Osteopenia of Prematurity (OOP) is a metabolic bone disease characterized by reduced bone mineral density (BMD) in premature infants.
It results from a failure to accumulate adequate calcium and phosphate during critical periods of rapid bone mineralization in the late third trimester of pregnancy. Prematurity affects bone mineralization and bone growth—thus the condition osteopenia of prematurity.
Essentially, premature infants miss out on the crucial placental transfer of these minerals, which normally occurs most rapidly between 28 and 40 weeks of gestation. This deficiency leads to bones that are weaker and more fragile than those of full-term infants.
- Reduced bone mineral content: The primary feature is a lower-than-normal amount of bone mineral.
- Increased bone fragility: The bones are weaker and more susceptible to fractures.
- Usually asymptomatic in mild cases: It can often go unnoticed unless it leads to complications like fractures.
- Primarily affects very low birth weight (VLBW) and extremely low birth weight (ELBW) infants: These infants are at the highest risk due to their extreme prematurity.
In simple terms, OOP is like "soft bones" in premature babies because they didn't get enough building blocks for strong bones while still in the womb.
Osteopenia of prematurity is the decrease in the amount of calcium and phosphorus in bones which makes the bones weak and brittle resulting into broken bones.
- Reduced Mineral Accretion:
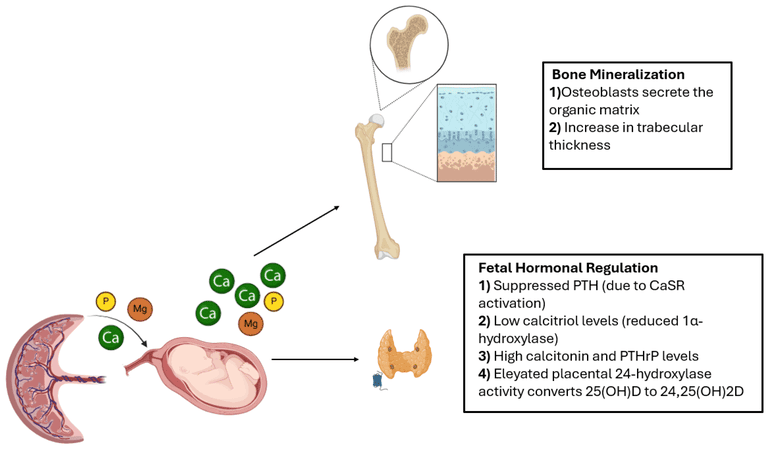
- Normal In Utero Mineralization: During the third trimester of pregnancy (especially from 28 to 40 weeks), there is a rapid and massive placental transfer of calcium and phosphorus from the mother to the fetus. The fetus accumulates approximately 80% of its total body calcium and phosphorus during this period.
- Premature Interruption: When an infant is born prematurely, this crucial period of high mineral accretion is abruptly halted. The infant is then reliant on enteral or parenteral nutrition, which often cannot match the efficiency and volume of mineral transfer achieved via the placenta.
- Bone Formation vs. Resorption Imbalance: The rate of bone formation is significantly reduced due to insufficient mineral supply, while bone resorption (breakdown) continues, leading to a net loss of bone mass.
- Nutritional Deficiencies:
- Inadequate Calcium and Phosphorus Intake:
- Parenteral Nutrition (PN): While PN solutions provide calcium and phosphorus, the solubility limits can restrict the amounts that can be safely administered, often falling short of intrauterine accretion rates.
- Enteral Nutrition: Breast milk, while ideal for term infants, has lower concentrations of calcium and phosphorus than required for the rapid growth of premature infants. Standard infant formulas also may not meet these elevated needs. Fortification of breast milk or specialized premature formulas are often required.
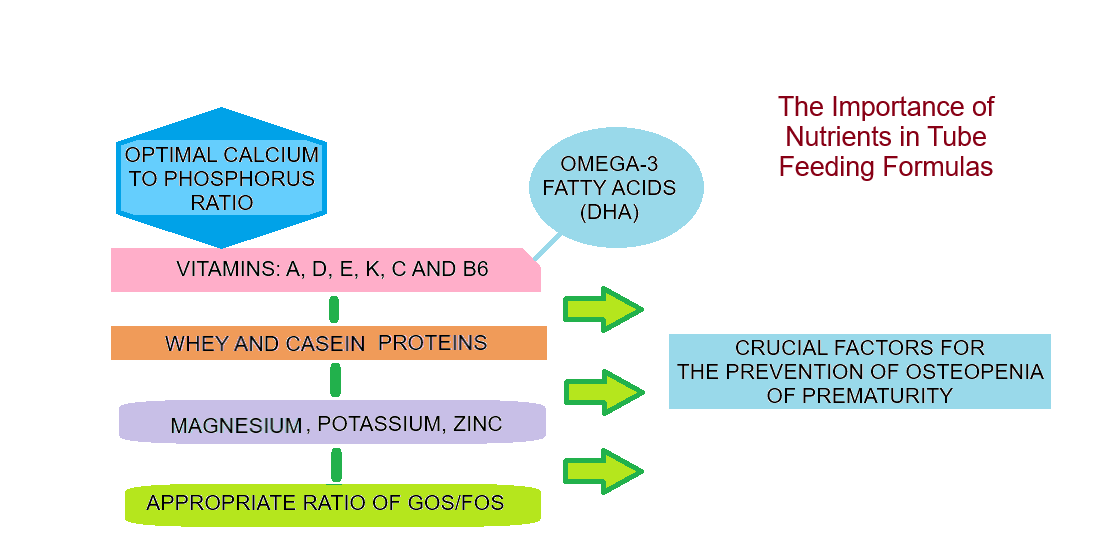
- Vitamin D Deficiency: Vitamin D is crucial for calcium and phosphorus absorption and bone mineralization. Premature infants may have insufficient stores due to prematurity, and inadequate exogenous intake can exacerbate this.
- Other Micronutrients: Deficiencies in vitamins A, C, and K, and minerals like magnesium and zinc can also indirectly impact bone health.
- Inadequate Calcium and Phosphorus Intake:
- Hormonal Imbalances and Immaturity:
- Calciotropic Hormones: The regulatory systems involving parathyroid hormone (PTH), calcitonin, and vitamin D metabolites (1,25-dihydroxyvitamin D) are immature in preterm infants. This immaturity can lead to inefficient regulation of calcium and phosphorus homeostasis.
- Growth Factors: Insulin-like growth factor 1 (IGF-1) and other growth factors play roles in bone growth and mineralization. Levels may be suboptimal in premature infants.
- Reduced Mechanical Loading (Immobility):
- Lack of Fetal Movement: In utero, fetal movements provide crucial mechanical stimulation to the developing skeleton, promoting bone formation.
- Postnatal Immobility: Premature infants, especially those critically ill or on ventilators, experience prolonged periods of immobility. This lack of weight-bearing and muscle activity reduces osteoblast (bone-forming cell) activity and increases osteoclast (bone-resorbing cell) activity, contributing to bone demineralization.
The primary etiological factor is prematurity itself, leading to:
- Interruption of Third-Trimester Mineral Transfer: This is the most significant single factor.
- Physiological Immaturity:
- Immature gastrointestinal tract, leading to reduced absorption of minerals.
- Immature renal function, affecting mineral reabsorption and excretion.
- Immature endocrine system, impacting calciotropic hormone regulation.
- Liver problems which may lead to deficiency of vitamin D e.g cholestasis(obstruction of bile flow).
- Medical Interventions and Comorbidities:
- Prolonged Parenteral Nutrition: As mentioned, limits on mineral content.
- Diuretic Use: Loop diuretics (e.g., furosemide) can increase urinary excretion of calcium.
- Corticosteroid Use: Often used in premature infants for lung maturation or chronic lung disease, corticosteroids can directly inhibit osteoblast function and promote bone resorption.
- Chronic Lung Disease (Bronchopulmonary Dysplasia - BPD): Infants with BPD often require prolonged ventilation, corticosteroids, and diuretics, further exacerbating OOP.
- Small for Gestational Age (SGA): Infants who are SGA may have had poor nutrient accretion even before premature birth.
- Sepsis/Inflammation: Chronic inflammation can negatively impact bone metabolism.
- Extreme Prematurity and Low Birth Weight:
- Gestational Age < 30-32 weeks: This is the most significant risk factor. The earlier the birth, the greater the deficit in intrauterine mineral accretion.
- Very Low Birth Weight (VLBW < 1500g) and Extremely Low Birth Weight (ELBW < 1000g): These infants typically have the shortest intrauterine mineral accretion period and are consequently at the highest risk.
- Inadequate Mineral and Vitamin D Intake:
- Prolonged Parenteral Nutrition (PN) without adequate mineral supplementation.
- Feeding with unfortified breast milk or standard infant formula.
- Inadequate Vitamin D supplementation.
- Chronic Medical Conditions and Comorbidities:
- Bronchopulmonary Dysplasia (BPD) / Chronic Lung Disease.
- Gastrointestinal Malabsorption Issues.
- Renal Disease.
- Medications:
- Corticosteroids.
- Loop Diuretics (e.g., Furosemide).
- Prolonged Immobility and Lack of Mechanical Loading:
- Prolonged ventilation/sedation.
- Neuromuscular disorders.
- Other Factors:
- Maternal Factors: Maternal vitamin D deficiency, preeclampsia, smoking, thin body habitus, low Calcium intake.
- Exposure to high doses of magnesium in utero.
- Higher incidence of postnatal rickets in infants with intrauterine growth restriction.
- Increased maternal parity and boys have higher incidence.
- Placental hormones imbalance.
In its mild to moderate forms, OOP is often asymptomatic, meaning there are no obvious signs. The signs usually appear when the condition is more severe or has led to complications.
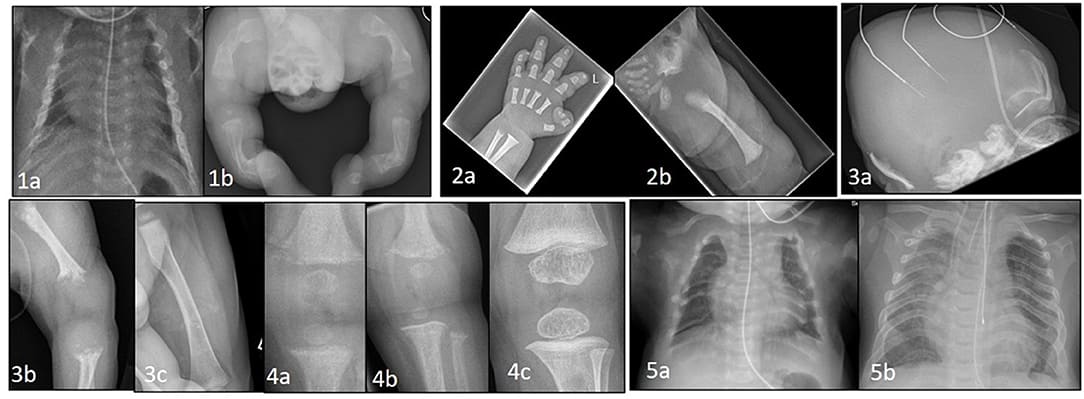
- Fractures: This is often the first and most dramatic clinical sign, especially of long bones (e.g., femur, humerus, ribs) or even vertebral compression fractures. These can occur with minimal trauma, or even during routine handling or diaper changes.
- Bone Deformities: Rickets-like changes can occur in severe cases, such as:
- Craniotabes: Softening of the skull bones.
- Rosary chest: Enlargement of the costochondral junctions.
- Widened wrists and ankles.
- Bowing of long bones.
- Poor growth/failure to thrive: Skeletal pain or generalized weakness can contribute to poor feeding and weight gain.
- Limited limb movement: Could be due to pain from microfractures or reluctance to move due to skeletal weakness.
- Increased respiratory support needs: Weak ribs due to demineralization can lead to a less stable chest wall, making ventilation more challenging.
- Recurrent respiratory infections.
- Hypotonia: Generalized muscle weakness can sometimes be associated.
- Elevated Alkaline Phosphatase (ALP): Persistently very high ALP levels can be a strong clinical indicator of active demineralization.
Diagnosis relies on a combination of biochemical tests and imaging studies, often in conjunction with identified risk factors.
- Alkaline Phosphatase (ALP): This is the most sensitive biochemical indicator. High levels (especially >500 IU/L, or often >800-1000 IU/L) suggest significant bone turnover and demineralization.
- Serum Phosphorus (Phosphate): Often low (< 4.0 mg/dL), suggestive of inadequate intake.
- Serum Calcium: Usually maintained within normal range but can be low.
- 25-hydroxyvitamin D [25(OH)D]: Assesses vitamin D status.
- Parathyroid Hormone (PTH): Often elevated.
- Urine Calcium and Phosphorus: Can help assess renal losses or adequacy of intake.
- Conventional Radiography (X-rays): Often the primary imaging modality.
- Findings: Generalized osteopenia ("washed out" bones), Metaphyseal fraying and cupping, Cortical thinning, Fractures, Bone modeling deformities.
- Limitation: Requires significant bone demineralization (20-40%) to be detectable.
- Dual-energy X-ray Absorptiometry (DXA) / Peripheral Quantitative Computed Tomography (pQCT): Considered the "gold standard" for quantifying bone density but not routinely available in all NICUs.
Prevention is paramount in neonatal care. Strategies focus primarily on optimizing mineral and vitamin D intake and promoting physical activity.
This is the cornerstone of OOP prevention, aiming to mimic the intrauterine mineral accretion rates.
- Early and Aggressive Nutritional Support:
- Parenteral Nutrition (PN): Early initiation with adequate calcium and phosphorus.
- Enteral Nutrition: Breast milk fortification and use of specialized preterm infant formulas to ensure adequate intake volume.
- Vitamin D Supplementation: Early and consistent supplementation (400-800 IU/day).
- Monitor Biochemical Markers: Serial monitoring of ALP, phosphorus, and calcium.
- Careful Use of Medications: Judicious use of corticosteroids and loop diuretics.
- Addressing Underlying Medical Conditions: Optimize management of chronic lung disease (BPD) and gastrointestinal issues.
- Early Mobilization and Positioning: Physiological positioning and supported handling.
- "Kangaroo Care": Skin-to-skin contact.
- Physical Therapy: Individualized programs for gentle movement.
- Maternal Vitamin D Supplementation during pregnancy.
The management and treatment are closely intertwined with prevention.
Aims
- To restore normal calcium and phosphorus in the body
- To prevent further complications or disease progress
The child is admitted to pediatric ward in case the child is referred from outside the hospital.
- Demographic data: Name, age, sex, etc.
- Detailed medical and obstetric history: Pre-natal and natal data, birth weight, APGAR score at birth history are taken.
- Physical examination: Done from head to toe, with more emphasis on bone formation to notify any abnormalities.
- Comfort and warmth: Baby is put in a comfortable, warm bed to prevent hypothermia.
- Pain relief: Analgesics like paracetamol 2.5mg 8-hourly for three days are administered to relieve pain which may be due to unknown fractures.
- Fracture immobilisation: Done in case of fractures, which helps to maintain the bone in position.
- Doctor's assessment: Doctor is called who will perform a quick assessment and order investigations.
Investigations will include:
- Blood tests: To detect calcium and phosphorus levels and a protein called alkaline phosphatase.
- Ultrasound: To rule out fractures.
- X-rays: To rule out the extent of fractures.
The following treatment is administered to the patient as prescribed by the doctor:
- Calcium administration: 1.25mmol/kg/dose added to IV fluids like normal saline and Ringer's lactate given until the condition is stable.
- IV Phosphorus administration: 1mmol/kg/dose added to IV fluids until the condition stabilizes.
- Vitamin D supplements: Given to children with liver problems.
- Ensure warmth and comfort: Keep the baby warm and comfortable.
- Vital observations: Monitoring of vital observations i.e. TPR.
- Nutritional support: Ensure the patient is getting a diet rich in calcium and phosphorus by feeding the baby with fortified milk.
- Physical exercises: Encouraged by the physiotherapists.
- Rest and sleep: Ensure the baby is getting adequate rest and sleep by providing a conducive environment.
- Psychological care: Provided to the mother to allay anxiety.
- Hygiene promotion: Both environmental and personal hygiene is promoted to prevent cross infection.
- Medication administration: As prescribed by the doctor.
- Weekly monitoring: Of urine calcium, phosphorus.
- Discharge consideration: When the patient improves.
- Increased Calcium and Phosphorus Supplementation: Goal is to provide higher intakes to support rapid bone mineralization.
- Optimize PN solutions.
- Fortify breast milk or use specialized post-discharge formulas.
- Individual mineral supplements if needed.
- Vitamin D Supplementation: Increased doses may be required for confirmed OOP.
- Monitoring of Biochemical Markers: Frequent assessment to guide adjustments.
- Management of Fractures: Careful handling, appropriate immobilization (splinting), and pain management.
- Promoting Physical Activity and Mobility: Gentle passive range of motion, therapeutic positioning, collaboration with PT.
- Addressing Underlying Conditions: Optimization of chronic lung disease and GI management.
- Pharmacological Agents: Bisphosphonates (rarely used, for severe intractable cases).
- Continued Nutritional Support Post-Discharge.
- Regular Monitoring of growth and bone health.
- Parental Education on safe handling and nutrition.
- Multidisciplinary Approach.
Nurses play a pivotal role in the prevention, identification, and management of OOP.
- Clinical Observation: Activity and movement, signs of pain, respiratory status, skeletal changes, and growth.
- Biochemical Monitoring: Timely blood draws and trend analysis.
- Radiological Monitoring: Awareness of X-ray findings.
- Accurate Preparation and Administration of Feeds: Fortification, mineral supplements, and proper PN infusion.
- Hydration: Ensure adequate hydration to prevent kidney stones.
- Gentle Handling Techniques: Minimize trauma, use two-person lift, gentle rolling during care.
- Therapeutic Positioning: Physiological alignment, pressure relief, and safe movement encouragement.
- Awareness of bone-affecting medications and monitoring for side effects.
- Educate on OOP causes and risks.
- Safe handling demonstration and practice.
- Nutritional instructions and signs of concern.
- Emotional support.
- Interdisciplinary team communication and accurate documentation.
Related to bone demineralization and fragility. Definition: Susceptible to accidental physical injury that is severe enough to require intervention, which may compromise health.
| Intervention | Rationale |
|---|---|
| 1. Gentle Handling Techniques: Support head and all limbs during repositioning, lifting, and diaper changes. Avoid sudden or forceful movements. | Minimizes stress on fragile bones, reducing the likelihood of microfractures or overt fractures caused by external forces. |
| 2. Two-Person Lift: When transferring the infant (especially larger ones), use a two-person lift to ensure even support. | Distributes the infant's weight evenly, preventing uneven pressure on specific bones that could lead to fractures. |
| 3. Proper Positioning: Utilize nesting devices, rolls, and blankets to maintain physiological flexion and support the body. | Promotes comfort and stability, preventing uncontrolled limb movements that could strain bones. Reduces pressure on bony prominences. |
| 4. Observe for Signs of Pain/Discomfort: Continuously assess for grimacing, crying, irritability, limb guarding, or changes in vital signs. | Early detection of pain or discomfort may indicate a new or impending fracture, allowing for prompt assessment and intervention. |
| 5. Educate Parents/Caregivers on Safe Handling: Demonstrate and allow return demonstration of all handling techniques. | Empowers parents to provide safe care, preventing accidental trauma once the infant is discharged home, fostering confidence and reducing anxiety. |
Related to inability to absorb or ingest adequate nutrients and minerals for bone growth. Definition: Intake of nutrients insufficient to meet metabolic needs.
| Intervention | Rationale |
|---|---|
| 1. Administer Fortified Breast Milk or Specialized Preterm Formula: Prepare and administer exactly as prescribed by the dietitian/physician. | Provides essential increased calories, protein, calcium, phosphorus, and other micronutrients critical for bone mineralization and overall growth that standard milk lacks. |
| 2. Administer Prescribed Mineral/Vitamin D Supplements: Ensure accurate dosing and timing of calcium, phosphorus, and vitamin D supplements. | Directly addresses the mineral and vitamin D deficiencies that are central to OOP, promoting absorption and utilization for bone growth. |
| 3. Monitor Feeding Tolerance: Assess for gastric residuals, abdominal distension, emesis, and stool characteristics. | Ensures the infant is tolerating the feeds and absorbing nutrients effectively. Poor tolerance may require adjustments to feeding volume, rate, or type. |
| 4. Monitor Weight, Length, and Head Circumference: Plot on appropriate growth charts regularly. | Provides objective data on growth progression, indicating the adequacy of nutritional intake and the effectiveness of interventions. |
| 5. Monitor Biochemical Markers: Review labs (ALP, Phos, Ca, 25(OH)D) and trend results. | Guides nutritional adjustments and monitors the body's response to interventions, indicating if mineral levels are improving or worsening. |
| 6. Consult with a Neonatal Dietitian: | Ensures individualized nutritional plans are optimized based on the infant's specific needs, tolerance, and lab results. |
Related to bone pain, fragility, and restricted movement. Definition: Limitation in independent, purposeful physical movement of the body or one or more extremities.
| Intervention | Rationale |
|---|---|
| 1. Pain Assessment and Management: Continuously assess for pain and administer analgesia as prescribed (if pain is identified, e.g., from a fracture). | Alleviating pain encourages spontaneous movement and reduces the infant's reluctance to move, promoting comfort and participation in therapeutic activities. |
| 2. Gentle Passive Range-of-Motion (PROM) Exercises: If ordered by PT, perform carefully and within the infant's pain tolerance. | Helps maintain joint flexibility, stimulates bone growth (due to gentle mechanical loading), and prevents contractures without causing trauma. |
| 3. Encourage "Tummy Time" (Supervised): For infants able to tolerate it. | Promotes strengthening of neck and upper body muscles, provides gentle weight-bearing, and contributes to motor development milestones. |
| 4. Utilize Positioning Aids: Use rolls and pillows to position the infant to allow for spontaneous, safe movements. | Supports the infant in positions that facilitate movement while ensuring safety and comfort, promoting self-initiated activity. |
| 5. Collaborate with Physical/Occupational Therapy: | Provides specialized expertise in therapeutic exercises, positioning, and developmental interventions to enhance mobility and minimize long-term impairments. |
Related to the disease process of OOP, treatment regimen, and safe care at home. Definition: Absence or deficiency of cognitive information related to a specific topic.
| Intervention | Rationale |
|---|---|
| 1. Provide Information on OOP: Explain the condition, its causes, and potential complications in clear, understandable language. | Enhances parental understanding of the infant's condition, reducing anxiety and promoting active participation in care. |
| 2. Demonstrate and Supervise Return Demonstration of Safe Handling Techniques: Emphasize the "how-to" and "why." | Builds parental confidence and competence in safely handling their fragile infant, preventing accidental injury at home. |
| 3. Provide Clear Written Instructions for Nutritional Care: Include details on formula preparation, fortification, and supplement administration. | Ensures accuracy and consistency of nutritional interventions at home, which is critical for bone mineralization and growth. |
| 4. Educate on Signs of Concern: Instruct parents on symptoms requiring medical attention (e.g., increased irritability, swelling of a limb, refusal to move an extremity). | Empowers parents to identify potential complications early, facilitating prompt medical intervention and preventing worsening outcomes. |
| 5. Discuss Follow-up Care: Explain the importance of regular clinic visits and multidisciplinary team appointments. | Ensures continuity of care, ongoing monitoring of bone health, and timely adjustments to treatment plans post-discharge. |
| 6. Provide Resources and Support: Offer information on support groups or community resources if available. | Helps parents cope with the challenges of caring for a medically fragile infant and connects them with additional support systems. |
While Osteopenia of Prematurity (OOP) can often be managed effectively, if left untreated or in severe cases, it can lead to a range of significant complications.
- Bone Fractures: The most common complication. Causes pain and prolongs hospitalization.
- Rickets: Severe, prolonged OOP can lead to overt rickets (skeletal deformities, growth retardation).
- Skeletal Malformations: Persistent bone weakness may lead to long-term issues.
- Increased Respiratory Morbidity: Weak ribs lead to a less stable chest wall, increasing work of breathing and exacerbating BPD.
- Prolonged Ventilator Dependence.
- Poor Weight Gain and Growth Failure: Due to pain and increased energy expenditure.
- Motor Developmental Delays: Fractures and pain restrict movement.
- Neurodevelopmental Impairment.
- Chronic Pain: Leading to irritability and sleep disturbances.
- Nephrocalcinosis/Nephrolithiasis: Risk of calcium deposits in kidneys if supplementation is not balanced.
- Electrolyte Imbalances.
- Reduced Peak Bone Mass: Potential for increased risk of osteoporosis later in life.


Have really liked the way the topic was fully explained and easy to understand.
Ya so simple mostly the mgt
Thanks so much this has really been helpful
J thank for the service,add prevention’s and complications
Precise and easy to understand…thanks so.much for the great work.
What are the possible complications?