MYOCARDITIS: Causes, Investigations, Management, and Nursing Interventions
Myocarditis is an inflammatory disease of the heart muscle (myocardium) that can be caused by various factors, most commonly viral infections. It can affect people of any age, from infants to adults, and its clinical presentation can range from asymptomatic to severe heart failure, arrhythmias, or sudden cardiac death. The inflammation can lead to damage of the heart muscle cells, impairing the heart's ability to pump blood effectively.
I. Causes of Myocarditis (Etiology)
Myocarditis can stem from a wide array of sources, often categorized as infectious or non-infectious.
A. Infectious Causes:
These are the most common triggers for myocarditis, with viruses being the predominant culprits.
Viral Infections:- Enteroviruses: Coxsackievirus B (most common cause globally), Echovirus.
- Adenoviruses: Often associated with respiratory infections.
- Herpesviruses: Cytomegalovirus (CMV), Epstein-Barr Virus (EBV), Human Herpesvirus 6 (HHV-6).
- Influenza Virus: Types A and B.
- Parvovirus B19: Can cause persistent infection.
- HIV: Direct viral effect or opportunistic infections in immunocompromised individuals.
- SARS-CoV-2 (COVID-19): Myocarditis has been recognized as a complication of COVID-19 infection.
- Spirochetes: Lyme disease (Borrelia burgdorferi), Syphilis (Treponema pallidum).
- Streptococcus: Post-streptococcal acute rheumatic fever can lead to myocarditis.
- Staphylococcus, Corynebacterium diphtheriae (Diphtheria): Diphtheria toxin can directly damage myocardial cells.
- Mycoplasma pneumoniae, Chlamydia pneumoniae.
- Rare, typically seen in immunocompromised individuals.
- Examples: Candida, Aspergillus, Histoplasma, Coccidioides.
- Trypanosoma cruzi (Chagas Disease): Endemic in Central and South America, causes chronic cardiomyopathy.
- Toxoplasma gondii.
B. Non-Infectious Causes:
These include autoimmune conditions, toxins, and drug reactions.
- Systemic Lupus Erythematosus (SLE): Can cause inflammation of various organs, including the heart.
- Rheumatoid Arthritis.
- Scleroderma, Sarcoidosis: Granulomatous inflammation in the myocardium.
- Inflammatory Bowel Disease (IBD): (Crohn's disease, Ulcerative colitis).
- Giant Cell Myocarditis: A rare but aggressive form of myocarditis requiring prompt immunosuppression.
- Eosinophilic Myocarditis: Associated with hypereosinophilic syndromes, parasitic infections, or drug reactions.
- Alcohol: Chronic abuse can lead to alcoholic cardiomyopathy, which has an inflammatory component.
- Chemotherapeutic Agents: Anthracyclines (e.g., Doxorubicin), Cyclophosphamide, Trastuzumab.
- Illicit Drugs: Cocaine, Amphetamines.
- Environmental Toxins: Heavy metals (e.g., lead), carbon monoxide.
- Hypersensitivity Reactions: Penicillins, Sulfonamides, Phenytoin, Methyldopa, Clozapine.
- Radiation Therapy: To the chest for cancer treatment.
- Heatstroke, Electric Shock.
- When no specific cause can be identified despite thorough investigation. Many cases presumed viral fall into this category retrospectively.
II. Clinical Manifestations (Signs and Symptoms) of Myocarditis
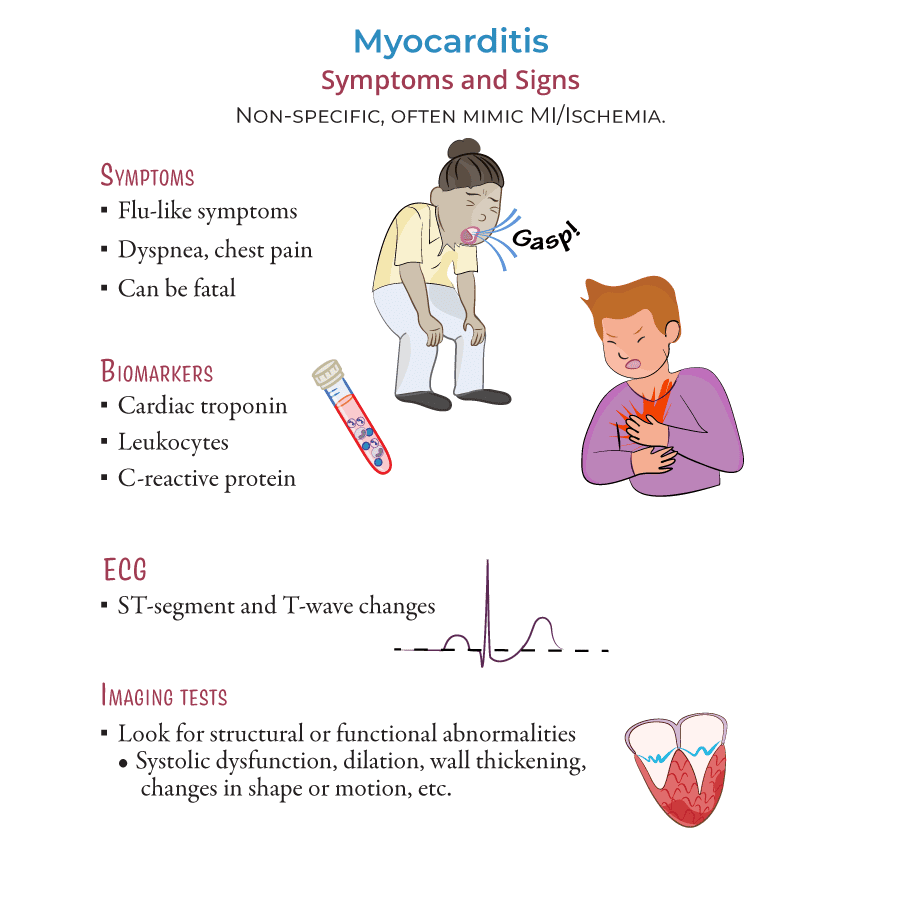
The presentation of myocarditis is highly variable, depending on the severity of inflammation, extent of myocardial damage, and the patient's immune response. Symptoms can mimic other cardiac or non-cardiac conditions.
Cardiac Symptoms:- Chest Pain: Can be sharp, stabbing, or dull, often mimicking myocardial infarction or pericarditis. May be pleuritic.
- Dyspnea (Shortness of Breath): On exertion or at rest, due to impaired cardiac function and potential heart failure.
- Fatigue and Weakness: Common, often profound, resulting from reduced cardiac output.
- Palpitations or Arrhythmias: Due to inflammation affecting the heart's electrical conduction system (e.g., premature beats, atrial fibrillation, ventricular tachycardia).
- Signs of Heart Failure: Peripheral edema, jugular venous distension (JVD), crackles in lungs, S3 gallop.
- Syncope or Near-Syncope: Due to arrhythmias or severely reduced cardiac output.
- Sudden Cardiac Death: In severe cases, due to malignant arrhythmias.
- Fever, Chills, Body Aches, Headache: Often preceding or accompanying viral infections.
- Myalgia (Muscle Pain), Arthralgia (Joint Pain): Common with systemic inflammatory responses.
- Upper Respiratory or Gastrointestinal Symptoms: Sore throat, cough, nausea, vomiting, diarrhea (often preceding viral myocarditis).
- Rash: Seen in some systemic or drug-induced causes.
- Many cases of myocarditis may be subclinical and resolve spontaneously without causing noticeable symptoms or long-term damage.
III. Investigations for Myocarditis (Diagnosis)
Diagnosing myocarditis can be challenging due to its varied presentation and the lack of a single definitive non-invasive test. A combination of clinical assessment, laboratory tests, imaging, and sometimes biopsy is required.
- History: Recent viral illness, exposure to toxins/drugs, autoimmune conditions, family history of cardiomyopathy. Detailed description of symptoms.
- Physical Exam: Auscultation for heart murmurs, S3 gallop, pericardial rub (if myopericarditis), signs of heart failure (rales, edema, JVD).
- Cardiac Biomarkers:
- Troponin I or T: Elevated in acute myocardial injury/inflammation. High sensitivity troponins are very sensitive.
- Creatine Kinase (CK) and CK-MB: May be elevated but less specific than troponin.
- Inflammatory Markers:
- C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Non-specific indicators of inflammation, often elevated.
- Complete Blood Count (CBC): Leukocytosis (elevated white blood cells) or eosinophilia (in eosinophilic myocarditis).
- Viral Serology/PCR: For specific viruses (e.g., Coxsackievirus, Adenovirus, HIV). May help identify the underlying cause but not always diagnostic of active cardiac involvement.
- Autoimmune Panel: Antinuclear antibodies (ANA), rheumatoid factor (RF), anti-dsDNA, ANCA if autoimmune etiology suspected.
- Renal and Liver Function Tests: To assess systemic effects or rule out other causes.
- Findings: Highly variable and non-specific. Can include:
- Sinus tachycardia (most common).
- Non-specific ST-T wave changes (ST elevation or depression, T wave inversion).
- Conduction abnormalities (bundle branch blocks, AV blocks).
- Arrhythmias (atrial fibrillation, premature ventricular contractions, ventricular tachycardia).
- Q waves (suggesting myocardial damage, but can be non-ischemic).
- Purpose: Assesses cardiac function, chamber size, wall motion abnormalities, and valvular function.
- Findings: Often shows left ventricular dysfunction (reduced ejection fraction), regional or global wall motion abnormalities, ventricular dilatation, and occasionally pericardial effusion (in myopericarditis).
- Purpose: Considered the gold standard non-invasive imaging technique for diagnosing myocarditis.
- Findings: Can detect myocardial edema (swelling), hyperemia (increased blood flow), and late gadolinium enhancement (LGE), which indicates myocardial fibrosis or necrosis. Uses "Lake Louise Criteria" for diagnosis.
- Purpose: The definitive diagnostic test, but rarely performed due to its invasive nature, patchy nature of the disease (sampling error), and risk of complications.
- Indications: Reserved for patients with rapidly progressive heart failure, life-threatening arrhythmias, or when specific etiologies (e.g., giant cell myocarditis, eosinophilic myocarditis) require specific immunosuppressive therapy.
- Findings: Histological examination shows inflammatory infiltrates with myocyte necrosis. Immunohistochemistry can identify specific inflammatory cell types.
IV. Management and Treatment of Myocarditis
Treatment is primarily supportive, aiming to manage symptoms, improve cardiac function, and prevent complications. Specific therapies are employed for identifiable causes.
A. General Supportive Care:
- Rest: Physical rest is crucial to reduce myocardial workload and promote healing. Strenuous exercise should be avoided during the acute phase and for several months.
- Management of Heart Failure:
- Diuretics: To reduce fluid overload and pulmonary congestion.
- ACE Inhibitors/ARBs: To reduce afterload and improve ventricular function.
- Beta-blockers: Once stable, to improve left ventricular function and control heart rate.
- Digoxin: May be used in specific cases to improve contractility.
- Arrhythmia Management:
- Antiarrhythmic Drugs: To control symptomatic arrhythmias.
- Temporary Pacing: For severe bradyarrhythmias or heart blocks.
- Implantable Cardioverter-Defibrillator (ICD): For persistent risk of malignant ventricular arrhythmias.
- Pain Management:
- NSAIDs: Generally avoided in pure myocarditis due to potential for worsening inflammation or renal effects, but may be used cautiously if there's a strong pericarditis component (myopericarditis) and no significant heart failure.
- Acetaminophen: Preferred for pain and fever control in pure myocarditis.
- Mechanical Circulatory Support:
- For severe, refractory heart failure or cardiogenic shock (e.g., Intra-aortic balloon pump (IABP), Extracorporeal membrane oxygenation (ECMO), Ventricular assist devices (VADs)).
- Cardiac Transplantation:
- In cases of irreversible, end-stage heart failure despite maximal medical therapy.
B. Specific Therapies (Targeted Treatment):
- Immunosuppressive Therapy:
- Corticosteroids: May be used in certain forms of myocarditis (e.g., giant cell myocarditis, eosinophilic myocarditis, sarcoidosis, lupus myocarditis) where there's an active inflammatory or autoimmune process. Generally not recommended for viral myocarditis.
- Other Immunosuppressants: Azathioprine, Cyclosporine, Mycophenolate mofetil in specific autoimmune cases.
- Antiviral Therapy:
- Not routinely used for acute viral myocarditis, as most cases resolve spontaneously. May be considered for specific viruses like HIV or CMV in certain contexts.
- Antibiotic/Antiparasitic/Antifungal Therapy:
- For bacterial, parasitic (e.g., Chagas disease), or fungal causes.
- Intravenous Immunoglobulin (IVIG):
- Some studies suggest a benefit in certain viral-induced myocarditis, but evidence is not conclusive and not routinely recommended.
V. Nursing Interventions for Myocarditis
Nursing care for patients with myocarditis is multifaceted, focusing on symptomatic relief, monitoring for complications, optimizing cardiac function, and providing emotional support and education.
- Cardiac Monitoring and Assessment:
- Continuous ECG Monitoring: To detect arrhythmias (tachycardia, bradycardia, blocks) and ST-T wave changes. Report any significant changes immediately.
- Frequent Vital Signs: Monitor heart rate, blood pressure, respiratory rate, and oxygen saturation regularly.
- Assess for Signs of Worsening Heart Failure: Monitor for increasing dyspnea, orthopnea, crackles in lungs, S3 gallop, peripheral edema, weight gain, and JVD.
- Auscultate Heart Sounds: Listen for muffled heart sounds, new murmurs, or pericardial friction rubs (if myopericarditis).
- Assess Peripheral Perfusion: Check skin temperature, color, capillary refill, and peripheral pulses.
- Activity Management and Rest Promotion:
- Strict Bed Rest: During the acute phase to reduce myocardial workload. Progress activity slowly as tolerated and as per physician orders.
- Assist with ADLs: Help with personal care to conserve patient energy and reduce cardiac demand.
- Provide a Quiet Environment: Minimize disturbances to promote rest and reduce anxiety.
- Educate on Activity Restrictions: Explain the importance of avoiding strenuous physical activity for several months (typically 3-6 months or more, depending on recovery) to allow for myocardial healing.
- Pain and Symptom Management:
- Assess Pain: Regularly assess chest pain characteristics (location, quality, severity, precipitating/alleviating factors).
- Administer Analgesics: As prescribed, typically acetaminophen, avoiding NSAIDs if possible unless specifically ordered for a pericarditis component.
- Positioning: Elevate the head of the bed to ease breathing and reduce cardiac workload.
- Manage Fever: Administer antipyretics as ordered.
- Fluid Balance and Nutrition:
- Monitor I&O: Accurately record all fluid intake and output.
- Daily Weights: Monitor for fluid retention (suggesting worsening heart failure) or dehydration.
- Administer Diuretics: As prescribed, and monitor for effectiveness and electrolyte imbalances (e.g., hypokalemia).
- Sodium and Fluid Restriction: If signs of fluid overload or heart failure are present, educate the patient on dietary restrictions.
- Medication Administration and Monitoring:
- Administer prescribed medications (e.g., ACE inhibitors, beta-blockers, antiarrhythmics, immunosuppressants) and monitor for their therapeutic effects and adverse reactions.
- Educate the patient about each medication, its purpose, dosage, and side effects.
- Psychosocial Support and Education:
- Address Anxiety and Fear: Acknowledge the patient's concerns regarding their cardiac condition. Provide reassurance and clear, concise information.
- Education on Disease Process: Explain myocarditis, its potential causes, symptoms, and the importance of adhering to the treatment plan.
- Risk Factor Modification: If applicable (e.g., abstinence from alcohol, illicit drugs).
- Warning Signs: Educate patient and family on signs and symptoms that require immediate medical attention (e.g., worsening dyspnea, chest pain, syncope, significant swelling).
- Coping Strategies: Help the patient develop coping strategies for managing chronic fatigue or activity limitations.
- Referrals: Consider referrals to cardiac rehabilitation, social work, or support groups as appropriate.
- Prevention of Complications:
- Infection Control: Practice strict aseptic technique for any invasive procedures.
- Skin Integrity: Reposition frequently and provide skin care, especially if on prolonged bed rest.
- Deep Vein Thrombosis (DVT) Prophylaxis: Implement measures such as sequential compression devices (SCDs) or anticoagulant therapy as ordered, given reduced mobility.