Table of Contents
ToggleFAMILY PLANNING
Family planning is defined as the practice of having children by choice and not by chance.
Family planning is defined as a process through which individuals, couples make an informed choice on how many children to have, when to have and how often to have so that each child born is expected and properly catered for in all ways.
Family planning policy does not discriminate against men; they also have great roles to play for the success of care.
Unplanned pregnancies constitute major public health problems .The United Nations International Children’s Emergency Fund (UNICEF) estimates that over 800,000 women worldwide die each year as a result of pregnancy and pregnancy-related causes and an additional 15 million women are severely disabled by pregnancy. Countries in which women utilize contraception have lower birth rates and the lowest rates of maternal mortality. Every method of birth control prescribed is safer than pregnancy.

Benefits/Importances of Family Planning
To the Mother
- Physical and Mental Recovery: Allows the mother to recover physically and mentally from the effects of previous pregnancies.
- Participation in Productive Activities: Offers ample time for a woman to actively participate in productive activities like farming and business.
- Enhanced Social Bondage: Increases social bondage between the mother and her baby.
- Reduced Maternal Mortality and Morbidity: Helps to reduce maternal mortality and morbidity due to pregnancy-related complications.
- Promotion of Marital Happiness: Promotes a happy marital life and enjoyment between the couples without fear of unwanted pregnancy.
- Preparation for Pregnancies: Family planning enables sexually active couples to prepare for pregnancies, optimizing fetal and maternal outcomes.
- Avoidance of Unwanted Pregnancies: Family planning helps avoid unwanted pregnancies, reducing complications associated with childbirth.
- Reduction of Maternal Complications: Reduces incidences of complications such as anaemia, poor maternal health, caesarean section, and maternal-child deaths.
To the Child
- Emotional and Social Support: The child receives adequate emotional and social support, contributing to emotional maturity and stability.
- Healthy Nutrition: Allows adequate nutrition for the baby in the womb, resulting in a healthy newborn.
- Reduced Malnutrition: Reduces malnutrition by preventing early weaning and ensuring enough food for the child.
- Fewer Infections: The child experiences fewer infections due to a strengthened immune system.
- Love and Care for the Child: Enables families to concentrate on other income-generating activities, ensuring love and care for the child.
- Ensuring Breastfeeding: Ensures adequate breastfeeding for the child, promoting child health.
To the Father
- Reduced Domestic Violence: Family planning reduces domestic violence in a home.
- Meeting Basic Needs: Enables the father to meet basic needs like food, medical care, etc.
- Cost of Living Reduction: Reduces the cost of living in a home, allowing the father to invest in productive activities.
- Preparation for Children: Assists couples in preparing for their children, ensuring they can provide love, care, and adequate support.
- Protection Against STIs: Some family planning methods are protective against HIV and other sexually transmitted infections (STIs).
To the Community
- Healthy and Productive Population: Family planning contributes to a healthy and productive population, enhancing community stability and harmony.
- Reduced Overcrowding: Reduces overcrowding, maximizing available land for productivity.
- Increased Socio-economic Development: Leads to increased socio-economic development within the community.
- Prevention of Negative Behaviours: Reduces the presence of negative characters in the community, as parents have adequate time to provide for their children.
- Improvement in Standards of Living: Family planning contributes to the improvement of standards of living within communities.
To the Nation
- Control of Population Growth: Reduces the rapid population growth rate at a national level.
- Reduced Dependence on Foreign Aids: Reduces the country’s dependence on foreign aids.
- Improved Government Services: Enables the government to provide better social services and infrastructures like roads and health facilities.
- Effective Resource Allocation: Facilitates easy budgeting for the people, as the number of resources to the population is manageable.
- Population Growth Prediction: Helps predict population growth, allowing for better planning and resource allocation.
Components of Family Planning Services
- Counselling: Counselling is an important need for the initiation and continuation of a family planning method. Service providers must undergo training to provide comprehensive counselling about all available family planning methods. Importantly, there should be no incentives or coercion to adopt family planning or a specific contraceptive method.
- Provision of Contraceptives: Contraceptives should be provided to clients based on approved method-specific guidelines. Service providers delivering these methods must undergo training to ensure competency in their provision. This ensures that clients receive family planning services that align with their needs and preferences.
- Follow-Up and Referral System: Clients choosing a family planning method should be informed about appropriate follow-up requirements. They should be encouraged to return to the service provider if they have any concerns or issues. The established referral system should be followed by service providers when making client referrals for further assistance.
- Record Keeping: Family planning service providers are required to maintain comprehensive records. These records help identify each client, specify the type of contraception provided, and note any special circumstances associated with its provision. Effective record-keeping contributes to the overall management and evaluation of family planning programs.
- Supervision: Supervision is an essential component of program evaluation. It ensures that client needs are met, and service delivery guidelines are adhered to. Supervisors act as team members who promote staff motivation, assist in problem-solving, and ensure the rights of both service providers and clients are observed throughout the delivery of family planning services.
- Logistics: Maintenance of an effective organization and supply system is crucial to prevent both understocking and overstocking of family planning commodities. Staff at service delivery points must adhere to proper procedures for the storage and handling of contraceptives and other supplies to maintain the quality of services provided. This ensures that family planning services are consistently available and accessible to those in need.
Characteristics of an Ideal Family Planning Method
- Effectiveness: A good family planning method should demonstrate high efficacy in preventing unintended pregnancies.
- Minimal Side Effects: The method should have minimal or no adverse effects on the health and well-being of the individual using it.
- Independence from Sexual Intercourse: The effectiveness of the method should not be relying on specific timing related to sexual activity.
- User Autonomy: The method should empower individuals to manage their reproductive health without requiring constant supervision or intervention from health professionals.
- Accessibility: It should be widely available, ensuring that individuals, regardless of geographic location or socioeconomic status, can access and utilize the method.
- Ease of Distribution: The method should have a distribution system that allows for easy accessibility, ensuring convenience for users.
- Affordability: Cost-effectiveness is crucial. A good family planning method should be affordable to a broad range of individuals, regardless of income.
- Cultural and Religious Acceptance: The method should be culturally and religiously sensitive, respecting diverse beliefs and practices.
- Reversibility: Individuals should have the option to discontinue the use of the method easily, with a quick return to fertility if desired.
- Educational Support: The method should come with educational resources to ensure users are well-informed about its proper use, benefits, and any potential risks.
- Long-Lasting: Ideally, the method should offer a duration of protection that aligns with the user’s family planning goals, whether short-term or long-term.
- Compatibility with Health: The method should not compromise overall health, and individuals with specific health conditions should have suitable alternatives available.
- Privacy and Confidentiality: The use of the method should be discreet, respecting the user’s privacy and maintaining confidentiality.
- Community and Partner Support: It should encourage open communication and support from partners, families, and communities.
- Research-Backed: The method’s safety and efficacy should be supported by scientific research and continuous monitoring.
- Inclusivity: The method should be inclusive, addressing the diverse needs of different populations, including adolescents, women, and men.
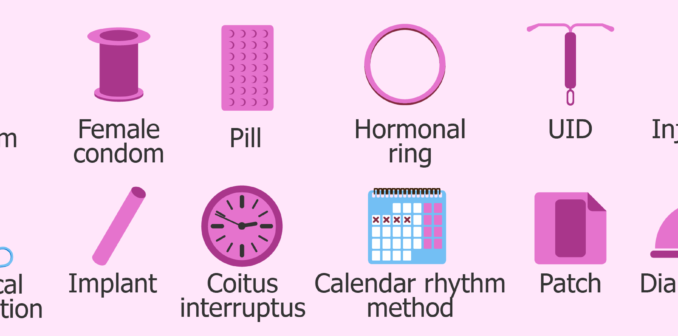
Classification of family planning methods
There are 2 broad types of family planning:
- Natural or Traditional or Non-hormonal methods.
- Artificial or Hormonal methods.
Natural/Traditional Methods
Method | Description |
Calendar/Rhythm | Tracking menstrual cycles for fertility awareness. This is the only method approved in the Roman Catholic Church |
Basal Body Temperature | Monitoring temperature variations during the menstrual cycle |
Cervical Mucus Method | Observing changes in cervical mucus for fertility awareness |
Lactation Amenorrhea Methods | Reliance on breastfeeding as a natural contraceptive during postpartum period |
Abstinence | Refraining from sexual activity |
Withdrawal/Coitus Interruptus | Withdrawing the penis before ejaculation |
Artificial Methods
a) Barrier Methods:
Method | Description |
Spermicides | Chemical substances that kill sperm |
Condoms | Barrier devices worn over the penis or inserted into the vagina to prevent sperm from reaching the egg |
Intrauterine Contraceptive Devices (IUCDs) | Devices placed inside the uterus to prevent pregnancy |
Diaphragm | Shallow, dome-shaped cup placed over the cervix with spermicide |
b) Hormonal Methods:
i. Oral Pills:
Method | Description |
Combined Oral Contraceptives | Pills containing both oestrogen and progestin hormones |
Progesterone-Only Pills | Pills containing only progestin hormone |
Emergency Contraceptive Pills | Pills taken after unprotected sex to prevent pregnancy |
ii. Implants:
Method | Description |
Implanon (1 Rod Capsule) | Subdermal contraceptive rod |
Jadelle (2 Rod Capsules) | Subdermal contraceptive rods |
Norplant (6 Rod Capsules) | Subdermal contraceptive rods |
iii. Injectable Contraceptives:
Method | Description |
Depo Provera | Injectable contraceptive administered every three months |
Injector Plan | Injectable contraceptive |
Sayana Press | Injectable contraceptive |
Noristrate | Injectable contraceptive |
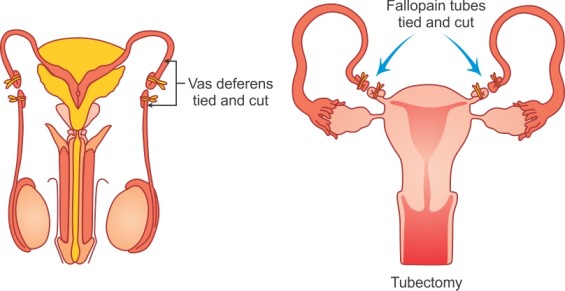
c) Permanent Methods:
Method | Description |
Tubal Ligation (Tubectomy) for Women | Surgical procedure to block or cut the fallopian tubes |
Vasectomy for Men | Surgical procedure to block the vas deferens in the male reproductive system |
NON-HORMONAL FAMILY PLANNING METHODS
They are so-called because they are not manufactured with hormone basis.
NATURAL NON-HORMONAL
These include:
Fertility awareness methods of family planning which involve identification of the fertile days of the menstrual cycle (when pregnancy is most likely to occur) and avoiding sexual intercourse (or using barrier methods ) during these days. The fertile days of the menstrual cycle can be determined by one of the following methods:
- Calendar/Rhythm or Standard Days method, including cycle beads.
- Basal Body Temperature
- Cervical Mucus Method
- Symptom- thermal ( a combination of cervical mucus and BBT methods).
Other Non Hormonal/traditional include;
- Lactation Amenorrhea Methods
- Periodic abstinence, abstaining from sexual intercourse during a woman’s fertile time.
- Withdrawal/Coitus Interruptus
These methods, also known as fertility awareness methods, are based on understanding key physiological conditions related to reproduction, Such as;
Lifespan of Sperm and Ovum:
- The lifespan of a sperm is approximately 3 – 5 days in the female reproductive tract.
- The lifespan of an ovum (egg) is around 12- 24 hours.
- Menstrual cycles can range between 23 to 35 days, but usually 28 days.
General Advantages:
- Safety and Lack of Side Effects: FAMs are generally considered safe with minimal or no side effects.
- Cost-Effectiveness: They are affordable, requiring no ongoing financial commitment.
- Acceptability Across Groups: Often acceptable to individuals and religious groups opposing modern contraceptive methods.
- Educational Benefits: These methods empower women with knowledge about their menstrual cycles and fertility.
- Couples’ Control: Couples have direct involvement and control over the method, promoting shared responsibility.
- Facilitates Pregnancy Planning: FAMs can be used for both family planning and to facilitate pregnancy when desired.
- Non-Invasive: FAMs do not involve invasive procedures or the use of synthetic substances.
- No Hormonal Interference: They do not interfere with hormonal balances, making them suitable for those sensitive to hormonal contraceptives.
- Long-Term Relevance: Useful throughout a woman’s reproductive life, fostering awareness and informed decision-making.
General Disadvantages:
- Learning Curve: Some methods require substantial education and learning before effective use.
- Record Keeping: Users must maintain accurate records over several menstrual cycles for proper reference.
- Challenges with Irregular Periods: Effectiveness diminishes when menstrual cycles are irregular.
- Behavioural Adjustments: Requires adjustments to sexual behaviors during fertile periods.
- Dependency on Partner Cooperation: Success depends on the level of cooperation between partners, which can be challenging.
- Risk of Error: Inconsistencies in recording or misinterpretation may lead to unintentional pregnancies.
- Limited Protection from STIs: FAMs provide no protection against sexually transmitted infections (STIs), including HIV/AIDS.
- Intensive Monitoring: The method demands continuous and intensive monitoring, which may be burdensome for some users.
Indications:
Fertility awareness methods are suitable for any woman or couple who is willing and committed to observing, recording, and interpreting fertility signs on a daily basis. This includes:
- Women who find other contraceptive methods unacceptable due to reasons such as religious beliefs.
- Women who cannot use certain contraceptive methods for health reasons.
- Couples who are open to abstaining from sexual intercourse (or using condoms) for more extended periods during each menstrual cycle.
Contraindications:
While there are no medical conditions that worsen with the use of fertility awareness methods, some conditions may make their application more challenging. In the presence of these conditions, the method may either be postponed or require specialized counselling to ensure correct utilization. These conditions include:
- Breastfeeding, especially until the return of menstruation.
- Less than three postpartum menstrual cycles.
- Irregular vaginal bleeding.
- Abnormal vaginal discharge.
- Diseases that influence body temperature.

Barrier methods
Barrier methods work by preventing the passage of sperm into the female genital tract.
Female barrier methods include the diaphragm, cervical cap, FemCap, and the condom to both females and males and Spermicides
Condoms
A condom is a latex sheath put on an erect penis before coitus and worn during coitus.
Indications for Condom Use:
- Men Engaging in Family Planning: Condoms are an excellent choice for men who wish to actively participate in family planning.
- Sexually Active Adolescents: Adolescents engaging in sexual activity can benefit from the use of condoms as a reliable contraceptive and STI prevention method.
- Infrequent Sexual Intercourse: Couples who engage in sexual intercourse infrequently may find condoms to be a practical and effective choice.
- Casual Sexual Relationships: Individuals in casual sexual relationships where pregnancy is not desired can use condoms to prevent both unwanted pregnancies and sexually transmitted infections (STIs).
- Back-Up Contraception: Couples waiting for another contraceptive method to become effective can use condoms as a reliable back-up method.
- Temporary Contraception: Couples awaiting the initiation of another contraceptive method can use condoms as a temporary solution to prevent unintended pregnancies.
Mechanism of action of condom
- Acts as a barrier, preventing sperm from entering the female genital tract.
- For condoms that are coated with spermicide, the spermicide immobilizes and kills sperm.
Advantages of male and female condom
- Effectiveness: When used correctly, condoms provide a high level of effectiveness (95 – 97%) in preventing pregnancy.
- STI and HIV Prevention: Condoms are crucial in preventing the spread of sexually transmitted infections (STIs), including HIV.
- Accessibility: Condoms are easy to obtain and can be distributed widely by Community Based Health Workers and the commercial sector.
- Dual Purpose: They serve a dual purpose of family planning and STI/HIV prevention.
- Potential Cervical Cancer Protection: There is a probable protective effect for women against the development of Intra-epithelial Neoplasm, i.e., cervical cancer.
- Ease of Use: Condoms are easy to use, usually inexpensive, safe, effective, and portable.
- Sexual Enhancement: They can help some men with premature ejaculation maintain an erection.
- Convenient Short-Term Contraception: Condoms are convenient when short-term contraception is required.
- Safety and Lack of Side Effects: Condoms are considered safe with minimal side effects.
Disadvantages:
- Allergic Reactions: Some individuals may experience allergic reactions to latex or other materials used in condoms.
- Sexual Enjoyment: Condoms may reduce the quality of sex for some individuals.
- Male Partner Cooperation: Requires cooperation from the male partner for effective use.
- Vulnerability to Damage: Can be damaged by exposure to oil-based lubricants, heat, humidity, or light.
- Decreased Sensitivity: May decrease sensitivity for men, impacting the enjoyment of intercourse.
- Slipping or Tearing: There is a small possibility of slipping or tearing during sexual intercourse.
- Storage Requirements: Condoms can deteriorate if not properly stored, e.g., in too much heat, sunlight, or humidity.
- Erection Challenges: Some men may struggle to maintain an erection with a condom on.
Spermicides
Vaginal spermicides come in the form of foam, cream, jelly, tablet or suppository and are inserted into the vagina just before sexual intercourse to prevent pregnancy.
Mechanism of action of spermicide
- Inactivates and kills sperm;
- Blocks the path of sperm to the uterus.
Effectiveness of spermicides
- Fairly effective, depending on the user (79-97%);
- If used with condom, effectiveness is 99%;
- Effectiveness lasts only 30 to 40 minutes after insertion.
Advantages of spermicides
- Over-the-Counter Availability: Spermicides can be obtained without a prescription, making them easily accessible.
- Immediate Protection: Spermicides can be kept available for immediate use whenever needed, providing on-the-spot protection.
- Additional Lubrication: Spermicides can offer additional lubrication during intercourse, enhancing comfort.
- Enhanced Effectiveness with Condoms: When used in conjunction with condoms, spermicides can increase their overall effectiveness in preventing pregnancy.
- Back-Up Option for Contraceptive Delays: Spermicides serve as a simple back-up option for women waiting to start oral contraceptives or have an IUD inserted. They are also useful for women who forget multiple contraceptive pills or run out of pills.
- Emergency Use: In cases of a condom breakage, spermicides can be applied quickly as an emergency measure.
Disadvantages and Side Effects:
- Sexual Interruption: Some forms of spermicides, such as suppositories or foaming tablets, may require a waiting period of 10 minutes for dissolving before becoming effective, potentially interrupting sexual intercourse.
- Application Before Each Act: Spermicides must be used before each act of sexual intercourse, requiring consistent and timely application.
- Post-Intercourse Wetness: Spermicides may cause increased vaginal wetness for several hours after intercourse.
- Sensitivity or Allergic Reactions: A few women may be sensitive or allergic to spermicides, leading to irritation and discomfort, especially with frequent use.
- Lower Effectiveness Rates: Spermicides are generally less effective in preventing pregnancy compared to more modern methods such as IUDs and hormonal contraceptives.
- Risk of Candida Vaginitis: Some women may develop Candida Vaginitis as a side effect of using spermicides.
- Increased Infections: Spermicides can potentially increase the risk of urinary and yeast tract infections in women.
- Messiness and Discomfort: Spermicides can be messy and may cause mild discomfort or minor allergic reactions in some individuals.
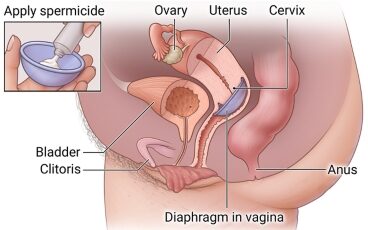
Vaginal Diaphragm
Diaphragm is a mechanical barrier placed between the vagina and cervical canal .They are designed to fit in the cul-de-sac and cover the cervix.
The contraceptive jelly or creams should be placed on the cervical side of the diaphragm before insertion because the device itself is ineffective. Again, this medication serves as lubricant for insertion of a device.
The device is inserted 6 hours prior to intercourse and should be left in place 6-24 hours after intercourse
Advantages
- Easy to use
- It offers some protection against STDs
- Well used, it protects from conception with the failure rate as low as 6% of women per year of exposure.
Disadvantages
- It require fitting by a well trained medical professional
- Fitting may loose during intercourse
- It cannot be effective in women with significant pelvic relaxation,a sharply retroverted or anteverted uterus or shortened vagina.
Side effects
- Vagina irritation
- Increased risk of urinary tract infection due to pressure of the rim against the urethra and alterations in the composition of vaginal normal flora.
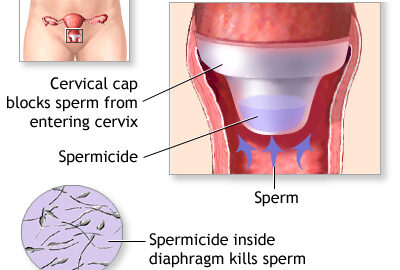
Cervical Cap (CAP)
Cervical caps are small cuplike diaphragms placed over the cervix that are held in place by suction.
To provide a successful barrier against the sperms, they must be tightly fit over the cervix therefore, individualization is essential because of variability in cervical size.
It has few advantages because;
- Unpleasant odour often develops after approximately 1 day of use
- Dislodgment (as in diaphragm)
- The cup should remain in place 1 or 2 days before intercourse and should be left in place for 8 -48 hours after intercourse.

Intrauterine Contraceptive Devices (IUCDs):
Intrauterine Contraceptive Devices, or IUCDs, are flexible plastic devices inserted into a woman’s uterus to prevent pregnancy, usually renewed every 3-5 years. These devices are often made of copper impregnated with gold, silver, and stainless steel.
Various Design Types:

- T-shaped device with copper on the stem and arms of the T.
- Duration of effectiveness: 10 years.
- Shelf life: 7 years.
Multiload 375:
- Lasts for 5 years.
Mechanism of Action:
- Renders the endometrium unsuitable for the implantation of a fertilized ovum.
- Copper emits metal ions with spermicidal properties.
Advantages:
- Very Effective: Provides high efficacy, ranging from 99-99.5%.
- Immediate Effectiveness: Works instantly upon insertion.
- Long-Term Method: Offers a long duration of effectiveness.
- No Interference with Intercourse: Does not interfere with sexual activity.
- Quick Return to Fertility: Fertility returns immediately upon removal.
- Few Side Effects: Mild side effects compared to other methods.
- No Client Supplies Needed: Does not require additional supplies by the client.
Disadvantages and Side Effects:
- Mild Cramps: May experience mild cramps in the first 3-5 days post-insertion.
- Menstrual Changes: Longer and heavier menstrual blood loss in the initial 3 months.
- Increased Cramping Pain: Increased cramping pain during menstruation.
- Provider-Dependent: Insertion and removal depend on a healthcare provider.
- String Checks: Need to check for strings after menstruation.
- Increased Bleeding: May experience increased bleeding in the first few months.
- Spontaneous Expulsion: There is a possibility of spontaneous expulsion, especially in the first 6 months.
- Uterine Perforation: Very rare, occurring in 1 out of 1000 cases.
- Pelvic Inflammatory Diseases (PID): May increase the risk of PID.
- Pain and Discomfort: Pain, especially with larger devices.
- Menstrual Changes: Increased menstrual loss; intermenstrual spotting may occur.
- Expulsion Risk: Higher risk of expulsion during the first 6 months, especially during menses.
- Translocation Risk: Possibility of translocation to the peritoneal cavity or broad ligament.
- Pregnancy Risks: May increase the risk of pregnancy and ectopic pregnancy.
- No Protection Against STIs/HIV or Cancers: Does not provide protection against STIs, HIV, ovarian, endometrial, or cervical cancers.
IUCDs users who develop PID should be treated with the IUCD in place if they want to continue using it. If no improvement within 72 hours, remove it.
When to Insert an IUCD:
- During or immediately after menstruation.
- At a postnatal examination.
- Immediately following delivery or any time within 46 hours after childbirth.
- After termination of a pregnancy.
- During the caesarean section.

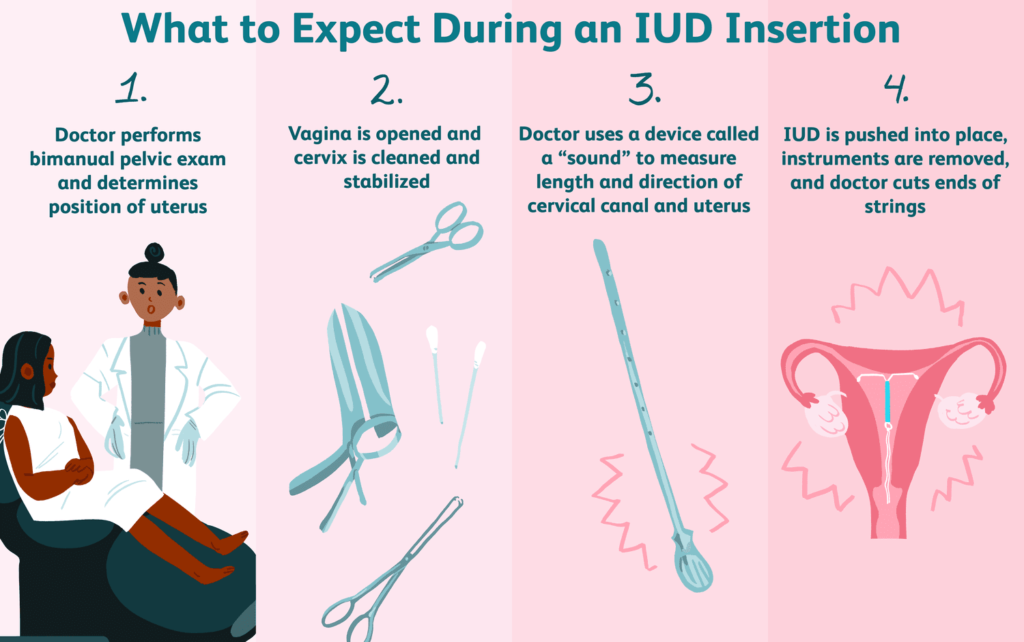
Insertion of an Intrauterine Contraceptive Device (IUD): Procedure
- Aseptic Technique: Implement aseptic techniques, including hand washing and wearing sterile gloves.
- Device Preparation: Place the IUD in an introducer and plunger.
- Straightening: The device straightens inside the introducer.
- Visualization of Cervix: Insert a Cusco’s vaginal speculum to clearly visualize the cervix.
- Cleaning: Clean the cervix and vaginal vault with sterile swabs.
- Uterine Measurement: Measure the length of the uterus with a uterine sounder.
- Introducer Insertion: Insert the introducer into the uterus through the cervix.
- Plunger Action: Gently push the plunger to force the device out of the introducer into the uterus.
- Device Lodging: In the uterus, the device resumes its original shape and lodges against the uterine walls.
- String Placement: The two small strings attached to the device hang down through the cervical opening.
- String Cutting: Cut the string with scissors to reduce the size, leaving approximately 3cm hanging out of the cervix.
- Post-Insertion: After insertion, the client rests and can remain on the procedure table until ready to get dressed.
- String Check: The woman can feel the strings in the vagina to ensure the device is in position.
Post-Insertion Instructions:
- Backup Use: Use backup contraception for a minimum of 3 days.
- Mild Pain: Slight pain may occur but usually does not require medication.
- String Check: Check the string during menstruation to ensure it is in place; return if removed or dislodged.
- Immediate Return for Discomfort: Return to the facility immediately in case of any discomfort.
Removing the IUDs:
- Discussion with Client: Discuss side effects with the client and weigh the option of managing the problem or immediate removal.
- Timing for Removal: Removal is simple and can be done any time of the month, with monthly bleeding making it easier.
Removal Procedure:
- Explain the removal procedure to the client.
- Ensure privacy and confidentiality.
- Visualize cervix and UID strings with a vaginal speculum.
- Clean cervix and vagina with antiseptic solution.
- Instruct the client to relax and take slow breaths.
- Gently pull the IUD strings until it comes completely out of the cervix.
- Show the removed IUD to the client for assurance.
- Thank the client for cooperating throughout the procedure.
Reasons for Missed Threads in IUDs:
- Coiled thread inside.
- Thread torn through.
- Device expelled outside unnoticed by the client.
- Device perforated the uterine wall and is lying in the peritoneal cavity.
- Device pulled by the growing uterus in pregnancy.
Methods of Identification:
- History taking (exclude pregnancy).
- Ultrasonography.
- Hysterectomy.
- Hysteroscopy.
- Straight x-ray.
Contraindications:
- Pregnant women or those suspected to be.
- Women with menorrhagia or abnormal bleeding.
- Women with PID, current, or in the past 3 months.
- Purulent per vaginal discharge, gonococcal, or chlamydial infection.
- Malignant trophoblastic disease.
- Pelvic tuberculosis.
- Women with genital tract cancer.
Surgical methods
Male Vasectomy
Male vasectomy is a permanent operation in the male where a segment of vas deferens of both sides are resected and the cut ends are ligated.
Vasectomy is a voluntary surgical procedure for permanently terminating fertility in men.
Mode of Action
Blocking the vas deferens (ejaculatory duct) to prevent sperm presence in the ejaculate.
Indications
Men certain about achieving their desired family size, seeking a highly effective permanent contraceptive method, or whose partners face unacceptable pregnancy risks.
Contraindications
Vasectomy should be delayed in the case of local or systemic infections.
Benefits
- Highly effective
- Permanent
- Simple surgery under local anesthesia
- No further expense or concerns about conception
- No long-term side effects
- Does not interfere with sexual intercourse
Side Effects
- Wound infection
- Scrotal hematoma
- Granuloma
- Excessive swelling
- Pain at incision sites
Explain to Clients
- When to come back for follow-up visits
- Common side effects of the method
- What to do if there are changes in menstrual periods
- How soon the method is effective
- How to protect against STIs
- How to care for the wound postoperatively
General Instructions to Clients Using Permanent Methods
- Inform about follow-up visit schedules
- Explain common side effects in simple language
- Share warning signs or possible problems requiring medical attention
- Guide regarding changes in menstrual periods
- Emphasize the method’s lack of protection against HIV/AIDS and STIs, advocating for backup methods like condoms
- Provide instructions on wound care postoperatively
Female -Tubal ligation
Female Tubal Ligation is the interruption of continuity of fallopian tubes.
Tubal ligation is a voluntary surgical procedure for permanently terminating fertility in women. It can be done by a mini-operation (laparatomy/laparoscopy).
Mode of Action
Blocking fallopian tubes by cutting, cautery, rings, or clips, preventing sperms from reaching the ovum.
Indications
Women certain about achieving desired family size, seeking a highly effective permanent contraceptive method, or facing unacceptable pregnancy risks. Family planning should be delayed in specific cases, such as pregnancy, postpartum complications, or certain health conditions.
Timing of the Tubal Ligation
- Immediately after childbirth or within the first seven days (if chosen in advance)
- Six weeks or more after childbirth
- Immediately after abortion (if chosen in advance)
- Any time, provided pregnancy is ruled out (between seven days and six weeks postpartum)
- During cesarean section
Benefits
- Highly effective
- Immediate effectiveness
- Permanent
- Simple surgery under local anesthesia
- No contraception-related concerns
- No long-term side effects
- Does not interfere with sexual intercourse
Disadvantage
- Does not protect against STIs/AIDS
- Irreversible
Side Effects
- Wound infection
- Post-operative fever
- Rare bladder and intestinal injuries
- Hematoma
- Pain at the incision site
- Superficial bleeding
Challenges associated with Tubal Ligation
- Desire for more children after the operation
- Excessive desire for reversal
- Disagreement to sign the informed consent form
- External pressures
- Depression
- Marital problems
General Complications
- Obesity
- Psychological upset
- Chronic pelvic pain
- Congestive dysmenorrhea
- Menstrual abnormalities
General Advantages
- Simple Surgical Procedure: The procedure is straightforward and uncomplicated.
- Out-Patient Procedure: It can be performed as an outpatient procedure, avoiding the need for a hospital stay.
- Few Complications: The surgery has a low incidence of complications.
- Reversal Anastomosis: Reversal procedures, known as anastomosis, have a 50% chance of success.
- Highly Effective: The failure rate is minimal, at 0.15%.
- No Interference with Sexual Life: Vasectomy does not interfere with the sexual life of the individual.
- Performed Under Anesthesia: The operation is conducted under anaesthesia, ensuring a painless experience.
General Disadvantages
- Lack of Protection Against HIV and STDs: Vasectomy does not provide protection against HIV and sexually transmitted diseases (STDs).
- Costly Reversal: Reversal procedures can be expensive.
- Consent Requirements: Obtaining consent may involve important family members in decision-making.
- Risk of Injury to Internal Organs: There is a potential risk of injury to internal organs during the procedure.
- Anaesthesia Risks: The use of anaesthesia carries inherent risks.
- Post-Surgical Complications: Possible complications include infection and bleeding.
- Additional Contraception Required: Additional contraception is needed for about 2-3 months until semen becomes free of sperm.
- Potential for Impotency: There is a rare risk of impotence.
- Frigidity: Frigidity, especially sexual unresponsiveness in women and an inability to achieve orgasm during intercourse, may occur.
- Stigma: Societal stigma may be associated with the decision to undergo vasectomy.
Important points to think about before the use of a permanent contraception
Because male and female sterilization are permanent methods of contraception, thorough counselling procedures must be followed to ensure that the client fully understands his or her choice and to minimize chances of regret.
- Counselling: Thorough counselling sessions to ensure informed decision-making.
- Reasons for Choosing Permanent Methods: Understand and evaluate the motivating factors behind the choice of permanent contraception.
- Screening for Risk Indicators for Regret: Identify potential risk indicators such as:
- Young age
- Low parity
- Single-parent status
- Marital instability
- Completion of Informed Consent Process: Ensure the individual fully comprehends the implications and consequences of the procedure.
- Details of the Procedure: Provide comprehensive information about the surgical process involved in permanent contraception.
- Possibility of Failure: Acknowledge the rare but existing possibility of the procedure not being 100% effective.
- Positive Pregnancy Test Result: In case of a positive pregnancy test post-tubal ligation, rule out ectopic pregnancy.
- Condom Use for STD Protection: Emphasize the continued need for condom use to safeguard against sexually transmitted diseases.

I appreciate the notes are well detailed, well explained and so on, I just wish it could be possible for me to download to my phone storage
Very nice notes can I download
How can I download this notes to my phone storage
Thank u sir for always adding a block to our success