Table of Contents
ToggleHEPATITIS
Hepatitis is an inflammation of the liver. While it can be caused by exposure to certain chemicals, drugs, or autoimmune processes, it is most commonly caused by a viral infection.
Types of Hepatitis
- Viral Hepatitis: Caused by a group of specific viruses (Hepatitis A, B, C, D, E, G). This is the most common form.
- Non-viral Hepatitis: Inflammation resulting from exposure to toxins (e.g., alcohol, industrial chemicals) or as a side effect of certain drugs (drug-induced hepatitis).
Viral Hepatitis
Viral hepatitis is a systemic viral infection in which necrosis and inflammation of liver cells produce a characteristic cluster of clinical, biochemical, and cellular changes. It is marked by liver-cell destruction, necrosis, and autolysis.
- Course: Viral hepatitis can be acute (short-term) or chronic (long-term, lasting more than 6 months). Hepatitis B, C, and D viruses can cause chronic hepatitis.
- Prognosis: The prognosis is generally good for acute hepatitis, but it becomes poor if complications like hepatic encephalopathy develop.
- Types: The main types are caused by viruses A, B, C, D, and E. Hepatitis F and G are rare.
Clinical Features of Viral Hepatitis (Phases)
The clinical manifestations of viral hepatitis can be classified into three phases.
1. Pre-icteric or Prodromal Phase
This is the initial phase before the onset of jaundice. Symptoms are often non-specific and flu-like.
- Anorexia (loss of appetite): Often the first and most significant symptom.
- Nausea and vomiting.
- Malaise, fatigue, and weakness.
- Headache and low-grade fever.
- Right upper quadrant discomfort or pain.
- Constipation or diarrhea.
- Decreased sense of taste and smell.
- Urticaria (hives).
- Hepatomegaly (enlarged liver) and splenomegaly (enlarged spleen) may be present.
2. Icteric Phase
This phase is characterized by the appearance of jaundice, although not all patients with hepatitis become jaundiced.
- Jaundice: Yellowing of the skin and sclera.
- Pruritus (itching): Due to bile salt deposition.
- Dark Urine (Bilirubinuria): Urine may appear deep orange or brown.
- Pale or White Stool (Acholic stool): Due to lack of bilirubin in the stool.
- Continued fatigue.
- Persistent hepatomegaly, often with tenderness.
- Weight loss.
3. Post-icteric or Convalescent Phase
This is the recovery phase, which begins as jaundice fades and can last for several weeks or months.
- Malaise and easy fatigability tend to persist.
- Hepatomegaly may continue but usually subsides.
- Appetite returns, and symptoms gradually improve.
Investigations for Viral Hepatitis
- Liver Function Tests (LFTs): To detect liver abnormalities. Typically shows markedly elevated levels of Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST).
- Viral Antigen and Antibody Tests (Serology): Blood tests are crucial to identify the specific type of hepatitis virus (e.g., Anti-HAV for Hepatitis A, HBsAg for Hepatitis B, Anti-HCV for Hepatitis C). Stool analysis can be done for Hepatitis A antigens.
- Abdominal Ultrasound Scan: To assess the size and texture of the liver and spleen and to rule out other causes of liver disease or obstruction.
- Blood for HIV Serology: To rule out co-infection, as HIV shares transmission routes with Hepatitis B and C.
Hepatitis A (HAV)
Hepatitis A, formerly known as infectious hepatitis, is caused by an RNA virus of the genus Enterovirus. It typically causes an acute, self-limiting illness and does not lead to chronic infection.
Transmission and Incubation
- Mode of Transmission: Primarily the fecal-oral route. This occurs through ingestion of food or liquids contaminated with the virus, poor sanitation, and close person-to-person contact.
- High-Risk Settings: Outbreaks are common in areas of overcrowding, poor sanitation, day-care centers, and other institutional settings.
- Infectious Period: The virus is found in the stool of infected patients before symptoms begin and during the first few days of illness.
- Incubation Period: Ranges from 2 to 6 weeks (15-50 days), with an average of about 4 weeks (30 days). The illness typically lasts for 4 to 8 weeks.
Prevention
- Hygiene: Regular and proper hand washing with clean water and soap is the single most effective preventive measure.
- Sanitation: Ensuring a safe water supply (boiling drinking water) and proper sewage disposal.
- Immunization (Pre-exposure Prophylaxis): Vaccination with the hepatitis A vaccine provides long-term protection. It is recommended for travelers to endemic areas.
- Post-exposure Prophylaxis: Administration of immune globulin (if not previously vaccinated) can prevent infection if given within 2 weeks of exposure to household members or sexual contacts.
- Health Education: Educating the public about safe food handling, personal hygiene, and transmission routes.
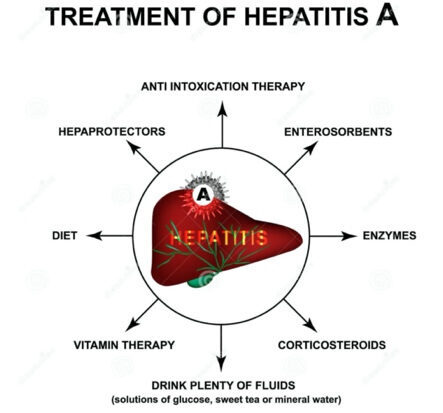
Management of HAV
Management is primarily supportive, as the infection is usually self-limiting.
- Encourage bed rest during the acute stage to reduce metabolic demands on the liver.
- Promote a nutritious, well-balanced diet. Small, frequent feedings may be better tolerated, supplemented by IV glucose if anorexia is severe.
- Promote gradual but progressive ambulation to hasten recovery. Patients are usually managed at home unless symptoms are severe.
- Instruct the patient and family on diet, rest, hygiene measures (especially hand washing) to prevent spread, and avoidance of alcohol, which is hepatotoxic.
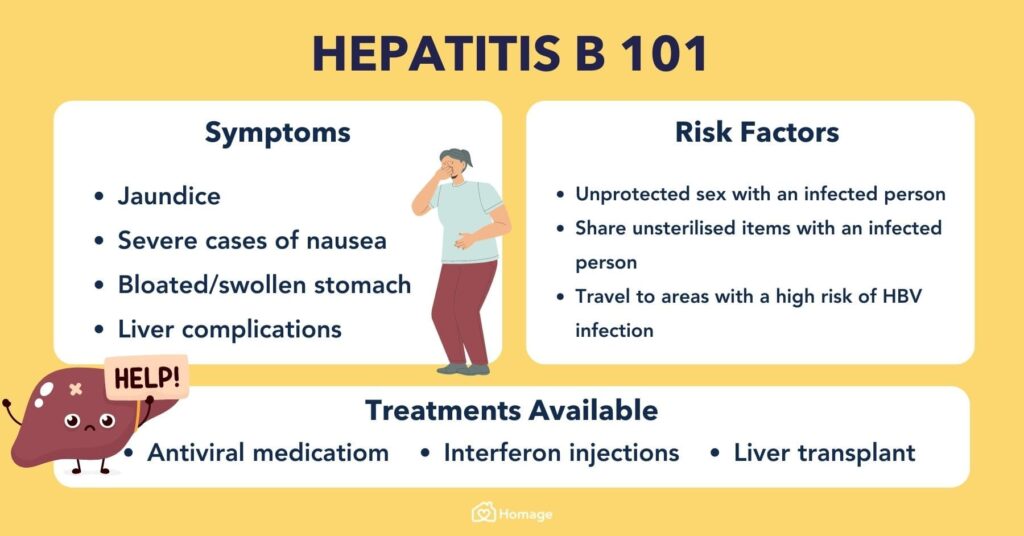
Hepatitis B (HBV)
Hepatitis B is caused by a DNA virus (HBV). It can cause both acute and chronic liver disease. About 10% of infected adults progress to a chronic carrier state, which poses a major worldwide risk for developing cirrhosis and hepatocellular carcinoma.
Transmission and Incubation
- Mode of Transmission: Transmitted primarily through blood and body fluids. The virus is found in blood, saliva, semen, and vaginal secretions and can be transmitted through breaks in the skin or mucous membranes.
- Incubation Period: HBV has a long incubation period, ranging from 1 to 6 months.
- Pathophysiology: The virus replicates in the liver and can remain in the serum for long periods, allowing for transmission.
Risk Factors for Hepatitis B
- Frequent exposure to blood, blood products, or other body fluids.
- Health care workers: Especially those in hemodialysis, oncology, and surgery, or those at risk for needlestick injuries.
- Patients undergoing hemodialysis.
- IV drug users (sharing needles).
- Individuals with multiple sexual partners or engaging in unprotected sex.
- Close contact with a person who is a chronic carrier of HBV.
- Receipt of blood products or organ transplants before routine screening was implemented.
Clinical Manifestations
Symptoms are often insidious and variable. In addition to the general features of hepatitis, some patients may have arthralgias (joint pain) and rashes.
Prevention
- Immunization: The hepatitis B vaccine is the mainstay of prevention. It is recommended for all children, health workers, and other high-risk populations.
- Screening: Continued screening of blood donors for hepatitis B surface antigen (HBsAg) to reduce transmission risk.
- Infection Control:
- Use of disposable syringes, needles, and lancets.
- Good personal hygiene and daily disinfection of work areas.
- Use of gloves (Standard Precautions) when handling any blood or body fluids.
- Safe Practices: Safe sexual practices (e.g., condom use) and safe transfusion practices.
Medical Management
- Antiviral Therapy: For chronic HBV, medications like Alpha-interferon, Lamivudine, or Adefovir may be prescribed to suppress viral replication.
- Supportive Care:
- Bed rest and restriction of activities until liver enlargement and LFTs begin to resolve.
- Maintain adequate nutrition. A diet low in protein may be necessary if the liver's ability to metabolize protein byproducts is impaired.
- Administer antiemetics for nausea and vomiting.
- Hospitalization and IV fluid therapy may be required for persistent vomiting and dehydration.
Hepatitis C (HCV)
Hepatitis C is caused by the hepatitis C virus. A significant portion of cases become chronic, making HCV a leading cause of cirrhosis, liver cancer, and liver transplantation.
- Transmission: Primarily transmitted by parenteral (blood-borne) means. This includes sharing contaminated needles (IV drug use), needlestick injuries in healthcare workers, and receipt of infected blood transfusions or organ transplants (though this is rare now due to screening). Sexual transmission is less common but possible.
- Incubation Period: Ranges from 15 to 160 days, with an average of 50 days.
- Clinical Course: The course is similar to hepatitis B, but symptoms are often milder or asymptomatic. However, a chronic carrier state occurs frequently, which significantly increases the risk for cirrhosis and liver cancer.
- Medical Management: Combination therapy with antiviral drugs like ribavirin and interferon has been used. Newer direct-acting antiviral (DAA) agents are now the standard of care, offering very high cure rates.
Risk Factors for Hepatitis C
- Recipient of blood products or organ transplants before 1992.
- Health care and public safety workers after needlestick injuries or mucosal exposure to blood.
- Children born to women infected with HCV.
- Past or current illicit IV or injection drug use.
- Past treatment with chronic hemodialysis.
- Having unprotected sex with an infected partner or multiple partners.
Hepatitis D (HDV - Delta Agent)
Hepatitis D is a unique virus that requires the hepatitis B surface antigen (HBsAg) for its replication. Therefore, HDV infection can only occur in patients who are also infected with hepatitis B.
- Risk: Only patients with hepatitis B are at risk for hepatitis D. It can occur as a co-infection (infected with HBV and HDV at the same time) or a superinfection (a chronic HBV carrier later gets infected with HDV).
- Transmission: Primarily through blood and sexual contact, similar to HBV. It is common in IV drug users and hemodialysis patients.
- Incubation Period: Varies from 21 to 140 days, with an average of 35 days.
- Clinical Course: Symptoms are similar to hepatitis B, but patients with HDV superinfection are more likely to have a severe, fulminant hepatitis and progress to chronic active hepatitis and cirrhosis.
- Treatment: Treatment is similar to other forms of hepatitis; there is no specific therapy for HDV. Prevention of HBV with vaccination also prevents HDV infection.
Hepatitis E (HEV)
Hepatitis E is caused by the hepatitis E virus and is clinically similar to hepatitis A.
- Transmission: Transmitted by the fecal-oral route, principally through contaminated water and poor sanitation.
- Incubation Period: Estimated to range from 15 to 65 days, with an average of 42 days.
- Clinical Course: Generally resembles hepatitis A, with a self-limited course and an abrupt onset. Jaundice is almost always present. HEV does not develop into a chronic form. However, it can be particularly severe in pregnant women, with a high mortality rate.
- Prevention: The major method of prevention is avoiding exposure through good hand hygiene and ensuring safe drinking water. The effectiveness of immune globulin is uncertain.
Hepatitis G (HGV)
Hepatitis G is a less common and less understood form of hepatitis.
- Transmission: It is primarily a post-transfusion hepatitis, transmitted through contaminated blood.
- Incubation Period: 14 to 145 days.
- Clinical Significance: Its role in causing significant liver disease is still being debated. The risk factors for infection are similar to those for hepatitis C.
NON-VIRAL HEPATITIS
Non-viral hepatitis is an inflammation of the liver that results from exposure to certain chemicals or drugs, rather than a viral infection. These substances can have toxic effects on the liver, leading to acute liver cell necrosis (toxic hepatitis).
Types of Non-Viral Hepatitis
- Toxic Hepatitis: Caused by exposure to hepatotoxic chemicals.
- Drug-Induced Hepatitis: Caused by a reaction to certain medications.
Causes
- Hepatotoxic Chemicals: Exposure can be through ingestion, inhalation, or injection. Examples include carbon tetrachloride, trichloroethylene, phosphorus, chloroform, and gold compounds.
- Drugs: Many drugs can be hepatotoxic, especially with overdose or in susceptible individuals. Common examples include acetaminophen (paracetamol), isoniazid, halothane, certain antibiotics, and anesthetic agents.
Clinical Features
The clinical presentation is similar to acute viral hepatitis.
- Anorexia, nausea, and vomiting.
- Jaundice with dark urine and clay-colored stools.
- Hepatomegaly and abdominal pain.
- Pruritus (itching) may be present in cholestatic forms.
Most patients recover fully from non-viral hepatitis once the offending agent is removed, although some may develop fulminant hepatitis or progress to cirrhosis.
Prevention
- Strict avoidance of alcohol during the acute illness and for at least 6 months after recovery.
- Avoidance of other potentially hepatotoxic substances, including certain medications, herbal remedies, illicit drugs, and toxins.
- Early detection and treatment of the acute illness.
Complications of Hepatitis
While many cases of acute viral hepatitis resolve without issue, serious and life-threatening complications can occur, particularly with chronic infections (HBV, HCV).
- Chronic Hepatitis: Persistent liver inflammation lasting more than 6 months, which can lead to more severe complications.
- Fulminant Hepatic Failure: A rare but severe complication of acute hepatitis, characterized by the sudden and massive destruction of liver cells, leading to liver failure.
- Liver Cirrhosis: Irreversible scarring of the liver tissue, which disrupts liver structure and function. This is a major long-term complication of chronic hepatitis B and C.
- Hepatocellular Carcinoma (Hepatic Cancer): Chronic HBV and HCV infections are primary risk factors for the development of liver cancer.
- Aplastic Anemia: A rare complication where the bone marrow fails to produce enough blood cells.
- Renal Failure: Can occur as part of a systemic response to severe liver disease (hepatorenal syndrome).
Management of a Patient with Hepatitis
Aims of Management
- To relieve signs and symptoms.
- To minimize liver inflammation and prevent further liver damage.
- To prevent complications.
- To prevent transmission to others.
Nursing Care Plan
Admission
The patient is admitted to a medical ward, ideally in an isolated or well-ventilated room if the type of hepatitis requires it (e.g., contact precautions for HAV). Place the patient on complete bed rest initially to decrease the metabolic demands on the liver. Record all patient particulars in the admission book.
Psychological Care
Establish a therapeutic rapport with the patient and their relatives. Provide counseling and clear information about the condition, its transmission, and the treatment plan to allay anxiety and promote cooperation.
Position
Nurse the patient in a position of comfort that ensures a patent airway and promotes easy breathing and circulation, such as semi-Fowler's position.
Observations
- Vital Observations: Monitor temperature, pulse, respiration, blood pressure, and oxygen saturation regularly (e.g., every 2-4 hours or as ordered). Maintain an observation chart and report any abnormalities promptly.
- Specific/Physical Observations: Closely observe and monitor for:
- Fever, jaundice, general aching, anorexia.
- Changes in urine (dark) and stool (pale).
- Dyspepsia, hepatomegaly, headache, pruritus.
- Nausea and vomiting.
- Signs of complications like changes in mental status (hepatic encephalopathy).
- Note the intensity and severity of all symptoms and report to the doctor.
Investigations
Prepare the patient for and assist with investigations as ordered:
- CBC: To rule out secondary bacterial infection and assess hemoglobin levels.
- Blood Smear for Malaria Parasites (MPs): To rule out malaria, a common cause of fever and jaundice.
- HIV Serology: To check for co-infection.
- Abdominal Ultrasound: To assess the size of the liver and spleen and rule out intra-abdominal complications.
- Liver Function Tests (LFTs): To monitor liver abnormalities.
- Viral Serology: Blood tests for viral antigens and antibodies to confirm the type of hepatitis.
Medications
Administer medications as prescribed and maintain an accurate treatment chart. This may include:
- IV antibiotics (e.g., Ceftriaxone) if a secondary bacterial infection is suspected.
- IV fluids (e.g., Normal Saline / 5% Dextrose) to maintain hydration, especially if the patient has anorexia, nausea, or vomiting.
- Analgesics/Antipyretics (e.g., Paracetamol) for pain and fever. Use with caution due to liver metabolism.
- Antivirals (e.g., Lamivudine, Tenofovir) for chronic Hepatitis B.
- Vitamin supplements as needed.
Diet
Provide a well-balanced diet that is high in carbohydrates and calories to spare protein and restore glycogen stores. Protein intake should be adequate unless signs of encephalopathy are present. Encourage plenty of oral fluids to aid digestion and prevent constipation. Small, frequent meals are often better tolerated.
Elimination
- Bladder and Bowel Care: Offer a bedpan or urinal. Observe urine and stool for color, amount, and consistency, and record on a fluid balance chart.
Hygiene
- Ensure comfort with daily bed baths and linen changes.
- Provide daily oral care to prevent complications like stomatitis and to stimulate appetite.
- Implement regular (e.g., 4-hourly) turning and pressure area care to prevent pressure sores, especially for debilitated patients on bed rest.
Physiotherapy / Exercises
Offer passive exercises while on bed rest. As the patient improves, encourage active exercises like deep breathing and gradual ambulation to prevent respiratory and circulatory complications (DVT, hypostatic pneumonia).
Advice on Discharge
Provide comprehensive health education to the patient and family:
- Medication: Take all medications as prescribed and complete the full course.
- Rest: Emphasize the need for adequate rest to allow the liver to regenerate.
- Diet: Continue a well-balanced diet. Strictly avoid alcohol as it is toxic to the liver.
- Hygiene: Reinforce infection control measures, especially hand washing, to prevent transmission.
- Follow-up: Return for review on the scheduled date for follow-up blood work and assessment. Advise them to return earlier if symptoms worsen or complications arise.