Table of Contents
ToggleSINUSITIS/RHINOSINUSITIS
Introduction
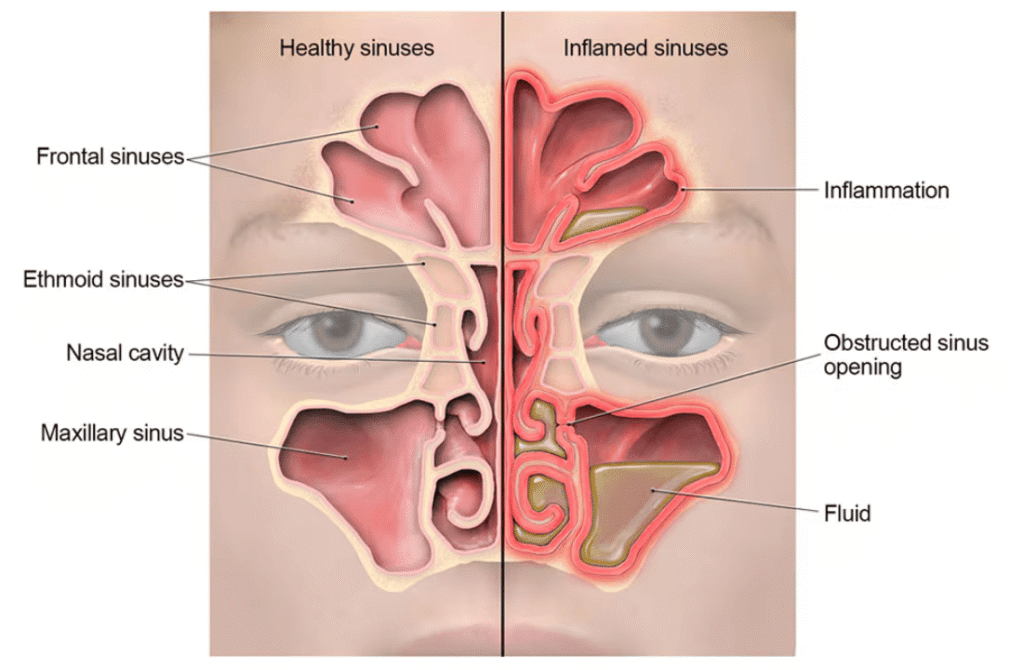
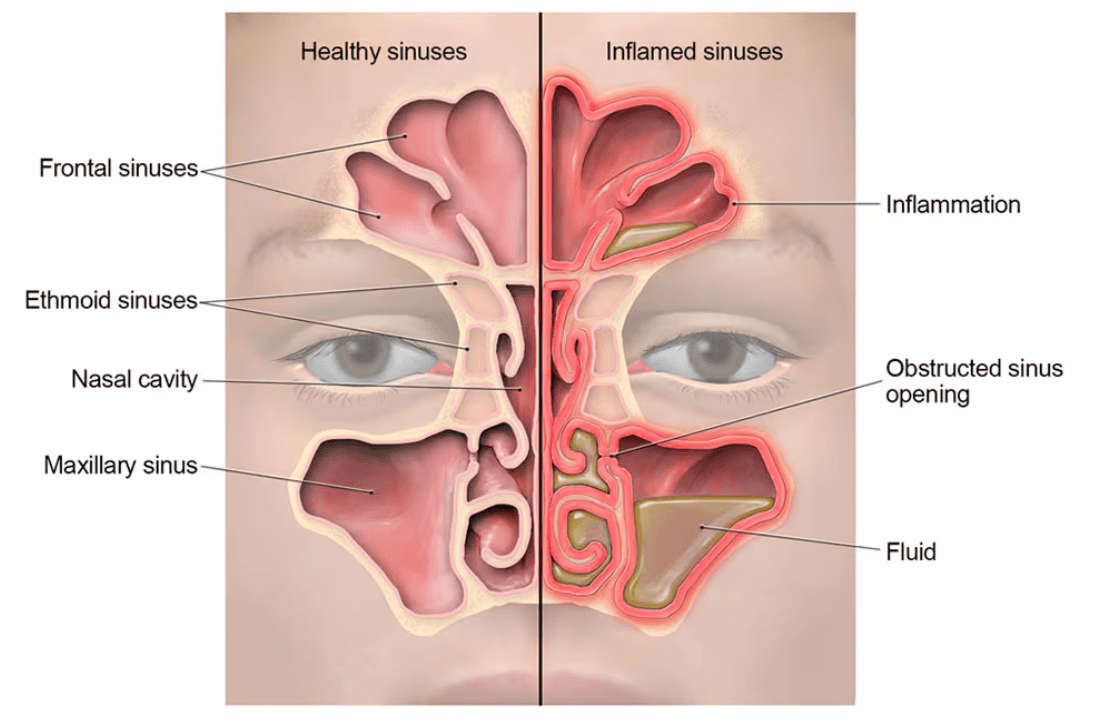
Sinusitis is the inflammation and swelling of the lining of the sinuses, which blocks the openings into the nose, prevents normal drainage and creates a breeding ground for further infection. Possible causes are a viral, bacterial or fungal infection, or an allergy. This condition is currently known as Rhinosinusitis. It's the inflammation of the paranasal sinuses and the nasal cavity. It is recommended to use the word rhinosinusitis because usually sinusitis is accompanied by inflammation of the nasal mucosa.
Types of sinusitis
CLASSIFICATION (according to duration) of symptoms:
- Acute sinusitis: is diagnosed when symptoms last up to four weeks (Brook et al, 2000). It often develops from a common cold or allergic rhinitis.
- Sub-acute (or relapsing) sinusitis: is diagnosed when symptoms persist or recur after four weeks, but for less than three months.
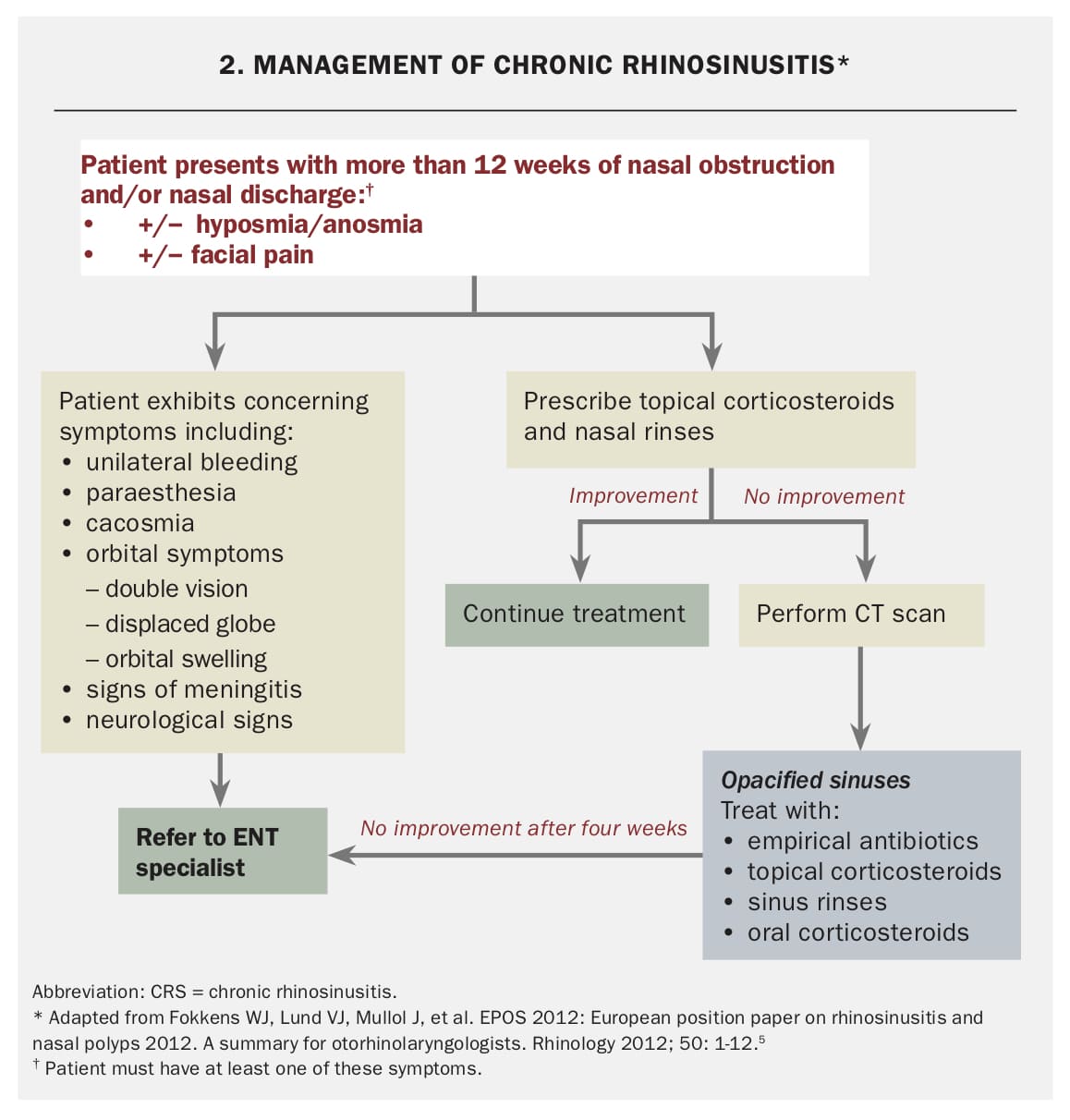
- Chronic sinusitis: is diagnosed when symptoms persist for more than three months. It is also diagnosed when people have more than three or four significant episodes annually, or repeatedly fail to respond to medical treatment. Chronic sinusitis can be further classified into chronic sinusitis with nasal polyps (CRSwNP) and chronic sinusitis without nasal polyps (CRSsNP).
- Recurrent acute rhinosinusitis: Characterized by four or more episodes of acute rhinosinusitis per year, with complete resolution of symptoms between episodes.
Pathophysiology
Most commonly a viral upper respiratory infection causes sinusitis secondary to edema and inflammation of the nasal lining and production of thick mucus that obstructs the paranasal sinuses and allows a secondary bacterial overgrowth. There are frontal, maxillary, sphenoid, and ethmoid sinuses. Allergic rhinitis can lead to sinusitis also due to ostial obstruction. Ciliary immobility can lead to increased mucus viscosity, further blocking drainage. Bacteria are introduced into the sinuses by coughing and nose blowing. Bacterial sinusitis usually occurs after a viral upper respiratory infection and worsening symptoms after 5 days, or persistent symptoms after 10 days. The impaired mucociliary clearance and obstruction of the ostia (openings of the sinuses) are key factors in the development of sinusitis. This creates an environment conducive to bacterial or fungal proliferation.
Causes of sinusitis
- Bacterial: Common causative organisms include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Less commonly, Staphylococcus aureus and anaerobic bacteria may be involved, especially in chronic cases.
- Viral: Rhinovirus, influenza virus, parainfluenza virus, adenovirus, and respiratory syncytial virus are common viral culprits, often preceding bacterial infections.
- Fungal: Fungal sinusitis is less common but can be severe, especially in immunocompromised individuals. It can be invasive (e.g., mucormycosis, aspergillosis) or non-invasive (e.g., fungal ball, allergic fungal rhinosinusitis).
- Allergic: Allergic reactions can lead to inflammation and swelling of the nasal and sinus lining, obstructing drainage and predisposing to infection.
- Environmental irritants: Exposure to pollutants, smoke, and chemical irritants can irritate the sinus lining and contribute to inflammation.
Risk factors for sinusitis
These include any condition that interferes with proper drainage and ventilation of the sinuses due to stasis of secretion and mucosal swelling e.g.
- Deviated nasal septum: A displacement of the wall that divides the nostrils, impeding drainage.
- Nasal polyps: Benign growths in the nasal passages or sinuses that can obstruct airflow and drainage.
- Adenoid hypertrophy: Enlarged adenoids, especially in children, can block the Eustachian tubes and contribute to sinus issues.
- Turbinate hypertrophy: Enlarged turbinates (structures inside the nose) can obstruct drainage.
CLINICAL MANIFESTATION
Symptoms can vary depending on the affected sinus and the severity of the inflammation.
- Facial pain and pressure: Often described as a dull, throbbing pain or pressure over the affected sinus (e.g., forehead for frontal, cheeks/upper teeth for maxillary, behind eyes for ethmoid/sphenoid). Pain worsens when bending forward, straining, or coughing.
- Nasal congestion/blockage: Difficulty breathing through the nose due to swollen nasal passages.
- Purulent nasal discharge (rhinorrhea): Thick, discolored (yellowish, greenish) discharge from the nose, which may be offensive in bacterial cases. Postnasal drip can also occur, leading to throat irritation and cough.
- Headache: Continuous frontal throbbing headache is common, especially with frontal sinusitis.
- Cough: Often worse at night due to postnasal drip.
- Fever: More common in acute bacterial sinusitis.
- Fatigue and malaise: General feeling of unwellness.
- Halitosis (bad breath): Due to bacterial overgrowth and drainage.
- Decreased sense of smell (hyposmia) or complete loss of smell (anosmia): Due to inflammation affecting the olfactory receptors.
- Ear pain or pressure: Can occur due to Eustachian tube dysfunction.
- Sore throat: From postnasal drip.
- Dental pain: Maxillary sinusitis can mimic toothache.
- Tenderness to palpation: Over the affected sinus areas.
NB: Bending and coughing or straining increases the pain. It can be confused with a lot of conditions like migraine, trigeminal neurological disorder or cranial arteritis.
DIAGNOSIS & DIFFERENTIAL DIAGNOSIS
DIAGNOSIS
Diagnosis of sinusitis involves a combination of clinical assessment and diagnostic tests.
- History taking: Detailed information about symptoms, their duration, severity, and associated factors.
- Physical examination:
- Anterior rhinoscopy: Examination of the nasal passages using a speculum to visualize inflammation, discharge, and any structural abnormalities.
- Palpation: Tenderness to palpation over the frontal and maxillary sinuses.
- Transillumination: Shining a light through the sinuses to check for opacity (cloudiness), though this is less reliable than imaging.
- Pharyngeal examination: To assess for postnasal drip.
- Plain sinus X-rays: May show mucosal thickening, air-fluid levels, or opacification (cloudiness) of the sinuses, but less sensitive than CT.
- Computed Tomography (CT) scan of the sinuses: The gold standard for diagnosing sinusitis, providing detailed images of bony and soft tissue structures, demonstrating mucosal thickening, fluid levels, polyps, and anatomical variations. It helps in planning surgical interventions.
- Magnetic Resonance Imaging (MRI): Useful for differentiating between inflammatory fluid, tumors, and fungal infections, especially when intracranial complications are suspected.
- Nasal endoscopy: A thin, flexible or rigid endoscope is inserted into the nose to directly visualize the nasal passages and sinus openings, assess for inflammation, polyps, and discharge, and obtain samples for culture.
- Nasal or throat swab: Less reliable for diagnosing bacterial sinusitis as it may reflect colonization rather than true infection.
- Sinus culture: Obtained directly from the sinus cavity (e.g., during endoscopy or aspiration) is the most accurate way to identify causative bacteria or fungi and determine antibiotic susceptibility.
- Complete Blood Count (CBC): May show an elevated white blood cell count in bacterial infections, but often non-specific.
- Inflammatory markers: Elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may indicate inflammation but are not specific to sinusitis.
Differential diagnosis
It is important to differentiate sinusitis from other conditions that present with similar symptoms:
- Common cold: Usually self-limiting with symptoms resolving within 7-10 days, without significant facial pain or purulent discharge.
- Allergic rhinitis: Characterized by sneezing, itching, watery eyes, clear nasal discharge, and often triggered by allergens. No fever or purulent discharge.
- Migraine or other headaches: Can cause severe head pain, but usually lack nasal symptoms, fever, or purulent discharge.
- Trigeminal neuralgia: Causes severe, sharp facial pain, but typically without nasal symptoms or signs of infection.
- Cranial arteritis (Giant cell arteritis): Inflammatory condition affecting arteries, causing headache and scalp tenderness, but usually in older adults and without typical sinus symptoms.
- Dental infections: Can cause pain in the upper jaw, mimicking maxillary sinusitis. Dental examination can differentiate.
- Nasal polyps: Can cause nasal obstruction and decreased sense of smell, but may not always be associated with acute inflammatory signs.
- Adenoids (especially in children): Enlarged adenoids can cause nasal obstruction and mouth breathing, leading to recurrent sinus infections.
- Foreign body in the nose: Especially in children, can cause unilateral foul-smelling nasal discharge.
- Temporomandibular joint (TMJ) dysfunction: Can cause facial pain around the jaw and ear.
Management
Treatment goals:
- Relieve symptoms (pain, congestion).
- Eradicate infection (if bacterial or fungal).
- Restore normal sinus drainage and ventilation.
- Prevent complications and recurrence.
Pharmacological Management:
- Antibiotics: For bacterial sinusitis, a course of antibiotics is typically prescribed. Common choices include Amoxicillin, Amoxicillin-clavulanate (co-amoxiclav), Doxycycline, or Fluoroquinolones (e.g., Levofloxacin, Moxifloxacin) for penicillin-allergic patients or resistant cases. The duration of treatment varies but is often 10-14 days for acute cases.
- Nasal Decongestants:
- Topical decongestants: (e.g., oxymetazoline, xylometazoline) can provide rapid relief of nasal congestion by constricting blood vessels. Use should be limited to 3-5 days to prevent rebound congestion (rhinitis medicamentosa).
- Oral decongestants: (e.g., pseudoephedrine, phenylephrine) can also reduce congestion, but may have systemic side effects like increased heart rate and blood pressure.
- Corticosteroids:
- Topical intranasal corticosteroids: (e.g., fluticasone propionate, mometasone furoate, budesonide) are highly effective in reducing mucosal inflammation and swelling, improving sinus drainage. They are a cornerstone of treatment for both acute and chronic rhinosinusitis, and particularly useful in allergic rhinitis.
- Oral corticosteroids: (e.g., prednisone) may be prescribed for severe cases of acute sinusitis or chronic sinusitis with significant inflammation or polyps, for a short course to reduce inflammation rapidly.
- Mucolytics: (e.g., guaifenesin) can help thin mucus, making it easier to drain.
- Antihistamines: May be used if allergic rhinitis is a contributing factor, but generally not recommended for non-allergic sinusitis as they can dry out nasal secretions.
- Pain relievers: Over-the-counter analgesics like acetaminophen (paracetamol) or NSAIDs (e.g., ibuprofen, naproxen) can manage pain and fever.
Non-Pharmacological and Supportive Measures:
- Nasal saline irrigation: Using a neti pot or saline spray to rinse nasal passages helps clear mucus, irritants, and allergens, and can reduce inflammation. This is highly recommended for both acute and chronic sinusitis.
- Steam inhalation: Inhaling steam from a bowl of hot water or a shower can help moisten nasal passages and loosen mucus.
- Warm compresses: Applying warm, moist towels to the face (over the affected sinuses) can help relieve pain and promote drainage.
- Adequate hydration: Drinking plenty of fluids (water, clear broths) helps thin mucus.
- Rest: Important for recovery, especially during acute phases.
- Humidifier: Using a humidifier in the bedroom can keep nasal passages moist.
- Avoid irritants: Steer clear of smoke, strong odors, and allergens that can worsen symptoms.
Surgical Management:
- Functional Endoscopic Sinus Surgery (FESS): This is the most common surgical procedure for chronic sinusitis that does not respond to medical treatment, or in cases of recurrent acute sinusitis, or complications. FESS aims to restore natural drainage pathways by removing obstructions (e.g., polyps, diseased tissue, bone) and enlarging sinus openings, while preserving healthy tissue.
- Balloon Sinuplasty: A less invasive procedure where a balloon catheter is used to dilate the sinus openings.
- Septoplasty: Surgical correction of a deviated nasal septum if it is contributing significantly to obstruction.
- Polypectomy: Surgical removal of nasal polyps.
Complication of sinusitis
If left untreated or inadequately managed, sinusitis can lead to several complications, some of which can be serious:
- Periorbital cellulitis: Infection of the soft tissues around the eye.
- Orbital cellulitis: More serious infection involving the tissues within the orbit, potentially leading to vision loss or blindness.
- Orbital abscess: Collection of pus within the orbit.
- Meningitis: Inflammation of the membranes surrounding the brain and spinal cord.
- Brain abscess: Collection of pus within the brain tissue.
- Epidural or subdural abscess: Collections of pus between the dura mater and the skull, or between the dura and arachnoid membranes, respectively.
- Cavernous sinus thrombosis: Formation of a blood clot in the cavernous sinus, a large venous channel at the base of the brain, which can lead to severe neurological deficits or death.
- Osteomyelitis: Infection of the bone (e.g., frontal bone osteomyelitis, also known as Pott's puffy tumor if associated with a swelling on the forehead).
Nursing Interventions for Sinusitis/Rhinosinusitis
Nursing care for patients with sinusitis focuses on symptom management, promoting drainage, preventing complications, and patient education.
1. Assessment:
- Gather comprehensive history:
- Onset, duration, and characteristics of symptoms (pain, discharge, congestion, fever, cough).
- Aggravating and alleviating factors.
- Presence of allergies, asthma, or other respiratory conditions.
- Previous episodes of sinusitis or respiratory infections.
- Medications being taken (prescription and over-the-counter).
- Risk factors (smoking, exposure to irritants, immune status).
- Perform thorough physical assessment:
- Assess vital signs (temperature, pulse, respiration, blood pressure).
- Inspect nasal mucosa for swelling, redness, and character of discharge.
- Palpate over sinus areas for tenderness.
- Assess for facial swelling or redness.
- Auscultate lung sounds to identify any signs of lower respiratory involvement.
- Assess sense of smell.
- Evaluate pain: Use a pain scale to assess severity, location, and quality of pain.
- Monitor for complications: Observe for signs of orbital or intracranial complications (e.g., changes in vision, eye swelling, severe headache, altered mental status, stiff neck).
2. Symptom Management:
- Pain management:
- Administer prescribed analgesics (acetaminophen, NSAIDs) as ordered.
- Educate patient on proper use of over-the-counter pain relievers.
- Encourage warm compresses to the face to reduce pain and discomfort.
- Promote sinus drainage and reduce congestion:
- Instruct and assist with nasal saline irrigation (e.g., neti pot, saline sprays) several times a day. Emphasize using distilled, sterile, or previously boiled and cooled water.
- Encourage steam inhalation (e.g., warm shower, humidifier, bowl of hot water with towel over head) for 10-15 minutes, several times a day.
- Administer prescribed nasal decongestants and corticosteroids, educating on proper technique and limiting use of topical decongestants.
- Encourage increased fluid intake (water, juices, clear broths) to thin secretions and prevent dehydration.
- Advise elevation of the head of the bed to promote drainage.
- Fever reduction: Administer antipyretics as ordered.
- Cough management: Encourage increased fluid intake and possibly cough suppressants if cough is disruptive.
3. Medication Administration and Education:
- Administer antibiotics as prescribed, ensuring completion of the full course even if symptoms improve, to prevent recurrence and antibiotic resistance. Educate on potential side effects.
- Educate on the correct use of nasal sprays (corticosteroids, decongestants), emphasizing proper head position and avoiding swallowing.
- Explain the purpose and potential side effects of all prescribed medications.
4. Patient Education:
- Disease process: Explain what sinusitis is, its causes, and expected course.
- Importance of adherence: Emphasize the importance of completing the full course of antibiotics and consistently using other prescribed medications.
- Self-care measures: Reinforce nasal saline irrigation, steam inhalation, hydration, and rest.
- Prevention strategies:
- Avoid irritants (smoke, allergens, strong chemicals).
- Practice good hand hygiene.
- Avoid close contact with sick individuals.
- Manage underlying conditions like allergies effectively.
- Consider humidifier use, especially in dry environments.
- Warning signs: Educate on signs and symptoms that warrant immediate medical attention (e.g., worsening pain, high fever, vision changes, severe headache, swelling around the eyes, stiff neck, altered mental status).
- Follow-up care: Explain the importance of follow-up appointments with the healthcare provider.
5. Promote Rest and Comfort:
- Encourage adequate rest to facilitate recovery.
- Provide a quiet and comfortable environment.
6. Nutritional Support:
- Encourage a balanced diet to support the immune system.
- Ensure adequate fluid intake.
7. Pre- and Post-operative Care (if surgery is indicated):
- Pre-operative:
- Provide clear explanations of the surgical procedure (e.g., FESS), expected outcomes, and potential risks.
- Educate on pre-operative instructions (e.g., NPO status, medication adjustments).
- Address patient anxieties and concerns.
- Post-operative:
- Monitor vital signs, level of consciousness, and pain.
- Assess for nasal bleeding or excessive drainage.
- Provide pain management.
- Educate on post-operative care: nasal packing care (if applicable), nasal saline rinses, activity restrictions, avoiding nose blowing, and signs of complications.
- Emphasize follow-up appointments for nasal endoscopy and cleaning.