Table of Contents
TogglePHARYNGITIS
Introduction
Pharyngitis is the inflammation of the mucous membranes of the pharynx. In most cases, the cause is an infection, either bacterial or viral. Other less common causes of pharyngitis include allergies, trauma, cancer, reflux, and certain toxins.
Types of Pharyngitis
Pharyngitis can be classified according to the duration i.e. as acute or chronic.
- Acute pharyngitis: has a sudden onset, and it resolves within less than 3 months. It may settle completely and recur in the future.
- Chronic pharyngitis: can last up to more than 3 months or having more than 5 episodes of tonsillitis in a year.
Classification of pharyngitis according to cause
- Infectious Pharyngitis: the cause is a pathogen e.g., commonly viruses, bacteria.
- Non-infectious pharyngitis: Caused by non-pathogens e.g., GERD.
Pathophysiology
Bacteria and viruses can cause direct invasion of the pharyngeal mucosa. Certain viruses like rhinovirus can cause irritation secondary to nasal secretions. In almost all cases, there is a local invasion of the pharyngeal mucosa which also results in excess secretion and edema. The inflammatory response leads to the characteristic symptoms of sore throat, redness, and swelling.
Causes of pharyngitis
- Viral causes: About 50% to 80% of pharyngitis, or sore throat, symptoms are viral in origin and include a variety of viral pathogens. These pathogens are predominantly rhinovirus, influenza, adenovirus, coronavirus, and parainfluenza. Less common viral pathogens include herpes simplex virus (HSV), Epstein-Barr virus (EBV) which causes infectious mononucleosis, human immunodeficiency virus (HIV), and coxsackievirus (causing Hand, Foot, and Mouth Disease). More severe cases tend to be bacterial and may develop after an initial viral infection.
- Bacterial causes: The most common bacterial infection is Group A beta-hemolytic streptococci (GAS), which causes 5% to 36% of cases of acute pharyngitis, particularly in children. Other bacterial etiologies include Group C and G streptococci, Chlamydia pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, Candida albicans (fungal infection, often in immunocompromised individuals), Neisseria meningitidis, Neisseria gonorrhoeae (gonococcal pharyngitis), Arcanobacterium haemolyticum, Fusobacterium necrophorum (associated with Lemierre's syndrome), and Corynebacterium diphtheriae (diphtheria, rare due to vaccination).
- Non-infectious causes: Environmental allergies and chemical exposures (e.g., smoke, pollutants, dry air), gastroesophageal reflux disease (GERD) where stomach acid irritates the throat, excessive voice use, and mouth breathing can also cause acute or chronic pharyngitis.
- Pharyngitis symptoms may also be part of the symptom complexes of other serious illnesses, including peritonsillar abscess, retropharyngeal abscess, epiglottitis (a life-threatening emergency), and Kawasaki disease (in children).
Clinical manifestations
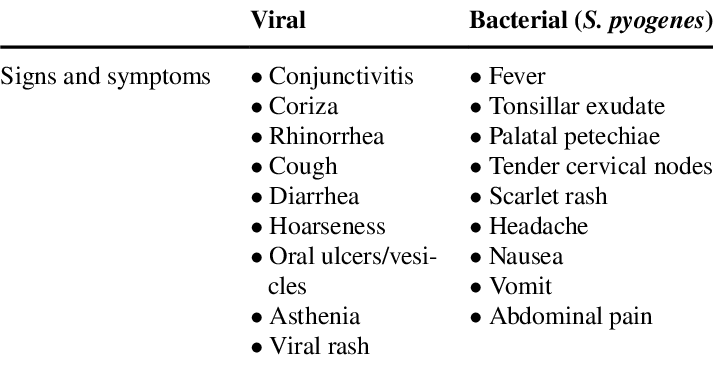
The signs and symptoms of pharyngitis can vary depending on the underlying cause, but common manifestations include:
- Sore throat/Throat pain: Often described as scratchy, burning, or painful, especially when swallowing.
- Dysphagia: Difficulty or pain when swallowing.
- Fever: Common, especially with bacterial or severe viral infections.
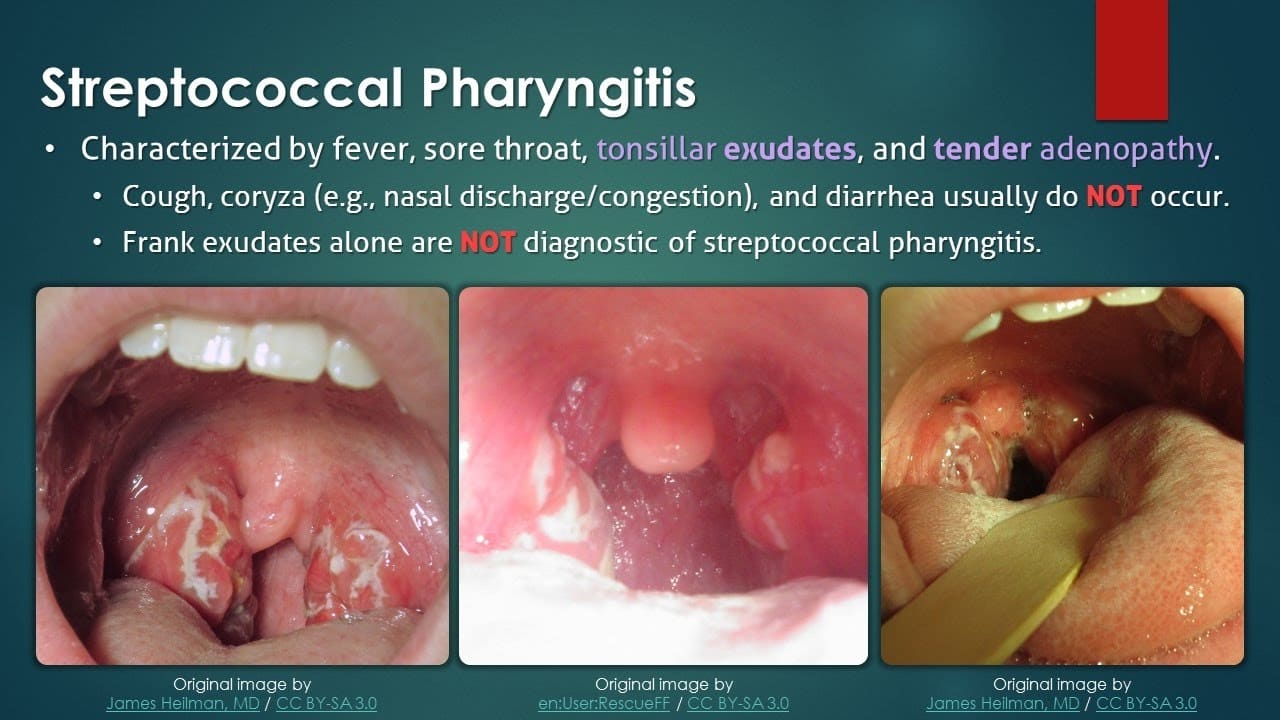
- Tonsillar exudates: White patches or streaks of pus on the tonsils (more common in bacterial infections like strep throat).
- Pharyngeal erythema: Redness and inflammation of the throat.
- Fatigue/Malaise: General feeling of being unwell.
- Nasal congestion and rhinorrhea: Runny nose, sneezing (more common in viral pharyngitis).
- Postnasal drip: Mucus dripping down the back of the throat, causing irritation and cough.
- Headache.
- Painful cervical adenopathy: Swollen and tender lymph nodes in the neck.
- Cough: Can be dry or productive.
- Myalgia and arthralgia: Muscle and joint aches (especially with viral infections like influenza).
- Ear pain: Referred pain from the throat.
- Rash: Can occur with certain infections, e.g., scarlatiniform rash with strep throat (scarlet fever), or maculopapular rash with infectious mononucleosis.
NB: Uncomplicated infectious pharyngitis, both viral and bacterial, typically is self-limited to 5 to 7 days, is not progressive, is bilateral, does not have trismus (difficulty opening the mouth), and does not have evidence of airway obstruction (stridor or severe difficulty breathing).
Diagnosis & Differential Diagnosis
Diagnosis
Diagnosis of pharyngitis typically involves a combination of clinical assessment and diagnostic tests.
- Inspection of the throat: Using a light source and tongue depressor to visualize the pharynx and tonsils for redness, swelling, exudates, ulcers, or vesicles.
- Palpation of the neck: To check for swollen and tender lymph nodes (cervical adenopathy).
- Examination of the ears and nose: To check for other possible sites of infection or signs of allergies.
- Skin examination: To check for any rashes (e.g., scarlatiniform rash of scarlet fever).
- Auscultation of lung and heart sounds: To rule out respiratory or cardiac involvement.
- Rapid Antigen Detection Test (RADT): A quick test performed in the clinic to detect Group A Streptococcus (GAS) bacteria. If positive, it suggests strep throat. If negative, a throat culture may still be performed, especially in children, to confirm.
- Throat culture: A sterile swab rubbed over the tonsils and posterior pharynx is sent to the lab to grow and identify bacteria. This is considered the gold standard for diagnosing strep throat.
- Molecular tests (PCR): Highly sensitive and specific tests that detect bacterial or viral DNA/RNA directly from a throat swab, providing rapid and accurate results for various pathogens.
- Complete Blood Count (CBC): May show elevated white blood cell count (leukocytosis) in bacterial infections, or atypical lymphocytes in viral infections like mononucleosis.
- Monospot test (Heterophile Antibody Test): Used to diagnose infectious mononucleosis, especially if EBV is suspected.
- Blood cultures: Rarely needed, but may be considered in severe cases or immunocompromised patients to rule out bloodstream infection.
Differential Diagnosis
It is important to differentiate pharyngitis from other conditions that can present with similar symptoms:
- Common cold: Usually presents with prominent nasal symptoms (runny nose, sneezing) and milder sore throat.
- Influenza: Characterized by abrupt onset of high fever, severe body aches, headache, fatigue, and respiratory symptoms including sore throat.
- Laryngitis: Primarily affects the voice box, leading to hoarseness or loss of voice, with less prominent throat pain.
- Tonsillitis: Often occurs with pharyngitis, but specifically refers to inflammation of the tonsils, which may be swollen, red, and have exudates.
- Allergic rhinitis: Chronic nasal congestion, sneezing, itching, and often clear nasal discharge, but typically without fever or significant throat pain unless due to postnasal drip.
- Gastroesophageal Reflux Disease (GERD): Can cause chronic sore throat, hoarseness, and a sensation of a lump in the throat, especially if untreated.
- Peritonsillar abscess: A collection of pus behind the tonsil, characterized by severe unilateral throat pain, trismus, muffled voice ("hot potato voice"), and deviation of the uvula. This is an emergency.
- Retropharyngeal abscess: A deep neck space infection, presenting with severe sore throat, fever, difficulty swallowing, stiff neck, and sometimes airway compromise. Also an emergency.
- Epiglottitis: Inflammation of the epiglottis, a life-threatening emergency, characterized by rapid onset of severe sore throat, dysphagia, drooling, muffled voice, and inspiratory stridor.
- Oral candidiasis (Thrush): Fungal infection causing white patches on the tongue and oral mucosa, which can extend to the throat, often seen in immunocompromised individuals.
- Sexually transmitted infections (STIs): Gonococcal pharyngitis or primary HIV infection can present with sore throat.
- Kawasaki disease: A rare childhood illness causing inflammation of blood vessels, with symptoms including fever, rash, conjunctivitis, swollen lymph nodes, and red throat.
Management
Treatment goals:
- Relieve symptoms (pain, fever).
- Eradicate infection (if bacterial).
- Prevent complications.
Medical Management
Treatment of pharyngitis is largely supportive for viral cases and focuses on maintaining adequate hydration and caloric intake and controlling pain and fever. For bacterial cases, antibiotics are crucial.
- Hydration: Maintaining adequate oral fluid intake is essential to prevent dehydration, especially with fever and difficulty swallowing. If oral intake is insufficient, intravenous (IV) hydration may be necessary.
- Diet: Soft, easily swallowed foods and cool liquids are often preferred. Avoid irritating foods (acidic, spicy).
- Rest: Adequate rest is important for recovery, especially for children.
- Pharmacologic Management:
- Antibiotics: Prescribed only for bacterial pharyngitis, most commonly for Group A Streptococcus. Penicillin or amoxicillin are first-line agents. For penicillin-allergic patients, azithromycin, cephalexin, or clindamycin may be used. The full course of antibiotics must be completed to prevent complications like rheumatic fever.
- Analgesics and Antipyretics:
- Acetaminophen (paracetamol): For pain and fever relief.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): (e.g., ibuprofen, naproxen) also reduce pain and inflammation.
- Topical Anesthetics: Throat lozenges, sprays (e.g., benzocaine, phenol), or gargles can provide temporary local pain relief.
- Corticosteroids: (e.g., dexamethasone) may be administered in severe cases of pharyngitis (e.g., with significant swelling or in infectious mononucleosis) to reduce inflammation, improve swallowing, and potentially reduce pain.
- Antivirals: Rarely used for viral pharyngitis, except in specific cases like severe influenza (oseltamivir) or herpes simplex virus (acyclovir).
Nursing interventions/management
1. Assessment of the patients
- a. Carrying out a comprehensive history of the presenting signs and symptoms (e.g., fever, ear pain, sore throat, difficulty swallowing, cough, nasal discharge, rash, muscle aches, exposure history).
- b. Taking vital observations (e.g., Temperature, Pulse, Respirations, Blood Pressure) and performing a general physical examination to assess the patient's overall condition and to exclude other serious conditions (e.g., signs of airway compromise, severe dehydration).
- c. Alerting the doctor if signs of severe infection or complications are present, for further investigations and management. The nurse will assist the patient throughout this process.
2. Managing fever
- a. Assess the patient’s vital signs, especially temperature, at least every 4 hours, and more frequently if fever is high.
- b. Remove excessive clothing and blankets. Adjust the room temperature to a comfortable level.
- c. Administer prescribed antipyretics (e.g., acetaminophen, ibuprofen) as ordered.
- d. Offer a tepid sponge bath or cool compresses to the forehead and axillae, if tolerated and effective.
- e. Encourage increased fluid intake to prevent dehydration associated with fever.
- f. Encourage rest.
3. To relieve pain and discomfort
- a. Assess the patient’s pain level using a pain scale and characteristics of pain (location, quality, duration) before and at least 30 minutes after administration of medication to evaluate effectiveness.
- b. Administer prescribed analgesics (e.g., acetaminophen, NSAIDs).
- c. Encourage warm or cool liquids (e.g., warm tea with honey, cold water, popsicles) as preferred by the patient to soothe the throat.
- d. Offer throat lozenges or sprays as ordered or as appropriate.
- e. Encourage gargling with warm salt water several times a day to reduce inflammation and discomfort.
- f. Advise the patient to minimize talking or rest the voice to reduce strain on the throat.
- g. Encourage the patient to verbalize feelings of pain and discomfort.
- h. Elevate the head of the bed or position the patient in semi-Fowler’s to promote comfort and ease breathing.
4. Prevention of complications
- a. Continuously assess the patient’s vital signs and respiratory status (rate, depth, effort, presence of stridor, retractions, oxygen saturation) at least every 4 hours, and more frequently if signs of respiratory distress are noted. Assess for signs of hypoxia (e.g., restlessness, cyanosis).
- b. Monitor for signs of worsening infection or development of complications (e.g., peritonsillar abscess: severe unilateral pain, trismus, muffled voice; rheumatic fever: joint pain, rash, cardiac murmurs; glomerulonephritis: dark urine, swelling).
- c. Ensure completion of the full course of antibiotics for bacterial pharyngitis to prevent complications like acute rheumatic fever and post-streptococcal glomerulonephritis.
- d. Position the patient in a side-lying or prone position if secretions are excessive to prevent aspiration, or elevate the head of the bed.
- e. Suction oral secretions as needed to maintain airway patency.
- f. Advise cessation of smoking or avoiding exposure to secondhand smoke, and minimizing alcohol intake, as these can irritate the throat and impede healing.
- g. Administer prescribed medications (e.g., corticosteroids to reduce swelling, antibiotics for bacterial infections).
5. To prevent infection and to promote good nutrition
- a. Assess vital signs and observe for any signs of worsening infection or secondary infections.
- b. Perform a focused assessment on the oropharyngeal region, particularly checking for any collection of abscess or spreading inflammation.
- c. Teach the patient and family how to perform proper hand hygiene to prevent the spread of infection.
- d. Encourage the patient to take a lot of warm fluids (at least 2-3 liters a day, unless contraindicated) to thin secretions and prevent dehydration.
- e. Encourage the patient to consume soft, easy-to-swallow foods rich in vitamins and nutrients to support the immune system. Avoid foods that may irritate the throat (e.g., very hot, cold, spicy, acidic, crunchy foods).
- f. Administer antibiotics as prescribed and ensure adherence.
6. To relieve the patient’s anxiety and Health educate the patient
- a. Reassure the patient and family, providing clear and honest information about the condition and treatment plan.
- b. Assess the patient’s fears and concerns, and provide emotional support and counselling as needed.
- c. Health educate the patient and family about the disease process, its causes, modes of transmission, and expected course.
- d. Teach the patient and family about proper hand hygiene, cough etiquette, and avoiding close contact with others to prevent the spread of infection.
- e. Explain the importance of completing the full course of antibiotics and the signs of complications that require immediate medical attention.
7. Advice on discharge
- a. Encourage the patient to maintain good hydration by taking plenty of warm fluids.
- b. Emphasize the importance of adhering to prescribed medications, especially completing the full course of antibiotics.
- c. Advise on when to return for follow-up appointments with the healthcare provider.
- d. Educate on lifestyle modifications, such as avoiding irritants (smoking, pollutants), managing underlying conditions like GERD or allergies.
- e. Provide clear instructions on warning signs or symptoms that necessitate seeking immediate medical attention (e.g., difficulty breathing, severe worsening pain, persistent high fever, rash, swelling, inability to swallow).
Complications
If left untreated or inadequately managed, pharyngitis, especially bacterial pharyngitis caused by Group A Streptococcus, can lead to several complications:
- Peritonsillar abscess (Quinsy): A collection of pus behind the tonsil, requiring drainage.
- Retropharyngeal abscess: A deep neck space infection behind the pharynx, a life-threatening emergency.
- Epiglottitis: Inflammation of the epiglottis, which can rapidly lead to airway obstruction.
- Cervical lymphadenitis: Inflammation and enlargement of neck lymph nodes.
- Otitis media: Middle ear infection.
- Sinusitis: Inflammation of the sinuses.
- Mastoiditis: Infection of the mastoid bone behind the ear (rare).
- Acute Rheumatic Fever (ARF): A serious inflammatory disease that can affect the heart (rheumatic heart disease), joints, brain, and skin. It is a preventable complication with appropriate antibiotic treatment of strep throat.
- Post-streptococcal Glomerulonephritis (PSGN): A kidney disorder that can develop after a strep infection, characterized by inflammation of the kidney's filtering units.
- Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS): A controversial condition where strep infections are thought to trigger or exacerbate certain neuropsychiatric disorders in children (e.g., OCD, Tourette's syndrome).


