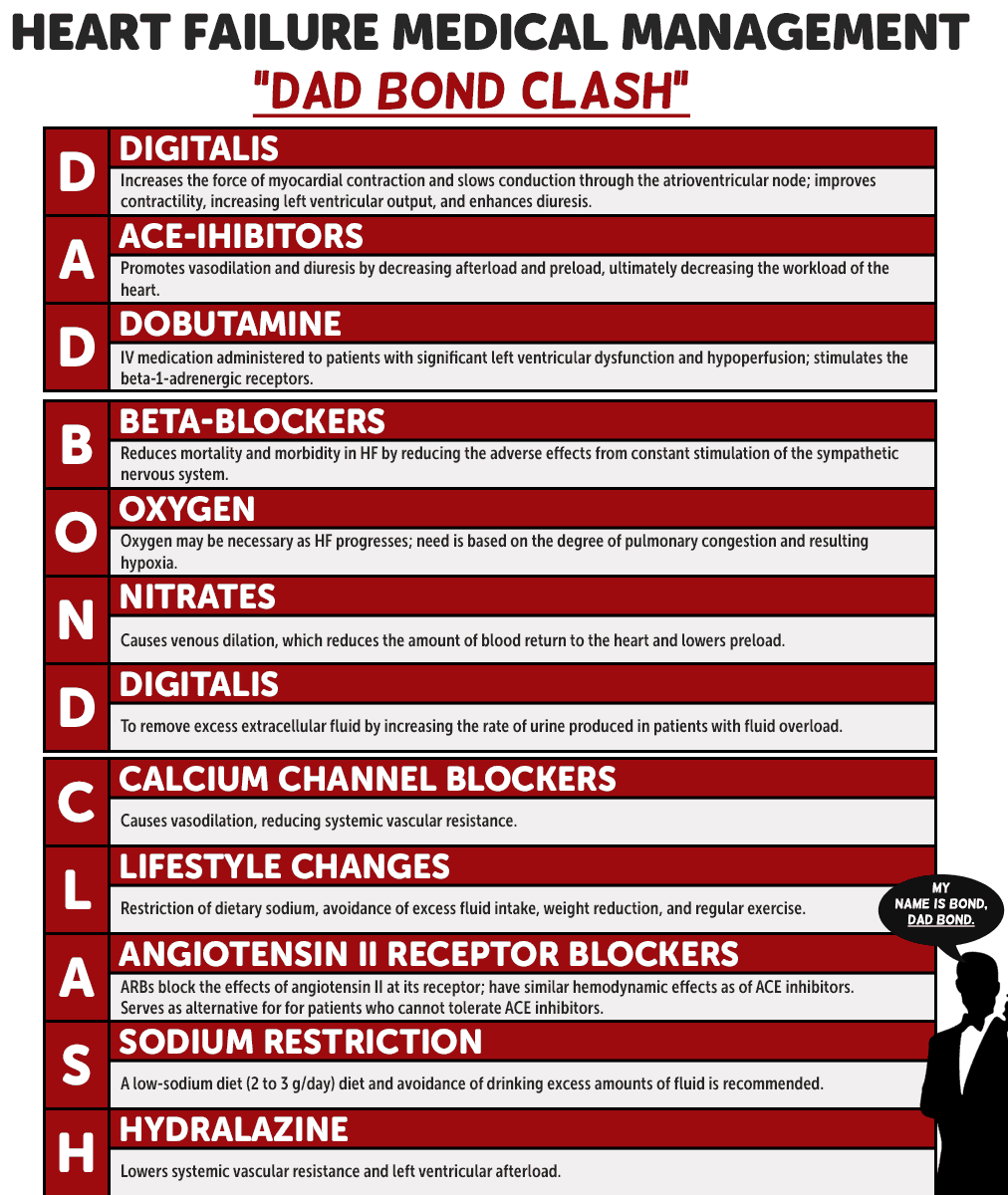
- Drug therapy:
- Digitalis group - like digoxin. Digitalis help to strengthens the heart and reduce on the contractility and conductivity of the heart. NB: digoxin should not be given when the pulse rate is < 60 b/m as it causes bradycardia.
- Diuretics - to promote renal excretion of salt and water thus correcting oedema. These include: furosemide, Bendrofluazide, Potassium sparing diuretics.
- Hypotensive - to normalize the blood pressure if high like: ACE inhibitors like captoprile, Beta blockers.
- Sedatives – like diazepam or phenytoin to promote rest and sleep.
- Supportive drugs like Haematenics e.g. Ferrous sulphate to prevent or treat anaemia, multivitamins to stimulate appetite.
- Abdominal paracentesis to relieve abdominal pressure caused by Ascites.
- Exercises – initially passive and when condition improves, active exercises can be commenced.
- Bladder and bowel care - fluid balance chart must be strictly monitored and balanced every after 24 hours to assess kidney function. Provide roughages and fruits with just enough fluids to avoid constipation.
- Health education: health educate patient and the patient's relative about:
- The nature of the disease and how it's managed in the hospital and at home.
- To adopt and comply with a cardiac diet- salt and fat free diet.
- About the drugs, how to take them and then drug compliance.
- To maintain a complete bed rest and the condition improves to carry out less strenuous exercises.
- To reduce or stop all the predisposing factors to cardiac failure (CCF) like stopping smoking, reduce weight (obesity) control DM, stop/reduce high fat diet.
- Vaccination of all patients against pneumococcal diseases, influenza, measles etc.
- Return to the hospital for review on the appointed date.
- NB: All mothers with cardiac failure (CCF) who want to conceive again must first consult their Cardiologists before conception.
Complications of Heart Failure
Heart failure is a progressive condition that can lead to various serious complications due to the body's compensatory mechanisms and the ongoing inability of the heart to pump effectively.
- Acute Pulmonary Edema: A life-threatening condition where fluid rapidly accumulates in the lung alveoli, causing severe shortness of breath, hypoxia, and respiratory distress. Requires immediate medical intervention.
- Kidney Damage or Failure: Chronic poor blood flow to the kidneys (due to low cardiac output) and the effects of medications (e.g., diuretics, ACE inhibitors) can impair kidney function, sometimes leading to cardiorenal syndrome.
- Liver Damage: Chronic venous congestion in right-sided heart failure can lead to liver enlargement (hepatomegaly) and impaired liver function (cardiac cirrhosis in severe, long-standing cases).
- Cardiac Arrhythmias: The stretched and damaged heart muscle is more prone to developing abnormal heart rhythms, including atrial fibrillation (very common), ventricular tachycardia, and ventricular fibrillation (life-threatening). These can further reduce cardiac output and increase the risk of sudden cardiac death.
- Valvular Heart Disease: As the heart chambers enlarge, the valves (especially the mitral and tricuspid valves) may become stretched and unable to close properly, leading to regurgitation (functional mitral or tricuspid regurgitation), which can worsen the heart failure.
- Stroke: Patients with heart failure, particularly those with atrial fibrillation, are at increased risk of blood clot formation within the heart chambers. These clots can dislodge and travel to the brain, causing an ischemic stroke.
- Pulmonary Hypertension: Left-sided heart failure often leads to increased pressures in the pulmonary arteries, which can eventually cause pulmonary hypertension and further strain the right ventricle.
- Anemia: Common in chronic heart failure due to various factors including chronic inflammation, kidney dysfunction, and nutritional deficiencies. Anemia can worsen HF symptoms.
- Malnutrition/Cardiac Cachexia: In advanced stages, patients may experience significant weight loss and muscle wasting (cardiac cachexia) due to increased metabolic demands, malabsorption from gut edema, and anorexia.
- Depression and Anxiety: The chronic and debilitating nature of heart failure can significantly impact a patient's mental health, leading to depression and anxiety, which can further affect self-care and quality of life.
- Increased Risk of Infections: Patients with chronic conditions like HF may be more susceptible to infections, especially respiratory infections like pneumonia, which can trigger acute decompensation.
Nursing Diagnoses for Heart Failure
Nursing diagnoses provide a framework for nursing care, identifying patient problems that nurses can independently address. Here are common nursing diagnoses for patients with heart failure:
- Decreased Cardiac Output related to altered contractility, altered preload, altered afterload, and/or altered heart rate/rhythm, as evidenced by dyspnea, fatigue, weakness, peripheral edema, S3 gallop, JVD, and altered blood pressure.
- Excess Fluid Volume related to compromised regulatory mechanisms (e.g., decreased kidney perfusion, increased ADH) and increased sodium/water retention, as evidenced by peripheral edema, pulmonary congestion (crackles, dyspnea, orthopnea), weight gain, and JVD.
- Impaired Gas Exchange related to alveolar-capillary membrane changes (fluid accumulation in lungs), as evidenced by dyspnea, tachypnea, abnormal blood gases, and crackles.
- Activity Intolerance related to imbalance between oxygen supply and demand, generalized weakness, and deconditioning, as evidenced by dyspnea on exertion, fatigue, and inability to perform activities of daily living (ADLs).
- Fatigue related to decreased cardiac output, inadequate tissue oxygenation, increased metabolic demands, and sleep disturbance (e.g., PND, nocturia), as evidenced by overwhelming sustained sense of exhaustion, decreased performance, and lethargy.
- Imbalanced Nutrition: Less Than Body Requirements related to anorexia, nausea, early satiety (from GI congestion), and increased metabolic demands, as evidenced by weight loss, muscle wasting, and abnormal laboratory values.
- Excessive Anxiety related to change in health status, perceived threat to self-concept, potential for death, and shortness of breath, as evidenced by restlessness, expressed concerns, and sympathetic nervous system manifestations.
- Deficient Knowledge regarding disease process, dietary and fluid restrictions, medication regimen, signs and symptoms of worsening condition, and self-care activities, as evidenced by verbalized questions, inaccurate follow-through of instructions, or exacerbation of symptoms.
- Risk for Impaired Skin Integrity related to edema, decreased tissue perfusion, and immobility, as evidenced by (potential for) skin breakdown in dependent areas.
- Risk for Ineffective Self-Health Management related to complexity of therapeutic regimen, perceived barriers, lack of motivation, or insufficient social support.
- Ineffective Breathing Pattern related to fluid shift into interstitial spaces/alveoli, as evidenced by dyspnea, orthopnea, tachypnea, and use of accessory muscles.

