The Respiratory System
Learning Objectives
Upon completion of this lecture, students will be able to:
- Identify the organs of the upper and lower respiratory tracts.
- Describe the detailed anatomy of the nasal cavity, pharynx, larynx, trachea, bronchial tree, and lungs.
- List and explain the multiple functions of the respiratory system, including gas exchange, air conditioning, and sound production.
- Explain the process of pulmonary ventilation (breathing), including the roles of the respiratory muscles.
- Define and differentiate between the various lung volumes and capacities.
- Describe the mechanisms of external and internal respiration, explaining the role of partial pressure gradients.
- Outline how oxygen and carbon dioxide are transported in the bloodstream.
- Explain the neural and chemical mechanisms that control the rate and depth of breathing.
- Identify common deviations from the normal structure and function of the respiratory system.
Introduction to the Respiratory System
The respiratory system is a group of organs and tissues responsible for breathing. Its primary role is to provide a continuous supply of oxygen from the atmospheric air to the body's cells and to remove the waste product, carbon dioxide. This process is essential for cellular respiration, the metabolic process that generates ATP (energy) for all cellular activities.
The respiratory system is responsible for breathing (moving air in and out of the lungs) and exchanging gases (oxygen and carbon dioxide).
Function: To bring oxygen from the air into the body and remove carbon dioxide from the body. This gas exchange happens at the lungs and in the body tissues.
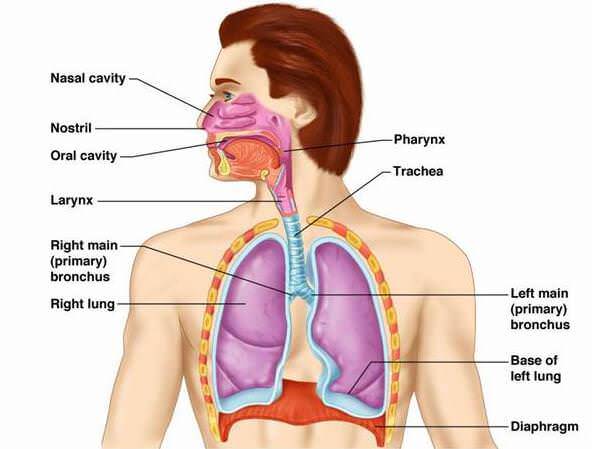
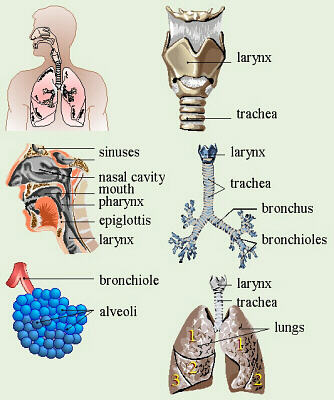
Main Parts: The system includes the passages that carry air and the organs where gas exchange takes place:
- The air passages (nose, pharynx, larynx, trachea, bronchi, bronchioles) – these are like the tubes air travels through.
- The lungs – where the important gas exchange happens.
- The pleura – the membranes covering the lungs.
- The muscles of breathing (diaphragm and intercostal muscles) – which help move air in and out.
Air Conditioning: The air we breathe from the environment can be cold, dry, dirty, or have different temperatures. As air travels through the air passages to the lungs, it is warmed or cooled to body temperature, moistened (saturated with water vapour), and filtered (cleaned) of dust, microbes, and other particles. This prepares the air before it reaches the delicate lungs.
Key Processes of Respiration:
The overall process of respiration involves four distinct events:
- Pulmonary Ventilation (Breathing): The mechanical process of moving air into and out of the lungs.
- External Respiration: The exchange of gases (oxygen and carbon dioxide) between the air in the alveoli of the lungs and the blood in the pulmonary capillaries.
- Transport of Respiratory Gases: The cardiovascular system transports oxygen from the lungs to the body tissues and carbon dioxide from the tissues back to the lungs.
- Internal Respiration: The exchange of gases between the blood in the systemic capillaries and the body's tissue cells.
Anatomy of the Respiratory System
The organs of the respiratory system are commonly divided into two tracts:
- Upper Respiratory Tract: Includes the nose, nasal cavity, pharynx, and associated structures.
- Lower Respiratory Tract: Includes the larynx, trachea, bronchi, and lungs.
The Nose and Nasal Cavity
The nose is the main route for air entry into the respiratory system.
Location: The nose is on the face, and the nasal cavity is a large space behind the nose, divided into two sides by a wall called the septum.
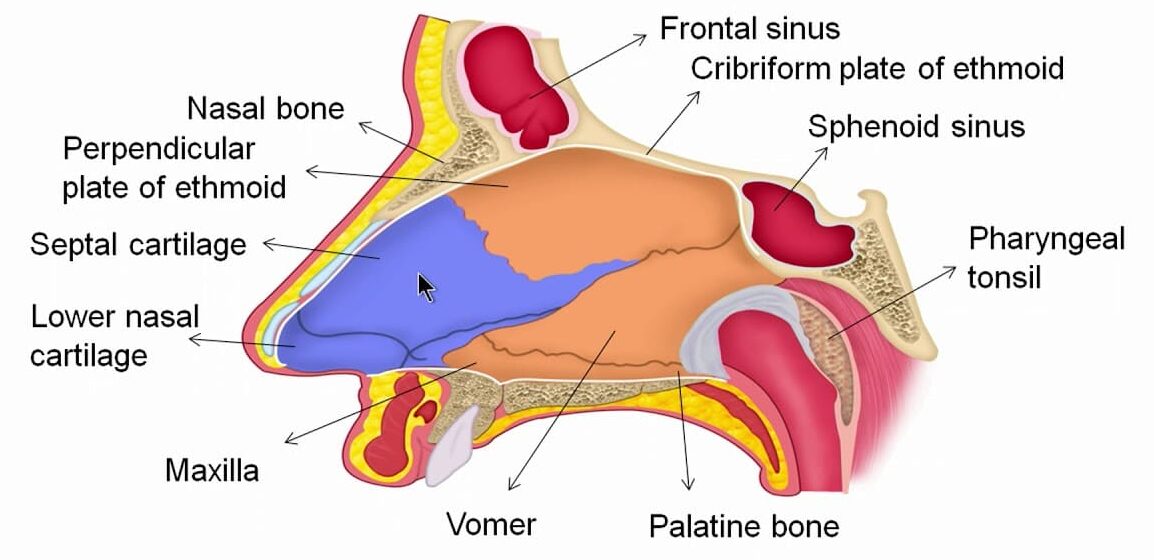
Structure: The nasal cavity is a large, irregular space divided into two equal passages by the nasal septum.
- Septum: The anterior part is made of hyaline cartilage, while the posterior bony part is formed by the vomer and the perpendicular plate of the ethmoid bone.
- Roof: Formed by the cribriform plate of the ethmoid bone and parts of the sphenoid, frontal, and nasal bones.
- Floor: Formed by the hard palate (composed of the maxilla and palatine bones) and the muscular soft palate.
- Walls: The lateral walls are formed by the maxilla, ethmoid bone, and the inferior nasal conchae. The medial wall is the septum.
- Conchae (or Turbinates): Three bony projections (superior, middle, and inferior) on each lateral wall that greatly increase the surface area and create turbulence in the inhaled air.
Functions of the Nose and Nasal Cavity:
- Warming: The nasal cavity is lined with a mucous membrane that has an immense blood supply (high vascularity). As air flows past, it is rapidly warmed. This high vascularity is also why nosebleeds (epistaxis) can result in significant blood loss.
- Filtering and Cleaning: Coarse hairs in the nostrils (anterior nares) trap larger particles. Smaller particles like dust and bacteria are trapped in the sticky mucus.
- Humidification: As air travels over the moist mucosal surface, it becomes saturated with water vapor, preventing the delicate lung tissues from drying out.
- Olfaction (Sense of Smell): The roof of the nasal cavity contains the olfactory epithelium, where receptors for the sense of smell are located.
- Protective Reflex: Irritation of the nasal mucosa triggers the sneeze reflex, a forceful expulsion of air to clear the passages of irritants.
- Passageway for air: Air enters through the nostrils (anterior nares) and passes through the nasal cavity to the back of the throat (pharynx).
The Pharynx (Throat)
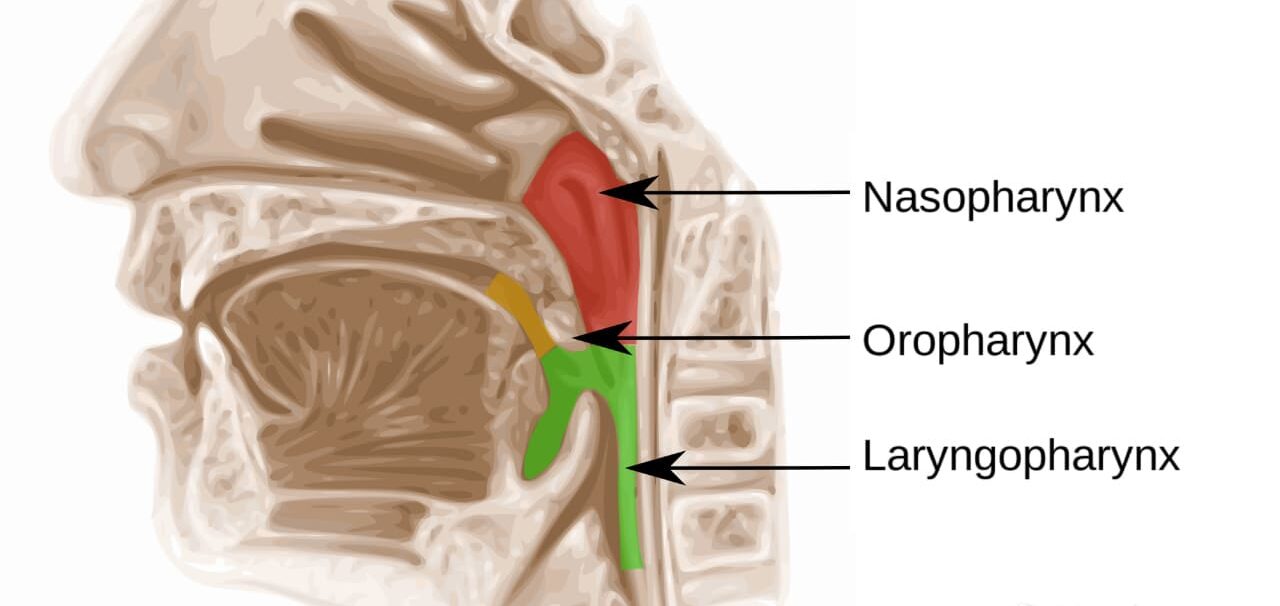
The pharynx is a muscular tube, approximately 12-14 cm long, that serves as a passageway for both air and food. It extends from the base of the skull to the level of the 6th cervical vertebra.
Location: The tube at the back of the mouth and nasal cavity, extending down to the oesophagus and larynx.
Structure: Divided into three parts (nasopharynx, oropharynx, laryngopharynx). It has a lining that changes from ciliated (in the nasopharynx, continuous with the nose) to stratified squamous epithelium (in the oropharynx and laryngopharynx, continuous with the mouth) for protection from food. It contains muscle in its walls.
Divisions of the Pharynx:
- Nasopharynx: The superior portion, located directly behind the nasal cavity. It is an air-only passageway. The pharyngeal tonsils (adenoids) and the openings of the auditory (Eustachian) tubes are located here.
- Oropharynx: The middle portion, located behind the oral cavity. It is a common passageway for both food and air. The palatine tonsils are found on its lateral walls.
- Laryngopharynx: The inferior portion, extending from the epiglottis to the larynx. It is also a common passageway for food and air, and it is where the respiratory and digestive pathways diverge.
Functions of the Pharynx:
- Passageway for Air and Food: Directs air towards the larynx and food towards the esophagus.
- Warming and Humidifying: Continues the process started in the nasal cavity.
- Hearing: The auditory tubes open into the nasopharynx, allowing pressure to be equalized between the middle ear and the atmosphere, which is crucial for protecting the eardrum.
- Protection: The tonsils (lymphoid tissue) provide immune surveillance against inhaled or ingested pathogens.
- Speech: The pharynx acts as a resonating chamber, helping to give the voice its unique characteristics.
The Larynx (Voice Box)
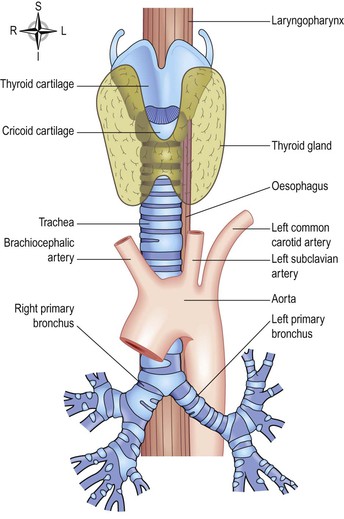
The larynx is a complex cartilaginous structure that connects the pharynx to the trachea.
Location: Situated at the top of the trachea, in front of the pharynx.
Structure: Made up of several irregularly shaped cartilages joined by ligaments and membranes. The main cartilages are the thyroid cartilage (forms the Adam's apple, more prominent in males), cricoid cartilage, and arytenoid cartilages. A leaf-shaped cartilage called the epiglottis sits at the top. The inside is lined with ciliated columnar epithelium (except on the vocal cords).
- Thyroid Cartilage: The largest cartilage, made of hyaline cartilage. Its anterior projection forms the laryngeal prominence, commonly known as the Adam's apple, which is more prominent in males after puberty.
- Cricoid Cartilage: A ring-shaped hyaline cartilage located below the thyroid cartilage. It is the only complete ring of cartilage in the airway.
- Arytenoid Cartilages: Paired, pyramid-shaped hyaline cartilages that anchor the vocal cords.
- Epiglottis: A leaf-shaped elastic cartilage. During swallowing, the larynx moves superiorly, and the epiglottis tips down to cover the laryngeal opening, preventing food and drink from entering the trachea.
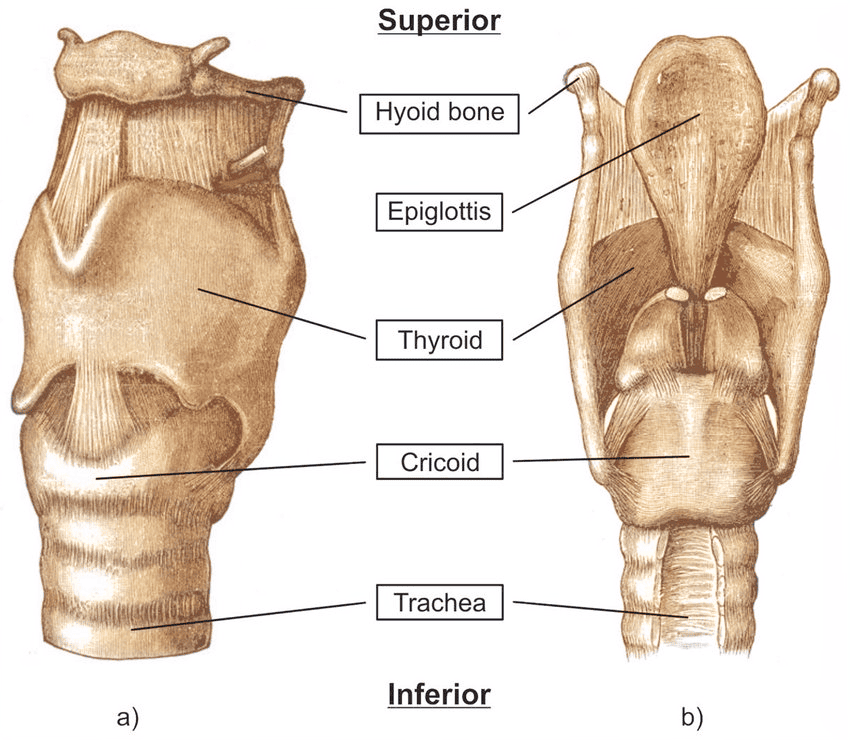
Vocal Cords:
The larynx contains two pairs of mucosal folds:
- True Vocal Cords (Vocal Folds): Vibrate as air is expelled from the lungs, producing sound.
- False Vocal Cords (Vestibular Folds): Superior to the true vocal cords; they do not produce sound but help close the glottis during swallowing.
Functions of the Larynx:
- Production of Sound (Phonation): Sound is produced when the true vocal cords vibrate. Pitch is controlled by the length and tension of the cords; volume is determined by the force of air passing over them; resonance is created by the pharynx, mouth, nasal cavity, and paranasal sinuses.
- Protection of the Lower Respiratory Tract: The epiglottis acts as a switching mechanism to route food and air into their proper channels.
- Passageway for Air: Provides an open (patent) airway between the pharynx and trachea.
- Air Conditioning: Continues to warm, filter, and humidify inspired air.
The Trachea (Windpipe)
The trachea is a flexible tube, about 10-12 cm long, that extends from the larynx into the mediastinum, where it divides into the two primary bronchi.
Structure: The wall of the trachea is composed of three layers and is supported by 16-20 C-shaped rings of hyaline cartilage.
- The cartilage rings are incomplete posteriorly, where the trachea lies against the esophagus. This allows the esophagus to expand as food is swallowed.
- The open posterior part is spanned by the trachealis muscle (smooth muscle) and connective tissue.
- Mucociliary Escalator: The inner lining of the trachea is ciliated columnar epithelium containing mucus-secreting goblet cells. The cilia beat continuously in an upward direction, propelling mucus loaded with debris toward the pharynx, where it can be swallowed or coughed out.
Functions of the Trachea:
- Support and Patency: The cartilage rings keep the trachea permanently open to allow the free passage of air.
- Mucociliary Escalator: Traps and removes particles from the airway.
- Cough Reflex: Nerve endings in the trachea are sensitive to irritation and can trigger a powerful cough to expel irritants.
- Air Conditioning: Continues warming, filtering, and humidifying air.
- Passageway for air: Carries air from the larynx to the bronchi.
- Support and Patency: The cartilage rings ensure the airway stays open.
- Mucociliary Escalator: The ciliated lining and mucus trap particles and sweep them upwards towards the larynx, where they are swallowed or coughed up. This is a very important cleaning mechanism.
- Cough Reflex: If the lining is irritated, it triggers a cough, which forcefully expels air and irritants from the airway.
- Warming, humidifying, and filtering: Continues air conditioning.
Functions related to respiration:
The Bronchi and the Bronchial Tree
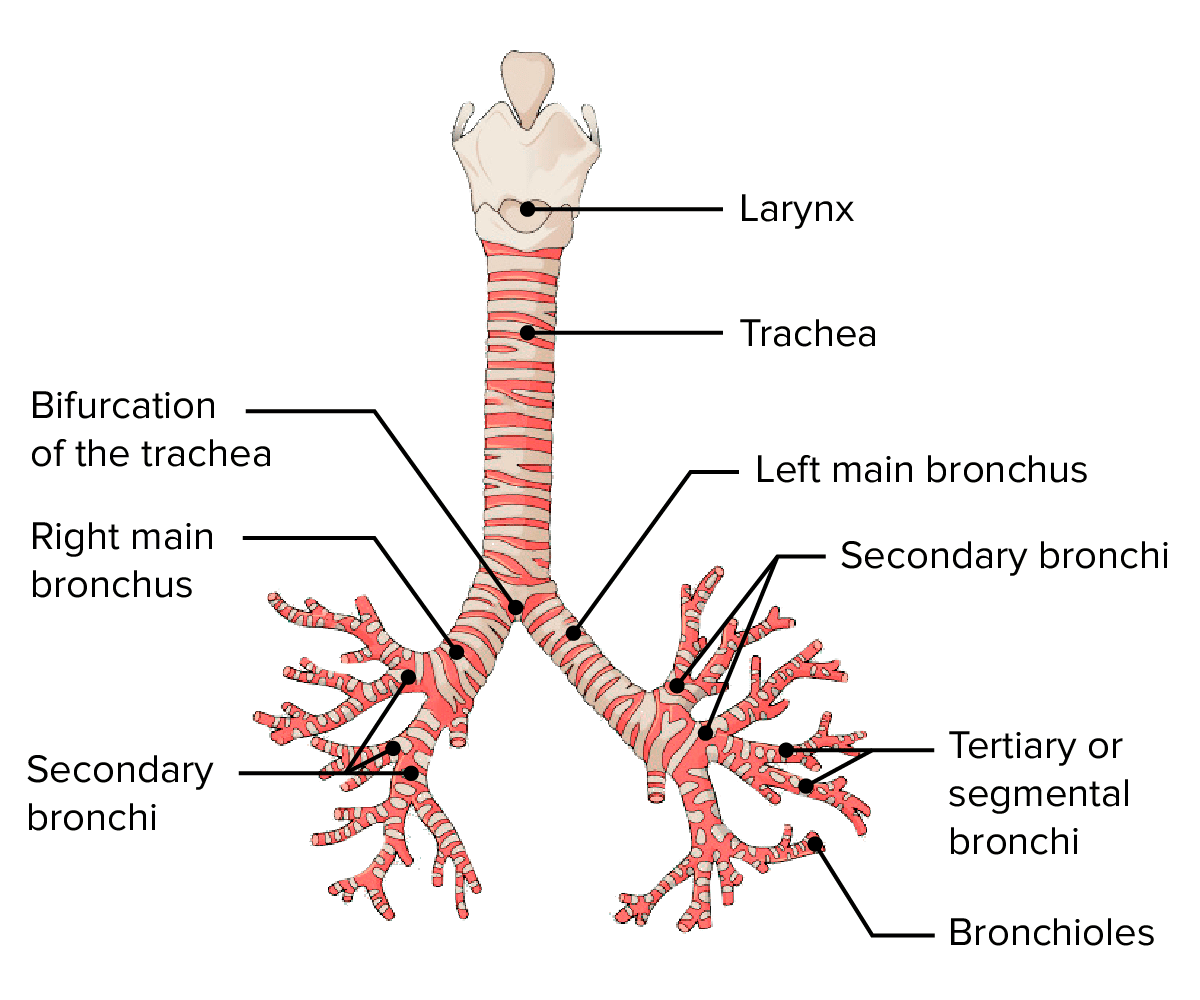
The trachea divides at a point called the carina into the right and left primary bronchi.
Location: The trachea splits into two main tubes called primary bronchi (one to each lung). These then branch repeatedly into smaller and smaller tubes within the lungs, like branches of a tree.
Structure: As the airways branch and get smaller, their structure changes:
- The cartilage rings become smaller plates and eventually disappear in the smallest airways (bronchioles). Without cartilage, these smaller airways can change diameter.
- The amount of smooth muscle in the walls increases as cartilage decreases.
- The lining changes from ciliated columnar epithelium to non-ciliated epithelium in the smallest bronchioles.
Functions related to respiration:
- Passageway for air: Carry air from the trachea deep into the lungs.
- Control of Air Entry: The smooth muscle in the walls can contract (narrowing - bronchoconstriction) or relax (widening - bronchodilation), controlling how much air flows into the lungs. This is controlled by the nervous system.
- Protection: Mucociliary escalator (in larger bronchi) continues cleaning.
Primary Bronchi:
- Right Primary Bronchus: Wider, shorter, and more vertical than the left. As a result, inhaled foreign objects are more likely to become lodged in the right bronchus.
- Left Primary Bronchus: Longer, narrower, and more horizontal.
Respiratory Bronchioles and Alveoli:
Location: The smallest bronchioles lead to even tinier tubes called respiratory bronchioles, which end in clusters of air sacs called alveoli (singular: alveolus). These are the very small, delicate parts of the lungs.
Structure:
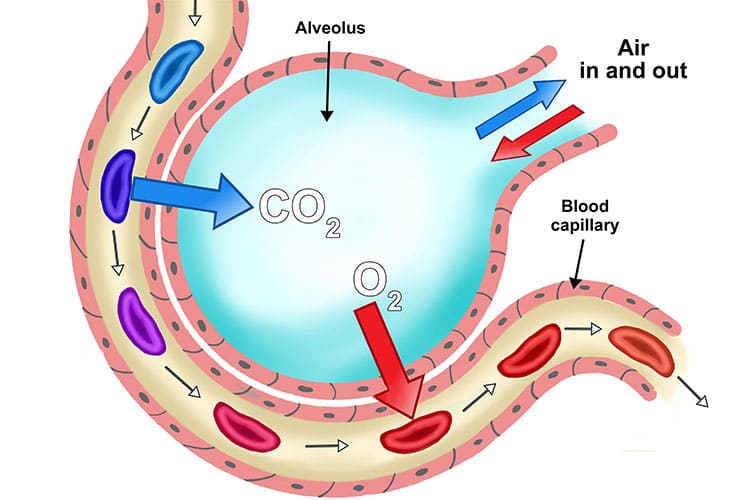
- Alveoli: Tiny, thin-walled sacs (like tiny balloons) where gas exchange happens. An adult lung has about 150 million alveoli, providing a huge surface area for gas exchange.
- Respiratory Membrane: The thin barrier between the air in the alveoli and the blood in the capillaries. It's made of the single cell layer of the alveolar wall and the single cell layer of the capillary wall, fused together. This very thin barrier (about 0.5 µm thick) is essential for quick gas diffusion.
- Surfactant: The lining of the alveoli is covered with a watery film. Special cells in the alveoli (septal cells) produce a substance called surfactant, which is a fat-protein mixture. Surfactant reduces the surface tension of the watery film, preventing the alveoli from collapsing completely between breaths and making it easier to inflate the lungs.
- Capillary Network: Each alveolus is surrounded by a dense network of tiny blood vessels called capillaries.
The Respiratory Zone: Alveoli
The respiratory zone is where gas exchange occurs. It consists of respiratory bronchioles, alveolar ducts, and alveoli (air sacs).
Alveoli: The primary sites of gas exchange. There are millions of alveoli in the lungs, providing an enormous surface area. They are surrounded by a dense network of pulmonary capillaries.
The Respiratory Membrane: A very thin (~0.5 µm) membrane that gases diffuse across. It consists of:
- The simple squamous epithelium of the alveolar wall (Type I pneumocytes).
- The fused basement membranes of the alveolar and capillary walls.
- The simple squamous endothelium of the capillary wall.
Surfactant: A detergent-like fluid secreted by Type II pneumocytes in the alveoli. It reduces the surface tension of the alveolar fluid, which is crucial for preventing the alveoli from collapsing during expiration.
The Bronchial Tree:
Upon entering the lungs at the hilum, the primary bronchi subdivide into a branching network of airways.
Primary Bronchi → Secondary (Lobar) Bronchi → Tertiary (Segmental) Bronchi → Bronchioles → Terminal Bronchioles.
Structural Changes Down the Tree:
- Cartilage: The amount of cartilage decreases, transitioning from rings to irregular plates, and is absent in the bronchioles.
- Smooth Muscle: The amount of smooth muscle increases relative to the diameter of the airway. This allows for the regulation of airflow (bronchodilation and bronchoconstriction).
- Epithelium: The lining changes from ciliated columnar to cuboidal epithelium, and goblet cells disappear in the smaller airways.
The Lungs and Pleura
The lungs are paired, cone-shaped organs that occupy most of the thoracic cavity.
Location: There are two lungs, one on each side of the chest, filling most of the thoracic cavity.
Structure: Each lung is divided into lobes (right lung has 3, left lung has 2). The lungs are made up of the air passages (bronchioles, respiratory bronchioles), alveoli, blood vessels, nerves, and connective tissue, all organised into small units called lobules.
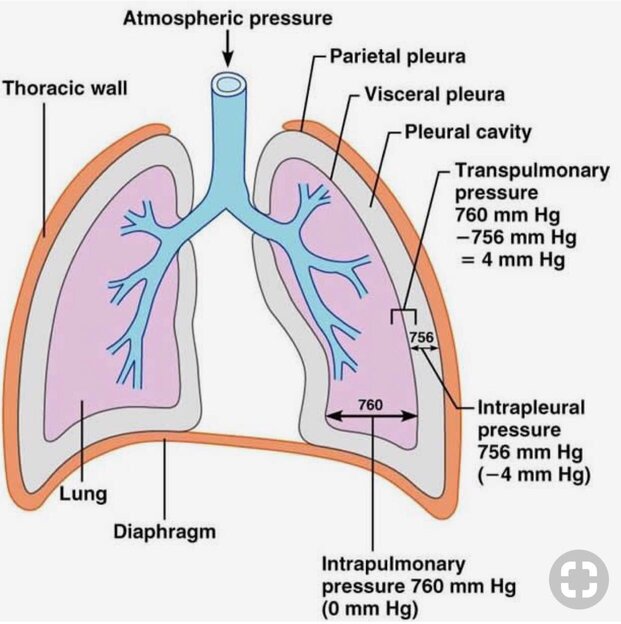
Pleura: Each lung is enclosed by a double-layered membrane called the pleura. One layer sticks to the lung (visceral pleura), and the other layer sticks to the chest wall (parietal pleura). A small space between the layers (pleural cavity) contains pleural fluid. This fluid acts as a lubricant, allowing the lungs to glide smoothly against the chest wall during breathing. The fluid also helps keep the lung expanded by creating a negative pressure between the layers.
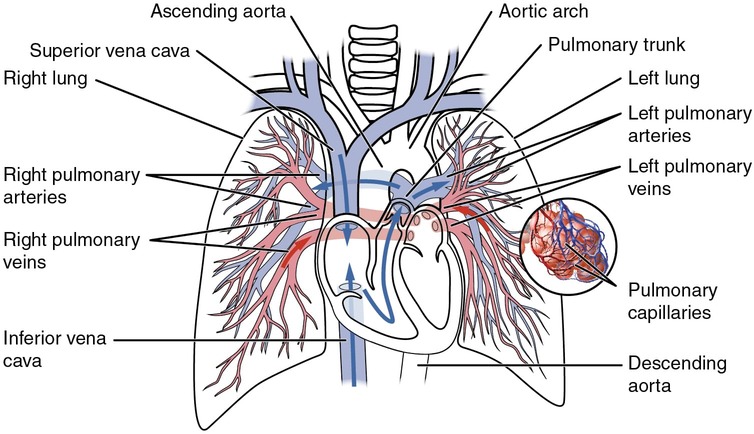
Pulmonary Blood Supply: The lungs receive blood from the heart through the pulmonary artery (carrying deoxygenated blood from the right ventricle). This artery branches extensively within the lungs, forming the capillary networks around the alveoli. Oxygenated blood returns to the heart through the pulmonary veins (entering the left atrium).
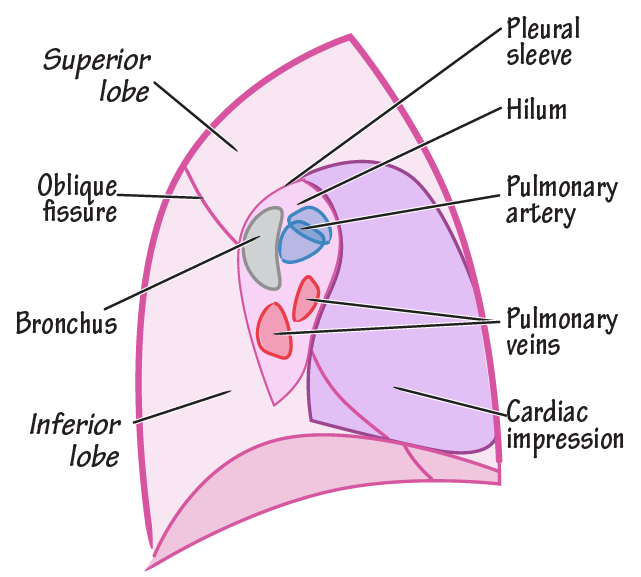
Gross Anatomy:
- Apex: The superior tip of the lung.
- Base: The inferior surface that rests on the diaphragm.
- Lobes: The right lung is larger and is divided into three lobes (superior, middle, inferior). The left lung is smaller to accommodate the heart (cardiac notch) and has only two lobes (superior, inferior).
- Hilum: An indentation on the medial surface where the primary bronchi, pulmonary blood vessels, lymphatic vessels, and nerves enter and leave the lung.
The Pleura:
The lungs are enclosed by a double-layered serous membrane called the pleura.
- Parietal Pleura: Lines the thoracic wall and the superior surface of the diaphragm.
- Visceral Pleura: Covers the external surface of the lungs.
- Pleural Cavity: A potential space between the two layers containing a thin film of pleural fluid. This fluid acts as a lubricant, allowing the lungs to glide smoothly during breathing, and creates surface tension that helps keep the lungs inflated.
Physiology of Respiration
Breathing (Pulmonary Ventilation):
The process of moving air into the lungs (inspiration) and out of the lungs (expiration). This happens because of changes in the volume and pressure inside the chest cavity, driven by the muscles of breathing. Air always flows from an area of higher pressure to an area of lower pressure.
Inspiration (Breathing In): This is an active process requiring muscle contraction. The main muscles are the diaphragm (a dome-shaped muscle below the lungs) and the external intercostal muscles (between the ribs).
- When the diaphragm contracts, it flattens and moves downwards.
- When the external intercostal muscles contract, they pull the rib cage upwards and outwards.
- These actions increase the volume of the chest cavity.
- Increasing the volume decreases the pressure inside the lungs (making it lower than the outside air pressure).
- Air flows into the lungs from the outside until the pressure equalizes.
Expiration (Breathing Out): In normal, quiet breathing, this is a passive process requiring muscle relaxation.
- The diaphragm and external intercostal muscles relax.
- The rib cage moves downwards and inwards, and the diaphragm moves upwards.
- This decreases the volume of the chest cavity.
- Decreasing the volume increases the pressure inside the lungs (making it higher than the outside air pressure).
- Air flows out of the lungs until the pressure equalizes.
Forced Breathing: During exercise or difficulty breathing, other muscles (accessory muscles) help increase the chest volume during inspiration and actively push air out during expiration (using internal intercostal and abdominal muscles).
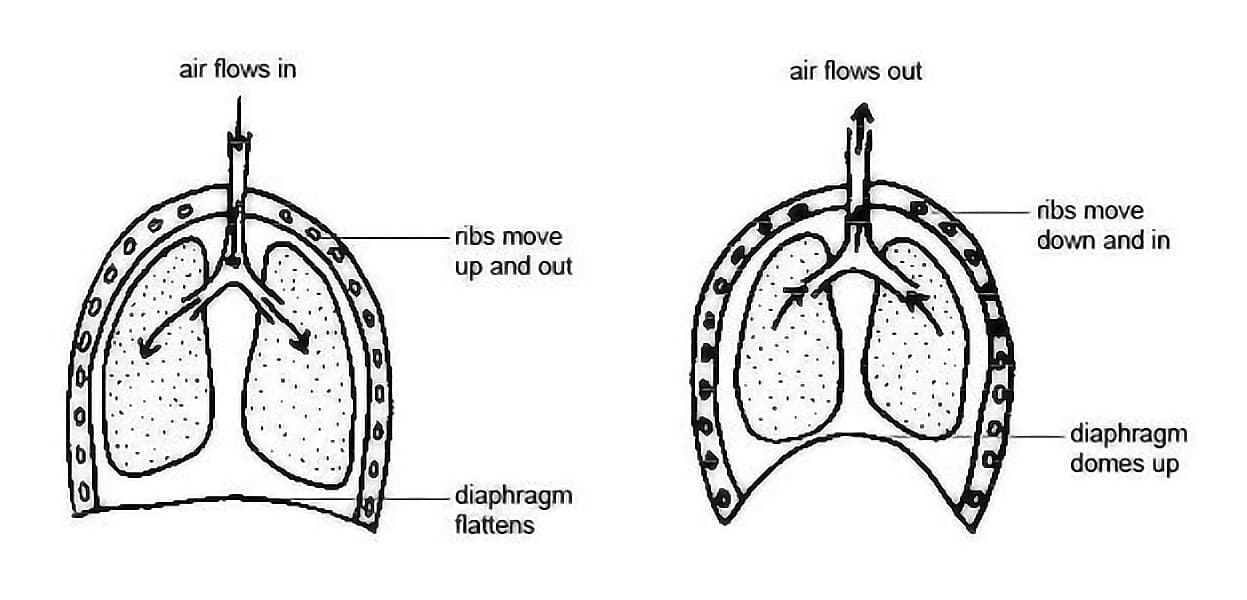
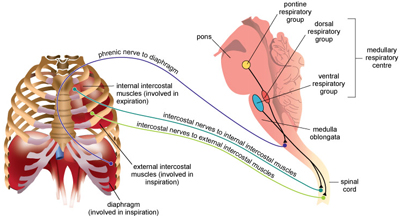
Muscles of Respiration:
- External Intercostals: Elevate the rib cage during inspiration.
- Internal Intercostals: Depress the rib cage during forced expiration.
The Breathing Cycle:
- Inspiration (Inhalation): An active process. The diaphragm contracts and flattens, and the external intercostal muscles contract, lifting the rib cage up and out. This increases the volume of the thoracic cavity, which decreases the pressure inside the lungs. Air flows into the lungs, down its pressure gradient.
- Expiration (Exhalation): A passive process during quiet breathing. The diaphragm and external intercostals relax. The natural elasticity of the lungs causes them to recoil, decreasing the thoracic volume and increasing the pressure inside. Air flows out of the lungs. Forced expiration is an active process involving the internal intercostals and abdominal muscles.
Lung Volumes and Capacities
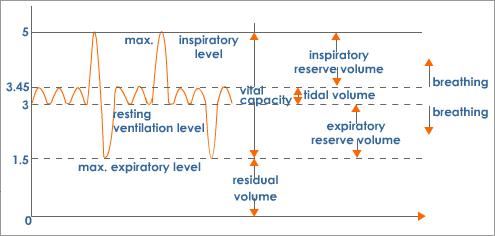
- Tidal Volume (TV): The amount of air inhaled or exhaled with each normal breath at rest (~500 mL).
- Inspiratory Reserve Volume (IRV): The extra volume of air that can be forcibly inhaled after a normal tidal inspiration.
- Expiratory Reserve Volume (ERV): The extra volume of air that can be forcibly exhaled after a normal tidal expiration.
- Residual Volume (RV): The volume of air that remains in the lungs even after a maximal exhalation. This keeps the alveoli open.
- Vital Capacity (VC): The maximum amount of air that can be exhaled after a maximal inhalation (VC = TV + IRV + ERV).
- Total Lung Capacity (TLC): The maximum amount of air the lungs can hold (TLC = VC + RV).
- Anatomical Dead Space: The volume of air that remains in the conducting airways (trachea, bronchi) and does not participate in gas exchange (~150 mL).
Gas Exchange (External and Internal Respiration)
This happens in two places:
External Respiration (at the Lungs): Exchange of gases between the air in the alveoli and the blood in the pulmonary capillaries.
- The partial pressure of oxygen (PO₂) in the alveoli is high, while in the deoxygenated blood arriving at the lungs, it is low. Therefore, oxygen diffuses from the alveoli into the blood.
- The partial pressure of carbon dioxide (PCO₂) in the deoxygenated blood is high, while in the alveoli, it is low. Therefore, carbon dioxide diffuses from the blood into the alveoli to be exhaled.
Simply
- Blood arriving at the lungs is low in oxygen and high in carbon dioxide.
- Oxygen moves from the air in the alveoli (where oxygen concentration is high) into the blood in the capillaries (where it's low) by diffusion.
- Carbon dioxide moves from the blood in the capillaries (where carbon dioxide concentration is high) into the air in the alveoli (where it's low) by diffusion.
- This exchange happens quickly across the very thin respiratory membrane.
Internal Respiration (at the Tissues): Exchange of gases between the blood in the systemic capillaries and the body tissues/cells.
- The PO₂ in the oxygenated blood arriving at the tissues is high, while in the tissue cells (which are using oxygen), it is low. Oxygen diffuses from the blood into the tissues.
- The PCO₂ in the tissue cells (where it is produced) is high, while in the blood, it is low. Carbon dioxide diffuses from the tissues into the blood.
Simply
- Blood arriving at the tissues is high in oxygen and low in carbon dioxide.
- Oxygen moves from the blood in the capillaries (where oxygen concentration is high) into the body tissues (where it's low) by diffusion.
- Carbon dioxide (a waste product of cell activity) moves from the body tissues (where carbon dioxide concentration is high) into the blood in the capillaries (where it's low) by diffusion.
Gas Transport in Blood (Transport of Gases in the Bloodstream)
- Oxygen: Mostly carried bound to haemoglobin inside red blood cells. A small amount is dissolved in plasma. Haemoglobin picks up oxygen in the lungs and releases it in the tissues where it is needed.
- Carbon Dioxide: Carried in the blood in three ways: mostly as bicarbonate ions in the plasma, some bound to haemoglobin, and a small amount dissolved in plasma. Carbon dioxide is picked up in the tissues and transported to the lungs to be breathed out.
Oxygen Transport:
- 98.5% is bound to hemoglobin (Hb) in red blood cells, forming oxyhemoglobin (HbO₂).
- 1.5% is dissolved in the plasma.
- The binding of oxygen to hemoglobin is reversible. Factors that promote the release (dissociation) of oxygen at the tissues include: low PO₂, high PCO₂, low pH (acidity), and high temperature.
Carbon Dioxide Transport:
- 70% is transported as bicarbonate ions (HCO₃⁻) in the plasma. This is the most important mechanism and plays a crucial role in buffering blood pH.
- 23% is bound to hemoglobin, forming carbaminohemoglobin.
- 7% is dissolved in the plasma.
Control of Respiration
Breathing is largely an involuntary process controlled by respiratory centers in the brainstem.
Neural Control:
- Medulla Oblongata: Contains the primary respiratory rhythmicity center that sets the basic pace and rhythm of breathing.
- Pons: Contains centers (pneumotaxic and apneustic) that modify and fine-tune the breathing rhythm.
Chemical Control (Chemoreceptors):
These receptors monitor chemical changes in the blood and cerebrospinal fluid (CSF) and send signals to the respiratory centers.
- Central Chemoreceptors: Located in the medulla, they are highly sensitive to changes in PCO₂ (and thus pH) of the CSF. An increase in PCO₂ is the most powerful stimulus for increasing the rate and depth of breathing.
- Peripheral Chemoreceptors: Located in the aortic arch and carotid arteries. They are sensitive to changes in blood PCO₂, pH, and, to a lesser extent, PO₂.
Regulation of Breathing(Control of Respiration)
Beyond the main neural centers and chemoreceptors, several other factors can influence the rate and depth of breathing.
Breathing is mostly an involuntary process controlled by the brain, but you can consciously control it sometimes (e.g., when speaking).
- The main control center is in the brainstem (medulla and pons), called the respiratory centre. It sends signals to the breathing muscles.
- Chemoreceptors in the brain and large arteries (aorta and carotid arteries) sense the levels of oxygen and carbon dioxide in the blood.
- If carbon dioxide levels rise or oxygen levels fall, these chemoreceptors send signals to the respiratory centre, telling it to increase the rate and depth of breathing to correct the levels. The body is very sensitive to changes in carbon dioxide levels.
Factors Influencing Respiration:
- Speech and Singing: We intentionally manipulate our breathing patterns to produce sound.
- Emotional Displays: Strong emotions like crying, laughing, fear, or anxiety can significantly alter the breathing pattern via the limbic system and hypothalamus.
- In a fever (hyperthermia), metabolic rate increases, leading to increased respiration.
- In low body temperature (hypothermia), metabolic and respiratory rates are depressed.
Consequences of Ageing on the Respiratory System:
- The elasticity of the lungs decreases, reducing their ability to recoil passively during expiration.
- The chest wall becomes more rigid, and respiratory muscles weaken, which can decrease the vital capacity.
- The sensitivity of chemoreceptors may decline.
- There is a higher risk of respiratory infections like pneumonia due to a less efficient mucociliary escalator and a decline in immune function.
Physiological Variables Affecting Breathing
For pulmonary ventilation to be effective, three key physical factors must be considered. These factors determine the effort required to breathe.Elasticity: This is the natural ability of the lung tissue to recoil, or return to its normal shape, after being stretched during inspiration. The elastic fibers in the lung's connective tissue are responsible for this property. Elastic recoil is the primary driving force behind quiet, passive expiration.
Clinical Correlation: In diseases like emphysema, the elastic tissue is destroyed, leading to a loss of elasticity. This makes expiration difficult and requires muscular effort (forced expiration).
- High Compliance: Means the lungs stretch easily (like a well-used balloon).
- Low Compliance: Means the lungs resist expansion and require more effort to inflate (like a new, stiff balloon). Compliance can be decreased by conditions that make the lungs stiffer, such as pulmonary fibrosis (scarring) or a lack of surfactant.
- Bronchodilation: An increase in the diameter of the bronchioles (caused by sympathetic stimulation) decreases resistance and allows for greater airflow.
- Bronchoconstriction: A decrease in the diameter of the bronchioles (caused by parasympathetic stimulation, histamine, or irritants) increases resistance and makes breathing more difficult.
Clinical Correlation: In asthma, inflammation and bronchoconstriction dramatically increase airway resistance, leading to wheezing and difficulty breathing.
Ageing and the Respiratory System
As people get older, changes naturally occur in the respiratory system:
- The lungs become less elastic, making it harder to breathe out effectively. This can cause smaller airways to collapse.
- The rib cage becomes stiffer, and the breathing muscles may become weaker, reducing the amount of air that can be moved in and out of the lungs.
- The mucus production may decrease, and the cilia may become less effective at clearing mucus and particles, increasing the risk of infections.
- The reflexes (like coughing) may become less sensitive.
- The body's response to low oxygen or high carbon dioxide may become less efficient.
These changes can make older adults more prone to breathing problems and infections.
Common Deviations from Normal Structure and Function (Disorders)
When parts of the respiratory system are not working normally, it leads to symptoms like coughing, difficulty breathing (dyspnoea), wheezing, chest pain, and fever. Disorders can affect different parts of the system:
- Upper Respiratory Tract Infections: Common infections like the common cold (usually viral, causes runny nose, sore throat) and influenza (viral, more severe symptoms like fever, muscle pain). Can also include sinusitis (inflammation of sinuses) and tonsillitis (inflammation of tonsils).
- Laryngitis: Inflammation of the larynx, often causing hoarseness or loss of voice.
- Bronchitis: Inflammation of the bronchi. Can be acute (often follows a cold, with cough) or chronic (long-term, with persistent cough and mucus, often due to smoking). Chronic bronchitis involves increased mucus and narrowing airways.
- Emphysema: Damage to the walls of the alveoli, causing them to lose elasticity and break down. This reduces the surface area for gas exchange and makes it hard to breathe out, trapping air in the lungs. Often linked to smoking.
- Asthma: A condition where the airways (bronchioles) become inflamed and narrow temporarily (bronchoconstriction) in response to certain triggers (like allergens or cold air). This makes it difficult to breathe, causing wheezing and shortness of breath. It involves inflammation, increased mucus, and muscle tightening in the airways.
- Pneumonia: An infection of the alveoli in the lungs, where air sacs fill with fluid and pus, making gas exchange difficult. It can be caused by bacteria, viruses, or fungi.
- Tuberculosis (TB): A serious bacterial infection of the lungs (though it can affect other body parts). It is caused by Mycobacterium tuberculosis and leads to inflammation and damage in the lung tissue.
- Lung Collapse (Atelectasis): Occurs when a part of the lung (or the whole lung) deflates or collapses. Can be caused by a blockage in an airway (preventing air from reaching that part) or by air or fluid building up in the space outside the lung (pleural cavity), pushing on the lung.
- Pneumothorax: Air in the pleural cavity, causing the lung to collapse. Can happen spontaneously or due to injury.
- Pleural Effusion: Excess fluid in the pleural cavity, causing the lung to collapse. Can be due to heart failure, infection, or other conditions.
- Pneumoconioses: Lung diseases caused by inhaling dusts (like coal dust - coal worker's pneumoconiosis, or silica dust - silicosis) over a long time. Leads to inflammation and fibrosis (scarring) in the lungs, making them stiff and reducing lung function.
- Lung Tumours: Abnormal growths in the lung tissue. Can be benign (non-cancerous) or malignant (cancerous). Lung cancer is often linked to smoking and can grow locally or spread to other parts of the body.
These are just some examples of how the normal structure and function of the respiratory system can be affected, leading to different illnesses. Understanding the normal state helps us recognize when things deviate and a person needs care.
Deviations and Disorders of the Respiratory System
Deviations from the normal structure and function of the respiratory system can lead to a variety of diseases and disorders.
- Asthma: A chronic inflammatory disease of the airways characterized by episodes of wheezing, breathlessness, chest tightness, and coughing. These episodes are caused by bronchospasm (sudden constriction of smooth muscle in the airways), inflammation, and excessive mucus production, all of which increase airway resistance.
- Chronic Obstructive Pulmonary Disease (COPD): A progressive disease that makes it hard to breathe, characterized by irreversible airflow limitation. It is most commonly caused by long-term exposure to irritants like tobacco smoke. COPD includes two main conditions:
- Chronic Bronchitis: Characterized by long-term inflammation of the bronchi, leading to excessive mucus production and a chronic cough.
- Emphysema: Characterized by the destruction of the alveolar walls, which reduces the surface area available for gas exchange and causes a loss of lung elasticity, trapping air in the lungs.
- Pneumonia: An infection that inflames the alveoli in one or both lungs. The alveoli may fill with fluid or pus, causing cough, fever, chills, and difficulty breathing. It can be caused by bacteria, viruses, or fungi.
- Tuberculosis (TB): An infectious disease caused by the bacterium Mycobacterium tuberculosis. It typically affects the lungs, where the immune system forms fibrous nodules (tubercles) around the bacteria. This can lead to lung tissue damage and respiratory failure.
- Lung Cancer: Uncontrolled growth of abnormal cells in the lung tissue. It is the leading cause of cancer death worldwide, strongly associated with smoking.
- Acute Respiratory Distress Syndrome (ARDS): A life-threatening lung condition that prevents enough oxygen from getting to the lungs and into the blood. It is often caused by severe illness, trauma, or infection, and leads to widespread inflammation and fluid leakage into the alveoli, often coupled with a breakdown of surfactant.
Summary and Revision Questions
The respiratory system is a marvel of biological engineering, precisely designed to facilitate the vital exchange of gases between the body and the environment. Its anatomy, from the large airways to the microscopic alveoli, is perfectly suited for its functions of ventilation, gas exchange, and protection. The physiological processes of breathing, gas transport, and neural control work in a coordinated manner to maintain stable levels of oxygen and carbon dioxide in the blood, adapting constantly to the body's changing metabolic demands.
To consolidate your understanding of this system, please review the following key areas:
Anatomy:
- State the organs of the upper and lower respiratory systems.
- Describe the location and detailed structure of the nasal cavity.
- Describe the location and structure of the pharynx, including its three divisions.
- Describe the structure of the larynx and outline the functions of its different cartilages.
- Describe the gross structure of the lungs, including their lobes, surfaces, and pleura.
- Trace the pathway of air through the entire bronchial tree, from the primary bronchus to the alveoli.
- Explain the structural changes that occur in the airways as they become progressively smaller.
- Write short notes on the pleura and identify its main functions.
- What is surfactant, where is it produced, and what are its functions?
- Outline the five main differences between the right and left lung/bronchus.
Physiology:
- Outline the main functions of the nose, pharynx, larynx, and trachea.
- State the primary muscles involved in quiet and forced respiration.
- Explain the mechanical events that occur during one cycle of inspiration and expiration.
- Define the following terms: compliance, elasticity, and airway resistance. How do they affect breathing?
- Explain the principal lung volumes and capacities (TV, IRV, ERV, RV, VC, TLC).
- Define and compare the processes of internal and external respiration, using the concept of partial pressure gradients.
- Describe the main ways that oxygen and carbon dioxide are transported in the blood. What factors promote the release of oxygen from hemoglobin?
- Explain the main mechanisms by which respiration is controlled, including the roles of the medulla, pons, and chemoreceptors.
More Questions
- What are the main functions of the respiratory system?
- List the major parts of the air passages in order from the nose to the alveoli.
- Describe how the nasal cavity conditions the air you breathe in.
- Explain the role of the epiglottis during swallowing.
- What keeps the trachea from collapsing?
- What is the function of the smooth muscle in the walls of the bronchioles?
- Where does gas exchange take place in the lungs?
- Describe the respiratory membrane and explain why it is important for gas exchange.
- What is the function of surfactant in the lungs?
- Explain how inspiration and expiration occur, mentioning the muscles involved.
- What is the difference between external respiration and internal respiration?
- How is oxygen transported in the blood? How is carbon dioxide transported?
- How does the brainstem control breathing? What role do chemoreceptors play?
- List three ways the respiratory system changes as a person gets older.
- Briefly describe how inflammation affects the airways in conditions like bronchitis or asthma.
- What happens to the alveoli in emphysema? How does this affect breathing?
- What is pneumonia?
References:
- Cohen, JB and Hull, L.K (2016) Memmlers – The Human body in Health and diseases 13th Edition, Wolters, Kluwer.
- Scott, N.W. (2011) Anatomy and Physiology made incredibly easy. 1st Edition. Wolwers Kluwers, Lippincotts Williams and Wilkins.
- Moore, L. K, Agur, M.R.A and Dailey, F.A. (2015) Essential Clinical Anatomy.15th Edition. Wolters Kluwer.
- Cohen, J.B and Hull, L.K (2016) Memmler's Structure and Function of the Human Body. 11th Edition. Wolters Kluwer, China
- Snell, S. R. (2012) Clinical Anatomy by Regions. 9th Edition. Wolters Kluwer, Lippincott Williams and Wilkins, China
- Wingerd, B, (2014) The Human Body-Concepts of Anatomy and Physiology. 3rd Edition Lippincott Williams and Wilkins and Wolters Kluwer.
- Rohen, Y.H-Orecoll. (2015) Anatomy.A Photographic Atlas 8th Edition. Lippincott Williams & Wilkins.
- Waugh, A., & Grant, A. (2014). Ross and Wilson Anatomy & Physiology in Health and Illness (12th ed.). Churchill Livingstone Elsevier.

Well equipped with notes.. everything is good 😊 and understandable