Table of Contents
ToggleINFECTIVE ENDOCARDITIS: Causes, Investigations, Management, and Nursing Interventions
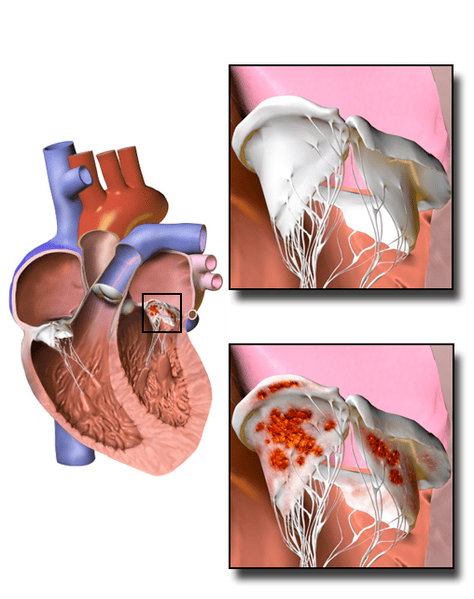
Infective Endocarditis (IE) is a severe and potentially life-threatening infection of the inner lining of the heart (the endocardium) and heart valves. It occurs when microorganisms, typically bacteria, enter the bloodstream and attach to damaged or abnormal heart valves or to areas of the endocardium, forming vegetations. These vegetations are composed of platelets, fibrin, inflammatory cells, and microorganisms, and can lead to valve destruction, embolization to other organs, and systemic infection.
I. Causes and Risk Factors of Infective Endocarditis (Etiology)
IE typically develops in individuals with pre-existing cardiac conditions or those with routes for bacteremia. The causative microorganisms are predominantly bacteria, but fungi can also be responsible, especially in immunocompromised individuals or those with indwelling catheters.
A. Microorganisms (Pathogens):
The type of pathogen often correlates with the route of infection and patient characteristics.
Staphylococci:- Staphylococcus aureus: The most common cause of acute IE, particularly in intravenous drug users (IVDUs), patients with prosthetic valves, and those with healthcare-associated infections. Known for rapid valve destruction and severe complications.
- Coagulase-negative Staphylococci (e.g., Staphylococcus epidermidis): Common cause of prosthetic valve endocarditis (PVE), especially early PVE, as they are part of normal skin flora and can contaminate surgical sites.
- Viridans group Streptococci (e.g., S. mutans, S. sanguinis, S. mitis): The most common cause of subacute IE, typically originating from the oral cavity (e.g., dental procedures, poor oral hygiene). Affects previously damaged native valves.
- Streptococcus gallolyticus (formerly S. bovis): Associated with gastrointestinal malignancies.
- Enterococci (e.g., Enterococcus faecalis, E. faecium): Common in older males with genitourinary or gastrointestinal tract procedures, often resistant to multiple antibiotics.
- Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella: Fastidious Gram-negative bacteria that are part of normal oral flora. Can cause large vegetations and embolic events, typically subacute.
- Candida species, Aspergillus species: Rare but highly lethal, seen in IVDUs, immunocompromised patients, or those with prolonged antibiotic use/central venous catheters. Often causes large vegetations.
- Gram-negative Bacilli: Pseudomonas aeruginosa, E. coli (rare).
- Culture-negative Endocarditis: Occurs when standard blood cultures fail to identify the pathogen, often due to prior antibiotic use, fastidious organisms (e.g., Coxiella burnetii, Bartonella spp., Tropheryma whipplei), or fungal infections.
B. Risk Factors:
Conditions that predispose individuals to bacteremia or provide a suitable surface for bacterial attachment.
Pre-existing Cardiac Conditions:- Prosthetic Heart Valves: Mechanical or bioprosthetic, highest risk due to foreign material.
- Previous Infective Endocarditis: Strongest risk factor for recurrence.
- Congenital Heart Disease: Unrepaired cyanotic heart disease, surgically repaired defects with residual shunts/regurgitation, bicuspid aortic valve (most common congenital lesion).
- Valvular Heart Disease: Rheumatic heart disease, degenerative valve disease (e.g., calcific aortic stenosis, mitral valve prolapse with regurgitation and thickened leaflets).
- Hypertrophic Obstructive Cardiomyopathy (HOCM).
- Intracardiac Devices: Pacemakers, implantable cardioverter-defibrillators (ICDs).
- Intravenous Drug Use (IVDU): Especially with unsterile injection practices; often affects the tricuspid valve.
- Intravascular Catheters: Central venous lines, PICCs, hemodialysis catheters.
- Dental Procedures: With gingival manipulation (high-risk procedures in patients with predisposing cardiac conditions). Poor oral hygiene is an ongoing risk.
- Other Invasive Procedures: Gastrointestinal, genitourinary, respiratory tract procedures, skin infections.
- Chronic Hemodialysis.
- HIV infection, malignancy, chemotherapy, immunosuppressive medications (e.g., post-transplant).
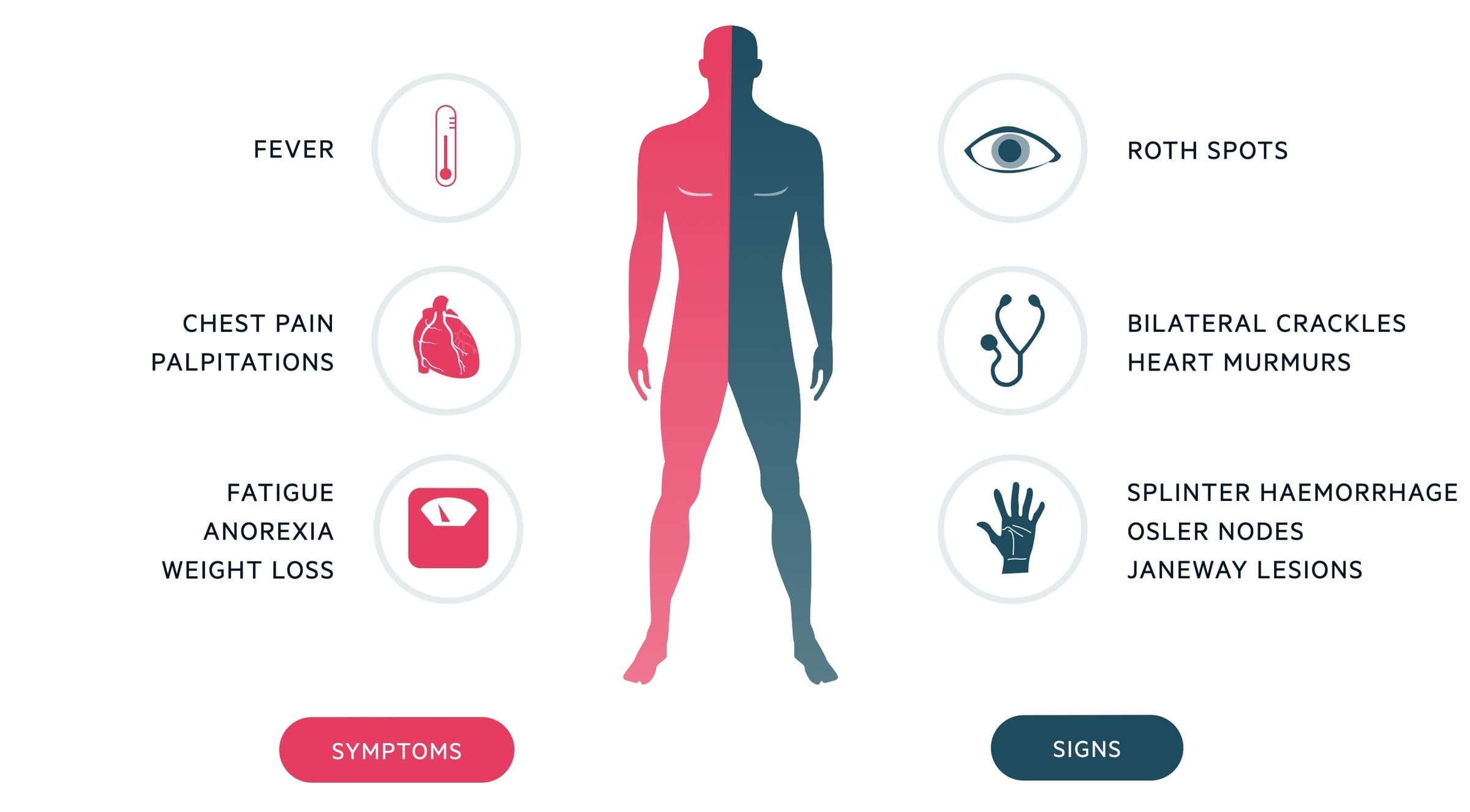
II. Clinical Manifestations (Signs and Symptoms) of Endocarditis
The clinical presentation of IE is diverse and can range from acute, rapidly progressing illness to a subacute, indolent course. Symptoms are often non-specific, making diagnosis challenging.
A. General and Constitutional Symptoms:
Common in both acute and subacute forms, reflecting systemic inflammation and infection.
- Fever: Present in >90% of cases, though may be absent in elderly, immunocompromised, or those with renal failure. May be intermittent.
- Chills, Sweats (especially night sweats).
- Fatigue, Malaise, Weakness.
- Anorexia and Weight Loss.
- Arthralgia (joint pain), Myalgia (muscle pain).
- Headache.
B. Cardiac Signs:
Reflect involvement of heart valves and potential heart failure.
- New or Changing Heart Murmur: The most important physical sign, occurring in up to 85% of cases. Due to valve destruction or altered blood flow.
- Signs of Heart Failure: Dyspnea, orthopnea, paroxysmal nocturnal dyspnea, peripheral edema, crackles in lungs, S3 gallop. Due to severe valvular regurgitation (e.g., aortic or mitral).
- Pericarditis/Myocarditis: Less common, but inflammation can extend to adjacent structures.
C. Embolic Phenomena (Systemic and Pulmonary):
Result from fragments of vegetations breaking off and traveling through the bloodstream.
- Systemic Embolism (Left-sided IE):
- Cerebral Emboli: Stroke (most common and serious), transient ischemic attack (TIA).
- Splenic Infarcts: Left upper quadrant pain, tenderness.
- Renal Infarcts: Flank pain, hematuria.
- Peripheral Arterial Emboli: Ischemia of limbs (pain, pallor, pulselessness, paresthesias, paralysis).
- Mycotic Aneurysms: Weakening of arterial walls due to infection, can rupture.
- Pulmonary Embolism (Right-sided IE, common in IVDUs):
- Recurrent pneumonia-like symptoms, pleuritic chest pain, dyspnea, hemoptysis.
- Septic pulmonary emboli can lead to lung abscesses.
D. Immunologic Phenomena:
Less specific but classic signs of IE, thought to be due to immune complex deposition or vasculitis.
- Osler's Nodes: Painful, tender, red or purplish nodules on finger or toe pads.
- Janeway Lesions: Non-tender, erythematous or hemorrhagic macules on palms and soles.
- Roth Spots: Retinal hemorrhages with pale centers on fundoscopic exam.
- Glomerulonephritis: Microscopic hematuria, proteinuria, renal dysfunction.
- Clubbing of Fingers and Toes: In chronic IE.
III. Investigations for Infective Endocarditis (Diagnosis)
Diagnosis of IE relies on a combination of clinical features, microbiological evidence, and echocardiographic findings, typically guided by the modified Duke Criteria.
A. Laboratory Tests:
- Gold Standard: At least three sets of blood cultures from different venipuncture sites, drawn at different times, before initiating antibiotic therapy.
- Yield: Positive in 90-95% of cases. Culture-negative IE requires specialized testing (e.g., serology for Coxiella burnetii, Bartonella, fungal cultures).
- ESR and CRP: Almost always elevated in active IE, but non-specific.
- Anemia: Common in chronic IE (anemia of chronic disease).
- Leukocytosis: May or may not be present.
- Monitor for glomerulonephritis or renal infarcts.
- May show microscopic hematuria (due to renal infarcts or glomerulonephritis).
B. Echocardiography:
Crucial for visualizing vegetations, assessing valvular damage, and evaluating cardiac function.
- Initial Imaging: Non-invasive, widely available. Good for visualizing large vegetations (>2-3 mm) on native valves, and assessing ventricular function.
- Limitations: Limited sensitivity for small vegetations, prosthetic valves, or in patients with poor acoustic windows.
- More Sensitive: Offers superior visualization of all four heart valves, prosthetic valves, perivalvular extensions (abscesses, fistulae), and smaller vegetations (<2-3 mm).
- Indications: Suspected IE with negative TTE, prosthetic valves, intracardiac devices, complicated IE, or when surgical intervention is contemplated.
C. Other Imaging:
- CT Scans (Chest, Abdomen, Brain):
- Purpose: To detect embolic events (e.g., splenic, renal, cerebral infarcts, mycotic aneurysms) or extracardiac infection.
- PET/CT (Positron Emission Tomography/Computed Tomography):
- Emerging Role: Particularly useful for diagnosing PVE and culture-negative IE by identifying areas of increased metabolic activity consistent with infection.
D. Modified Duke Criteria:
A set of clinical criteria used to classify the likelihood of IE (definite, possible, or rejected) based on major and minor criteria. Requires clinical judgment.
- Major Criteria:
- Positive blood cultures for IE-typical microorganisms (e.g., S. aureus, Viridans strep) or persistently positive cultures.
- Evidence of endocardial involvement by echocardiography (vegetation, abscess, new partial dehiscence of prosthetic valve, new regurgitation).
- Minor Criteria:
- Predisposition (predisposing heart condition or IVDU).
- Fever (temperature >38°C).
- Vascular phenomena (e.g., arterial emboli, septic pulmonary infarcts, mycotic aneurysm, conjunctival hemorrhages, Janeway lesions).
- Immunologic phenomena (e.g., glomerulonephritis, Osler's nodes, Roth spots, rheumatoid factor).
- Microbiological evidence (positive blood culture not meeting major criteria or serologic evidence of active infection with organism consistent with IE).
IV. Management and Treatment of Infective Endocarditis
Treatment of IE involves prolonged courses of high-dose intravenous antibiotics and, in many cases, surgical intervention. The goals are to eradicate the infection, prevent complications, and restore valvular function.
A. Antibiotic Therapy:
The cornerstone of IE treatment. Therapy is empiric initially, then tailored based on blood culture results and antibiotic sensitivities.
- Empiric Therapy:
- Choice: Broad-spectrum antibiotics covering likely pathogens (e.g., Staphylococci, Streptococci, Enterococci). Often involves combination therapy (e.g., Vancomycin + Ceftriaxone or Gentamicin).
- Initiation: Started after obtaining adequate blood cultures.
- Targeted Therapy:
- Adjustment: Based on identification of the pathogen and its antibiotic sensitivities.
- Duration: Typically 2-6 weeks of intravenous antibiotics. Longer courses are common for prosthetic valve endocarditis, fungal endocarditis, or difficult-to-treat organisms.
- Route: Primarily IV, often requiring PICC line insertion for outpatient management.
- Monitoring Antibiotic Levels:
- For certain antibiotics (e.g., Vancomycin, Gentamicin) to ensure therapeutic levels and minimize toxicity (e.g., nephrotoxicity, ototoxicity).
B. Surgical Intervention:
Up to 50% of patients with IE may require surgery. Timing of surgery is crucial and can be emergent, urgent, or elective.
- Indications for Surgery:
- Heart Failure: Due to severe valvular regurgitation (e.g., aortic or mitral valve destruction) refractory to medical therapy. This is the most common indication.
- Uncontrolled Infection: Persistent bacteremia despite appropriate antibiotic therapy (typically >7-10 days), perivalvular extension (abscess, fistula, pseudoaneurysm), or infection by resistant organisms (e.g., fungi, multidrug-resistant bacteria).
- Prevention of Embolism: Large vegetations (>10-15 mm, especially mobile vegetations on the anterior mitral leaflet), or recurrent embolic events despite appropriate antibiotics.
- Prosthetic Valve Dysfunction or Dehiscence.
- Surgical Procedures:
- Valve Repair: Whenever possible, especially for mitral valve.
- Valve Replacement: With mechanical or bioprosthetic valves.
- Debridement of Infected Tissue: Removal of vegetations and abscesses.
C. Management of Complications:
- Embolic Stroke: Medical management, potential anticoagulation (controversial in active IE due to risk of hemorrhagic transformation).
- Mycotic Aneurysm: May require surgical or endovascular repair.
- Renal Failure: Supportive care, dialysis if needed.
- Heart Block: Temporary or permanent pacemaker insertion.
D. Prophylaxis:
Antibiotic prophylaxis is recommended only for very specific high-risk cardiac conditions undergoing high-risk dental procedures.
- High-Risk Cardiac Conditions: Prosthetic heart valves, previous IE, unrepaired cyanotic congenital heart disease, repaired congenital heart disease with residual defects, cardiac transplant recipients who develop valvulopathy.
- High-Risk Dental Procedures: Involving manipulation of gingival tissue or periapical region of teeth, or perforation of the oral mucosa.
- Not Recommended: For routine dental cleanings in low-risk individuals, or for GI/GU procedures unless there is an active infection.
V. Nursing Interventions for Infective Endocarditis
Nursing care for patients with IE is complex, requiring vigilant monitoring, meticulous infection control, comprehensive medication management, and extensive patient education.
- Infection Control and Prevention:
- Aseptic Technique: Maintain strict aseptic technique during IV line insertion, dressing changes, and medication administration to prevent secondary infections.
- Catheter Care: Meticulous care for central venous catheters (PICC lines, CVCs) used for prolonged antibiotic therapy. Monitor insertion sites for signs of infection (redness, swelling, drainage, pain).
- Oral Hygiene: Encourage and assist with regular and thorough oral hygiene to reduce bacterial load.
- Skin Care: Assess and maintain skin integrity, especially in IV drug users, to prevent skin breakdown and source of infection.
- Medication Administration and Monitoring:
- Accurate IV Antibiotic Administration: Administer high-dose IV antibiotics on time, ensuring correct dilution and infusion rates.
- Monitor for Adverse Drug Reactions: Assess for common side effects (e.g., rash, nausea, diarrhea) and specific toxicities (e.g., nephrotoxicity, ototoxicity with aminoglycosides/vancomycin; monitor peak and trough levels as ordered).
- Anticoagulation Management: If on anticoagulants (e.g., for mechanical prosthetic valves), monitor INR/PTT and assess for bleeding.
- Pain Management: Administer analgesics as needed, assess pain effectiveness.
- Cardiac Monitoring and Assessment:
- Continuous Cardiac Monitoring: Observe for arrhythmias (e.g., new heart blocks due to perivalvular abscess) and signs of worsening heart failure.
- Frequent Vital Signs: Monitor temperature (fever patterns), heart rate, blood pressure, and respiratory rate for signs of infection progression or sepsis.
- Assess Heart Sounds: Auscultate regularly for new or changing heart murmurs, S3 gallop.
- Monitor for Signs of Heart Failure: Assess for dyspnea, orthopnea, crackles, JVD, peripheral edema, daily weights.
- Monitoring for Embolic and Immunologic Phenomena:
- Neurological Assessment: Frequent assessment for changes in mental status, new neurological deficits (e.g., weakness, numbness, speech changes) indicative of cerebral emboli.
- Peripheral Vascular Assessment: Check pulses, color, temperature, and sensation in all extremities for signs of peripheral emboli.
- Abdominal Assessment: Palpate for tenderness (splenic or renal infarcts).
- Skin and Eye Assessment: Inspect skin for Janeway lesions, Osler's nodes, petechiae. Fundoscopic exam for Roth spots if indicated.
- Urine Output: Monitor for hematuria or signs of renal impairment.
- Patient Education:
- Disease Process: Educate the patient and family about IE, its causes, complications, and the importance of prolonged antibiotic therapy.
- Medication Adherence: Emphasize the critical importance of completing the entire course of antibiotics, even if feeling better, to prevent relapse. Teach proper PICC line care if antibiotics are given at home.
- Oral Hygiene: Stress the importance of meticulous lifelong oral hygiene and regular dental check-ups.
- Prophylaxis: Educate high-risk patients about the need for antibiotic prophylaxis before specific dental procedures and provide them with an endocarditis prophylaxis card/information.
- Warning Signs: Instruct on signs and symptoms of recurrent IE (e.g., fever, new murmur) and when to seek immediate medical attention.
- Avoidance of IV Drug Use: For IVDU patients, provide counseling and referral to addiction treatment programs.
- Nutritional Support:
- Assess nutritional status; encourage a high-protein, high-calorie diet to support recovery and combat weight loss associated with chronic infection.
- Provide small, frequent meals if anorexia is an issue.
- Psychosocial Support:
- Address anxiety, fear, and depression associated with a serious illness, prolonged hospitalization, and potential surgical intervention.
- Encourage verbalization of feelings and provide emotional support.
- Facilitate communication between the patient/family and the healthcare team.
- Refer to social work or support groups if needed.
- Pre- and Post-Operative Care (if surgery is indicated):
- Standard cardiac surgical nursing care, including close hemodynamic monitoring, pain management, wound care, and early mobilization.