Sub-topic 3.4.1: Review of Anatomy and Physiology of the Circulatory system
Anatomy of the Heart and Circulatory System
- Arteries: Carry oxygenated blood away from the heart to the rest of the body. The largest artery is the aorta.
- Veins: Carry deoxygenated blood back to the heart. The largest veins are the vena cavae.
- Capillaries: Tiny blood vessels that connect arteries and veins, where the exchange of oxygen, nutrients, and waste products occurs between blood and tissues.
Physiology of the Circulatory System
- Cardiac Cycle: The sequence of events that occurs when the heart beats, including systole (contraction) and diastole (relaxation).
- Blood Pressure: The force of blood against the walls of the arteries. Measured as systolic pressure (during heart contraction) over diastolic pressure (during heart relaxation).
- Heart Rate: The number of times the heart beats per minute.
- Cardiac Output: The volume of blood pumped by the heart per minute (Heart Rate x Stroke Volume).
- Regulation of Blood Flow: Regulated by various mechanisms, including nervous system control, hormonal control, and local factors.
- Gas Exchange: Occurs in the lungs (oxygen into blood, carbon dioxide out) and in the tissues (oxygen out of blood, carbon dioxide into blood).
- Nutrient and Waste Transport: Blood delivers nutrients and hormones to cells and removes waste products.
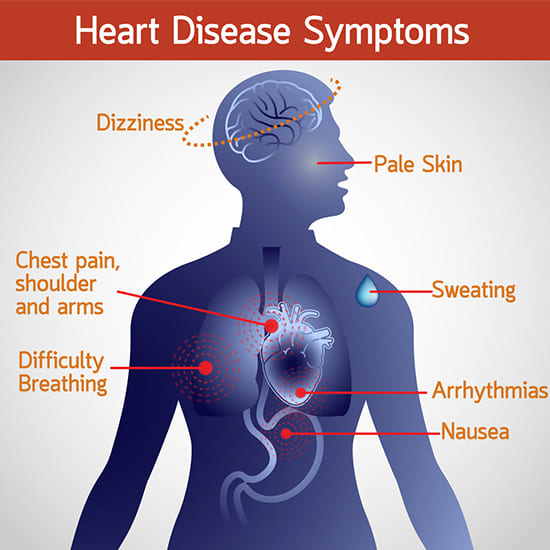
Sub-topic 3.4.2: General Signs and Symptoms of Cardiovascular Disorders
Signs and symptoms of heart disease
- Chest pain (Angina Pectoris): Often described as a heavy, squeezing, or burning sensation, typically in the center or left side of the chest. It may radiate to the left arm, neck, jaw, back, or stomach. Often provoked by exertion or stress and relieved by rest or nitroglycerin. Different types include stable angina, unstable angina, and Prinzmetal's angina.
- Dyspnoea (Shortness of Breath): Difficulty breathing, which can be exertional (occurs with activity), orthopnea (occurs when lying flat), or paroxysmal nocturnal dyspnoea (occurs at night, waking the person from sleep). It results from pulmonary congestion due to inefficient heart pumping.
- Palpitations: A sensation of a rapid, strong, irregular, or fluttering heartbeat. Can be caused by various arrhythmias (abnormal heart rhythms).
- Syncope (Fainting): Temporary loss of consciousness due to a sudden decrease in blood flow to the brain, often caused by arrhythmias, severe valve disease, or significant drop in blood pressure.
- Fatigue: Persistent and unexplained tiredness, often due to the heart's inability to pump enough oxygenated blood to meet the body's demands (inadequate systemic perfusion).
- Peripheral Oedema: Swelling, typically in the ankles, feet, and legs, due to fluid retention. This occurs when the heart's pumping action is inefficient, leading to increased pressure in the veins and fluid leakage into surrounding tissues, exacerbated by renal underperfusion and activation of the Renin-Angiotensin-Aldosterone System (RAAS).
- Cyanosis: Bluish discoloration of the skin and mucous membranes due to inadequate oxygenation of the blood. Can be central (lips, tongue) or peripheral (fingertips, toes).
- Clubbing of the Fingers: Enlargement of the fingertips and curving of the nails, often associated with chronic oxygen deprivation.
- Irregular or Thread Pulse: An abnormal heart rhythm or a weak and rapid pulse, indicating issues with heart function or blood volume.
- Raised Jugular Venous Pressure (JVP) and Extended Jugular Veins: Visible distension of the jugular veins in the neck, indicating increased pressure in the right side of the heart.
- Restlessness and Irritability: Non-specific symptoms that can be associated with reduced cerebral perfusion or overall systemic illness related to heart conditions.
- Heart Murmurs: Abnormal sounds heard during auscultation of the heart, caused by turbulent blood flow through damaged or narrowed heart valves, or other structural abnormalities.
Investigations done in heart disease
- Complete Blood Count (CBC): To assess for anemia (which can exacerbate heart conditions) and signs of infection.
- Haemoglobin level estimation: Specific measurement of oxygen-carrying capacity.
- Cardiac Enzymes/Biomarkers: Such as troponin (I and T), creatine kinase-MB (CK-MB), and B-type natriuretic peptide (BNP). These are released into the bloodstream when the heart muscle is damaged.
- Blood Urea Nitrogen (BUN) and Creatinine: To assess kidney function, which can be affected by heart disease and impact treatment.
- Serum Electrolytes: (Sodium, Potassium, Chloride, Magnesium, Calcium) to check for imbalances that can affect heart rhythm and function.
- Liver Function Tests (LFTs): To assess liver health, as liver congestion can occur in severe heart failure.
- Thyroid Function Tests: To rule out thyroid disorders, which can mimic or exacerbate heart conditions.
- Lipid Profile: (Total cholesterol, LDL, HDL, triglycerides) to assess risk factors for atherosclerosis and coronary artery disease.
- Blood for Culture and Sensitivity: If an infection (e.g., endocarditis) is suspected.
- C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Markers of inflammation, which can be elevated in various cardiac conditions.
- Exercise Stress Test: Monitors heart function during physical exertion (treadmill or stationary bike) to detect coronary artery disease.
- Pharmacological Stress Test: Uses medication to simulate the effects of exercise on the heart for patients unable to exercise.
- Stress Echocardiography or Nuclear Stress Test: Combines stress testing with imaging to assess blood flow to the heart muscle.
Revision Questions:
- What is the difference between a diagnosis and a differential diagnosis?
- List five general causes of disease and provide one specific example for each.
- Describe the three levels of disease prevention and give a nursing activity that falls under each level.
- What is Cor-pulmonale?
- A patient presents with breathlessness that worsens when they lie flat. What is the medical term for this symptom?

