THYROTOXICOSIS.
Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism.
Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormone by the thyroid gland. Some, however, use the terms interchangeably
Overactive thyroid, is called hyperthyreosis/Hyperthyroidism

Anatomy of the Thyroid gland.
The thyroid gland is located in the lower portion of the neck in front of the larynx and the trachea at the level of 5th, 6th & 7th cervical and the 1st thoracic vertebrae.
It is a highly vascular gland that weighs about 25 g and resembles a butterfly shape.
It has two lobes, one on either side.
The lobes are joined by isthmus in front of the trachea
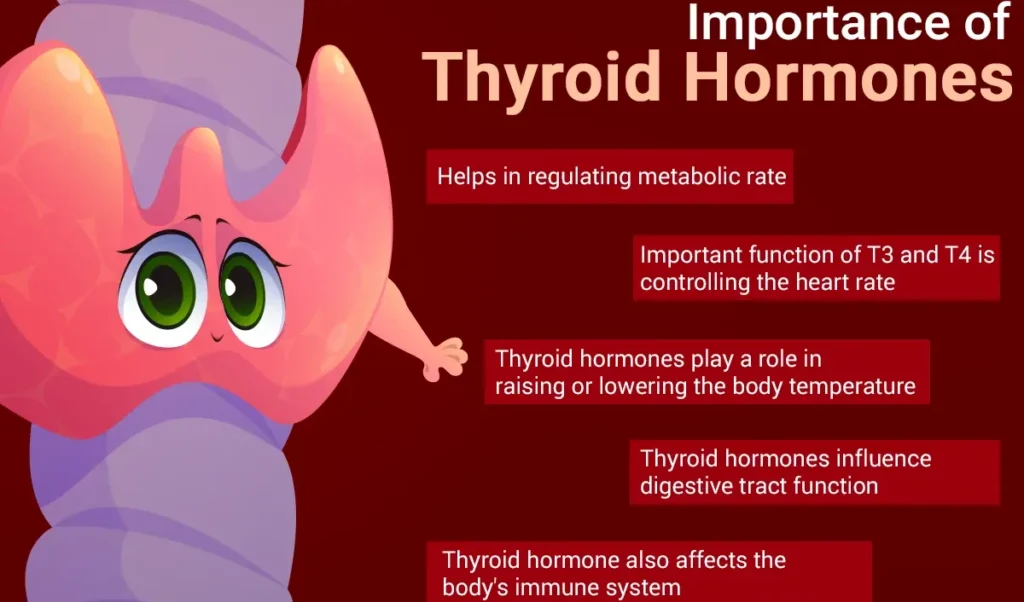
Its major function is to produce thyroid hormone (T3 and T4 and calcium).
These hormones are responsible for growth and regulating metabolic rate
Common Terms
a. Hyperthyroidism: Hyperthyroidism is a medical condition characterized by excessive production of thyroid hormones by the thyroid gland. This overactivity of the thyroid gland leads to an increased metabolic rate in the body, resulting in symptoms such as weight loss, rapid heartbeat, irritability, heat intolerance, and tremors.
b. Thyrotoxicosis: Thyrotoxicosis is a condition in which there is an excess of thyroid hormones circulating in the bloodstream. It can be caused by various factors, including hyperthyroidism (excessive thyroid hormone production), inflammation of the thyroid gland, or external sources of thyroid hormone intake. The symptoms of thyrotoxicosis are similar to those of hyperthyroidism.
c. Graves’ disease: Graves’ disease is an autoimmune disorder that is the most common cause of hyperthyroidism. It occurs when the immune system mistakenly attacks the thyroid gland, causing it to produce excessive amounts of thyroid hormones. People with Graves’ disease often experience symptoms such as goiter (enlarged thyroid gland), bulging eyes (exophthalmos), weight loss, tremors, and heat intolerance.
d. Hypothyroidism: Hypothyroidism is a condition characterized by an underactive thyroid gland, leading to insufficient production of thyroid hormones. This deficiency of thyroid hormones slows down the body’s metabolism, resulting in symptoms such as fatigue, weight gain, cold intolerance, constipation, and depression.
e. Cretinism: Cretinism is a condition that occurs when a baby is born with severe hypothyroidism or when the condition is left untreated during early childhood. It leads to stunted growth, intellectual disability, and developmental delays. Cretinism can be caused by iodine deficiency, thyroid gland abnormalities, or genetic factors.
f. Myxedema: Myxedema refers to the severe form of hypothyroidism that develops in adults. It is characterized by the accumulation of mucopolysaccharides (a complex sugar) in the connective tissues, leading to swelling and thickening of the skin. Symptoms of myxedema include extreme fatigue, cold intolerance, weight gain, dry skin, hair loss, and mental sluggishness.
g. Goiter is a medical condition characterized by the enlargement of the thyroid gland, which is located in the front of the neck. It usually appears as a visible swelling or lump in the throat area. Goiter can develop due to various reasons, including iodine deficiency, inflammation of the thyroid gland, or certain thyroid disorders such as Graves’ disease or Hashimoto’s thyroiditis.
h. Hashimoto’s thyroiditis is an autoimmune disorder that affects the thyroid gland which can result in an underactive thyroid or hypothyroidism. In this condition, the immune system mistakenly attacks the thyroid gland, leading to chronic inflammation and damage to the gland.
i. Thyroid storm: Thyroid storm, also known as thyrotoxic crisis, is a life-threatening condition characterized by an extreme and sudden exacerbation of the symptoms of hyperthyroidism. It usually occurs in individuals with untreated or poorly controlled hyperthyroidism, often as a result of Graves’ disease. Symptoms include high fever, severe agitation, delirium, rapid heartbeat, high blood pressure, vomiting, diarrhea, and jaundice. Thyroid storm requires immediate medical attention and hospitalization. Treatment includes medications to block the production and release of thyroid hormones, as well as supportive care to manage symptoms and stabilize vital signs.
Why we need the Thyroid Gland & Hormones
1. Regulation of Metabolism: The thyroid gland plays a central role in regulating metabolism, influencing the rate at which cells convert nutrients into energy. It does so by producing and releasing thyroid hormones (triiodothyronine or T3 and thyroxine or T4), which control the body’s metabolic processes.
2. Body Temperature Control: Thyroid hormones help regulate body temperature by influencing heat production and heat loss mechanisms. They help maintain the body’s core temperature within a normal range.
3. Growth and Development: Thyroid hormones are important for proper growth and development in children. They are essential for the normal development of the skeletal system, brain, and other organs. Insufficient thyroid hormone production can lead to growth and developmental delays.
4. Brain Function: Thyroid hormones are necessary for the normal functioning of the brain. They play a role in cognitive function, mood regulation, memory, and overall mental well-being.
5. Energy Levels: Thyroid hormones contribute to energy production in the body. They help convert food into usable energy, ensuring adequate energy levels for daily activities.
6. Heart Function: Thyroid hormones have an impact on heart rate, heart rhythm, and cardiac output. They help regulate the overall function of the cardiovascular system.
7. Muscle Function: Thyroid hormones are involved in maintaining muscle tone and strength. They contribute to muscle contraction and overall muscle function.
8. Digestion: Proper thyroid function is necessary for healthy digestion. Thyroid hormones influence the movement of food through the digestive tract and the secretion of digestive enzymes.
9. Reproductive Health: Thyroid hormones play a role in reproductive health, including menstrual cycle regulation in women. Thyroid disorders can affect fertility, pregnancy outcomes, and the health of the developing fetus.
10. Maintenance of Healthy Skin, Hair, and Nails: Optimal thyroid function is important for maintaining healthy skin, hair, and nails. Thyroid hormones contribute to the growth, maintenance, and integrity of these structures.

Causes of Hyperthyroidism and/or Thyrotoxicosis
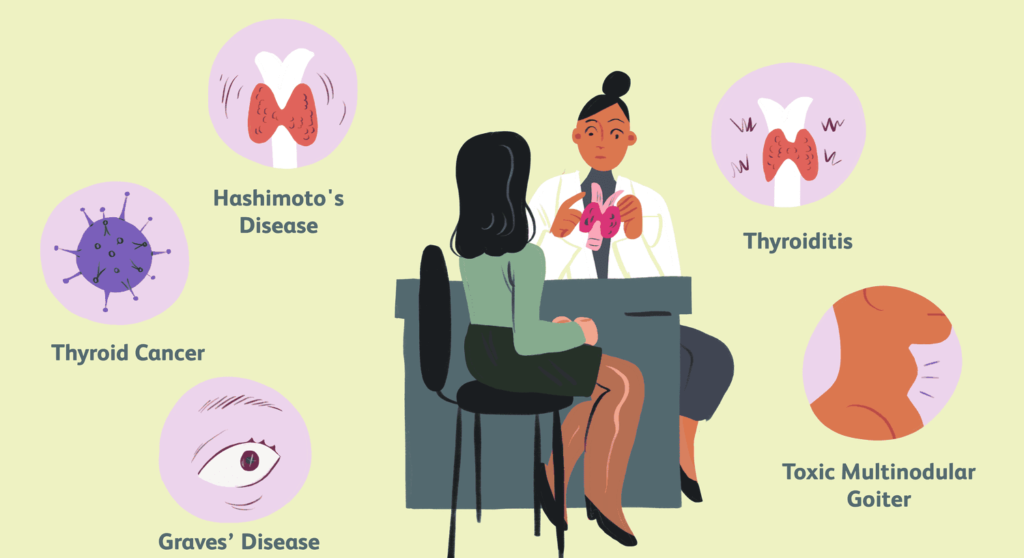
- Graves’ Disease: An autoimmune disease, Graves’ disease is the most common etiology worldwide, with a prevalence of 50-80%. It is often linked to varying iodine levels in the diet. Graves’ disease is more prevalent in females, occurring eight times more frequently in women than in men, and is commonly diagnosed in young females aged 20-40 years.
- Toxic Thyroid Adenoma: Common in Switzerland (53%), this etiology is believed to be atypical due to a low level of dietary iodine in the country. It involves the development of a toxic adenoma in the thyroid.
- Toxic Multinodular Goiter: This condition is characterized by the presence of multiple nodules in the thyroid gland, contributing to excessive thyroid hormone production.
- Thyroiditis: Inflammation of the thyroid, such as Hashimoto’s thyroiditis (immune-mediated hypothyroidism) and subacute thyroiditis (de Quervain’s), can initially lead to excess thyroid hormone secretion and progress to gland dysfunction, resulting in hypothyroidism.
- Medication and Exogenous Thyroid Hormone: Consumption of excess thyroid hormone tablets or ingestion of ground beef contaminated with thyroid tissue can cause hyperthyroidism. Amiodarone, an antiarrhythmic drug, may lead to under- or overactivity of the thyroid.
- Postpartum Thyroiditis (PPT): Affecting about 7% of women after childbirth, PPT undergoes several phases, with the initial phase being hyperthyroidism. This usually corrects itself without treatment.
- Struma Ovarii: A rare form of monodermal teratoma containing mostly thyroid tissue, leading to hyperthyroidism.
- Excess Iodine Consumption: Particularly from algae like kelp, can contribute to hyperthyroidism.
- Excessive Thyroid Hormone Supplements: Taking too much thyroid hormone in the form of supplements, such as levothyroxine, can lead to thyrotoxicosis.
- Pituitary Adenoma: Hypersecretion of thyroid-stimulating hormone (TSH) due to a pituitary adenoma accounts for less than 1 percent of hyperthyroidism cases.
General Causes of The above conditions(In Common Terms)
- Autoimmune Disorders: Autoimmune disorders, such as Hashimoto’s thyroiditis and Graves’ disease, are among the most common causes of thyroid problems. In Hashimoto’s thyroiditis, the immune system attacks and damages the thyroid gland, leading to hypothyroidism. In Graves’ disease, the immune system stimulates the thyroid gland, causing excessive production of thyroid hormones and resulting in hyperthyroidism.
- Iodine Deficiency or Excess: Adequate iodine intake is crucial for proper thyroid function, as iodine is a key component in the synthesis of thyroid hormones. An inadequate intake of iodine can lead to hypothyroidism and goiter. Conversely, excessive iodine intake can disrupt thyroid function and potentially cause hyperthyroidism. Governments provide iodized table salts as a way to avoid less iodine intake.
- Thyroid Nodules: Thyroid nodules are abnormal growths or lumps that form within the thyroid gland. They can be benign (noncancerous) or malignant (cancerous). Thyroid nodules may cause problems by affecting hormone production or through physical compression of surrounding structures, leading to symptoms or requiring medical intervention.
- Medications and Medical Treatments: Certain medications and medical treatments can interfere with thyroid function. For example, certain drugs, such as lithium, can contribute to hypothyroidism or hyperthyroidism. Radiation therapy to the head and neck region, often used in the treatment of certain cancers, can also affect thyroid function.
- Congenital Thyroid Disorders: Some individuals may be born with congenital thyroid disorders, such as congenital hypothyroidism. This condition occurs when the thyroid gland does not develop properly or is absent at birth, resulting in inadequate thyroid hormone production. Early detection and treatment are critical to prevent developmental and growth problems.
- Genetic Factors: Genetic factors can contribute to an increased risk of developing thyroid problems. Certain gene mutations or a family history of thyroid disorders may predispose individuals to conditions like thyroid cancer or autoimmune thyroid diseases.
- Inflammation and Infection: Inflammation of the thyroid gland, known as thyroiditis, can disrupt thyroid function. Viral or bacterial infections can also affect the thyroid gland and potentially lead to thyroid problems.

Signs and symptoms of Thyrotoxicosis
Thyroid hormone plays a crucial role in normal cellular function. When in excess, it not only over-stimulates metabolism but also increases the effects of the sympathetic nervous system, leading to a “speeding up” of various body systems. This results in symptoms resembling an overdose of epinephrine (adrenaline). Hyperthyroidism may manifest with various symptoms, and while some individuals may be asymptomatic, others may experience significant clinical signs.
Symptoms
- Nervousness: Elevated thyroid hormones stimulate the nervous system, leading to increased sensitivity and heightened feelings of nervousness.
- Irritability: The overstimulation of the sympathetic nervous system can result in irritability.
- Increased perspiration: Hyperactive metabolism causes an increase in sweat production as the body tries to cool down.
- Heart racing: Excess thyroid hormones accelerate heart rate and may cause palpitations.
- Hand tremors: Stimulated nervous system and increased metabolic activity contribute to hand tremors.
- Anxiety: Elevated thyroid hormone levels can induce a constant state of anxiety.
- Difficulty sleeping: Hyperthyroidism disrupts normal sleep patterns, leading to insomnia.
- Thinning of the skin: Increased metabolism may affect skin thickness and texture.
- Fine brittle hair: Changes in hormone levels can impact hair growth and texture.
- Muscular weakness: Thyroid hormones influence muscle function, leading to weakness, especially in the upper arms and thighs.
- More frequent bowel movements: Accelerated metabolism speeds up digestive processes, causing more frequent bowel movements and diarrhea.
- Weight loss: Increased metabolism burns calories rapidly, resulting in weight loss despite a heightened appetite.
- Vomiting: Gastrointestinal disturbances, including increased stomach activity, can lead to vomiting.
- Changes in menstrual flow: Altered hormone levels affect the menstrual cycle, leading to lighter periods or longer cycles in women.
Major Clinical Signs:
- Weight loss: Accelerated metabolism and increased calorie consumption contribute to weight loss.
- Anxiety: Overstimulation of the nervous system manifests as heightened anxiety.
- Heat intolerance: Elevated metabolism generates more internal heat, causing intolerance to warm environments.
- Hair loss: Changes in hormone levels impact hair follicles, resulting in hair loss, particularly in the outer third of the eyebrows.
- Muscle aches: Thyroid hormones influence muscle function, leading to aches and weakness.
- Weakness: Muscular weakness is a common symptom of hyperthyroidism.
- Fatigue: Despite increased activity, individuals may experience fatigue due to the strain on the body.
- Hyperactivity: Elevated metabolism and increased energy levels contribute to hyperactivity.
- Irritability: Overstimulation of the nervous system can lead to irritability.
- High blood sugar: Thyroid hormones can impact glucose metabolism, leading to elevated blood sugar levels.
- Excessive urination: Altered kidney function due to hormone imbalances can result in increased urination.
- Excessive thirst: Increased fluid loss through urine may lead to excessive thirst.
- Delirium: Severe cases of hyperthyroidism can cause mental confusion and delirium.
- Tremor: Increased nervous system activity may manifest as tremors in various parts of the body.
- Pretibial myxedema: Specific to Graves’ disease, it involves skin changes, swelling, and redness on the shins.
- Emotional lability: Mood swings and emotional instability can occur due to hormonal fluctuations.
- Sweating: Excessive sweating is a common symptom of hyperthyroidism.
- Panic attacks: The combination of heightened nervous system activity and anxiety can lead to panic attacks.
- Inability to concentrate and memory problems: Cognitive functions may be affected, leading to difficulties in concentration and memory.
Physical Symptoms:
- Palpitations: Increased heart rate and irregular heart rhythms may cause palpitations.
- Abnormal heart rhythms: Hyperthyroidism can disrupt normal heart rhythms, notably causing atrial fibrillation.
- Shortness of breath: Respiratory and cardiovascular effects may result in shortness of breath (dyspnea).
- Loss of libido: Hormonal imbalances can impact sexual desire and lead to a loss of libido.
- Gynecomastia and feminization: Altered hormone levels may cause breast enlargement (gynecomastia) and feminine characteristics in males.
Note:
- An association between thyroid disease and myasthenia gravis has been recognized, with approximately 5% of patients with myasthenia gravis also having hyperthyroidism.
- In Graves’ disease, ophthalmopathy may cause enlarged eyes due to swelling eye muscles pushing the eyes forward, often with one or both eyes bulging.
- Swelling of the front of the neck (goiter) may also occur.
Minor Ocular Signs:
- Eyelid retraction (“stare”): Overactive thyroid hormones can affect the muscles that control eyelid movement, leading to a wide-eyed or “staring” appearance.
- Extraocular muscle weakness: Weakness in the muscles that control eye movement may result in difficulties in moving the eyes.
- Lid-lag (von Graefe’s sign): A characteristic eye movement sign where the upper eyelid lags behind the downward movement of the eye.
- Double vision: Weakened eye muscles may cause double vision.

Exophthalmos/Proptosis in Graves’ Disease:
- Exophthalmos or proptosis, the protrusion of the eyeball, is unique to hyperthyroidism caused by Graves’ disease. It results from immune-mediated inflammation in the retro-orbital fat, leading to forward protrusion of the eyes. Exophthalmos, when present with hyperthyroidism, is diagnostic of Graves’ disease.
Diagnosis and Investigation
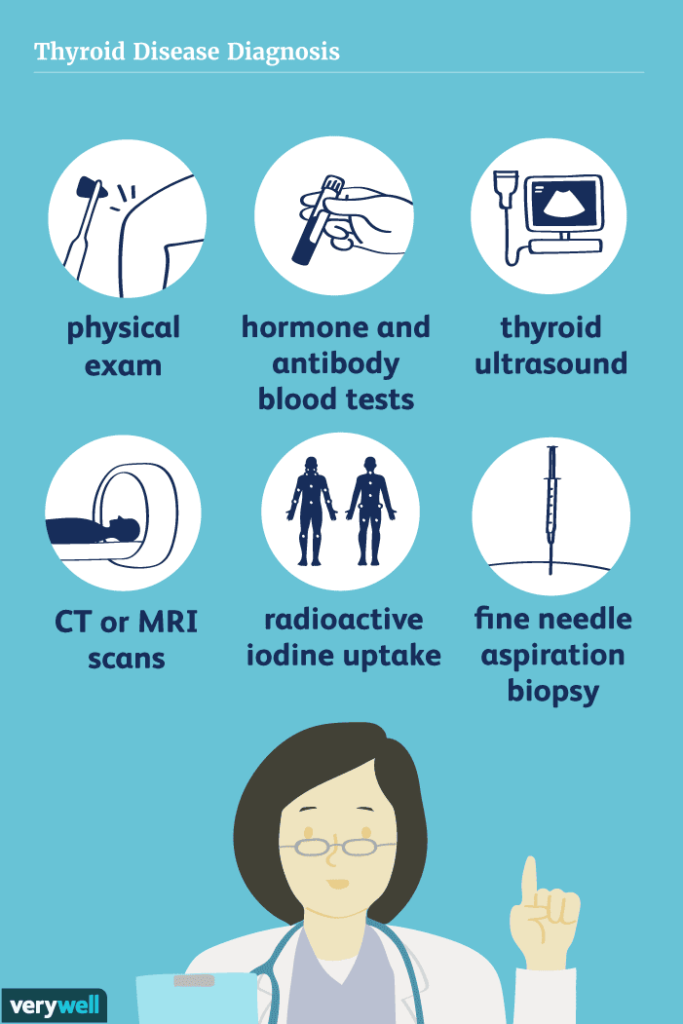
- Physical examination: enlarged, bumpy or tender gland through the neck, Eyes for swelling, redness or bulging, Heart for for a rapid heartbeat and irregular heartbeats, Hands for tremors, Skin if its moist and warm.
Blood Tests:
- The Thyroid Stimulating Hormone (TSH) Test measures TSH levels, a hormone from the pituitary gland that stimulates the thyroid. Abnormal levels may indicate hyperthyroidism or hypothyroidism.
- Thyroid Hormone (T3 and T4) Tests evaluate T3 and T4 hormone levels. Elevated levels may suggest hyperthyroidism, while decreased levels may indicate hypothyroidism.
- Thyroid Antibody Tests check for antibodies linked to autoimmune thyroid disorders like Hashimoto’s thyroiditis or Graves’ disease.
- Thyroid Function Panel combines TSH, T3, and T4 tests for a comprehensive thyroid function assessment.
Imaging Studies:
- Ultrasound uses sound waves to create thyroid gland images, aiding in identifying nodules, goiter, or structural abnormalities.
- Thyroid Scan utilizes radioactive tracers to assess overall thyroid structure and function.
- Radioactive uptake study i.e. For this test, a small, safe dose of radioactive iodine (also called a radiotracer) is taken by mouth to see how much of it your thyroid gland absorbs. After 6 to 24 hours later, the neck is scanned with a device called a gamma probe to see how much of the radioactive iodine your thyroid has absorbed. If your it absorbs a lot, it means that your thyroid gland is producing too much thyroxine (T4)
Fine-Needle Aspiration (FNA) Biopsy:
- In cases of suspicious thyroid nodules or potential cancer, FNA Biopsy extracts a sample for laboratory analysis.
Thyroid Imaging:
- Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) assess the thyroid and adjacent structures when further evaluation is needed.
ADDITIONAL DIAGNOSTIC MEASURES
- TSH Measurement: Initial test for suspected hyperthyroidism, assessing TSH levels produced by the pituitary gland, regulated by the hypothalamus.
- Antibody Tests: Checking specific antibodies like anti-TSH-receptor antibodies in Graves’ disease aids in diagnosis, as they indicate autoimmune thyroid disorders.
- Confirmation Blood Tests: Confirms hyperthyroidism with blood tests showing low TSH and elevated T4 and T3 levels. Low TSH indicates excess thyroid hormone.
- Radioactive Iodine Uptake Test: Measures iodine absorption by the thyroid. Hyperthyroid individuals absorb more iodine, including radioactive iodine used for measurement.
- Thyroid Scan: Conducted with the uptake test, it visually examines the over-functioning gland, producing images for characterization.
- Thyroid Scintigraphy: Useful in distinguishing causes of hyperthyroidism and thyroiditis. Combines an iodine uptake test and a scan with a gamma camera for comprehensive evaluation.
Medical Management of Hyperthyroidism:
Antithyroid Medications:
- – Propylthiouracil (PTU): Adult dose is usually 100-150 mg three times a day. Side effects may include liver toxicity, rash, joint pain, and agranulocytosis (a rare but serious condition characterized by a low white blood cell count).
- – Methimazole (Tapazole): Adult dose is 10-30 mg once daily or divided into two doses. Side effects may include rash, itching, nausea, and agranulocytosis.
Beta-Blockers:
- – Used to alleviate symptoms associated with hyperthyroidism such as rapid heart rate, tremors, and anxiety. Commonly prescribed beta-blockers include propranolol and atenolol. Adult doses may vary, and side effects can include fatigue, dizziness, and low blood pressure.
Radioactive Iodine (RAI) Therapy:
- Administered orally to destroy or reduce the activity of the overactive thyroid gland. Side effects may include temporary worsening of hyperthyroid symptoms, neck tenderness, and radiation sickness.
Management of Thyrotoxicosis
Aims
- To reduce the activity of the thyroid gland
- To reduce heart rate (hypertension)
- To remove part of thyroid gland
Pre-operatively
- Admission: The patient is admitted 32 days before surgery in surgical ward.
- Position: The patient is made to lie in a comfortable position according to her
choice. - History taking: Patient’s history is taken to details about the patient’s life which includes:
– Demographic data
– Past history
– Medical history for diseases like diabetes, liver cirrhosis e.t.c
– Past family history eg hypertension
– Actual history to rule out the real cause of the disease - Observation
– Vital observation eg TPR/BP to rule out vital abnormalities
– General observation i.e head to toe rule out abnormalities (JACCOLD)
– Specific observations eg palpation of the enlarged gland to any abnormality - Inform the doctor about patient
- On waiting for the doctor the following are done: – orientation of the
patient, On arrival of the doctor, he will then order for investigations.
Investigation
– Chest x-ray
– Thyroid function test. (TFT).
– Biopsy of thyroid gland for cytology and histology.
– Indirect laryngoscopy - Medical Management: The doctor will then prescribe preoperative medications depending on the results from lab mainly;
- Carbimazole 10-15 mg O.D X 12/52 then reduce to 5 mg 8hrly last
dose given prior to surgery. - Lugols iodine 0.3-0.9ml tds in milk 10 times prior to surgery until
the day of surgery. - Propranolol 40 – 80 mg 12 hourly incase of increased BP.
- Diazepam 5mg b.d to seduce the patient
- Digoxin 0.25mg o.d if atrial fibrillation is detected
- Nursing care
- Explain the procedure, the benefits and outcomes of the operation
and consent form obtained. - Re-assurance
- Give the informed consent form to be signed
- Clean the patient and dress the patient in theater gown
- Obtain blood sample for Hb estimations & grouping
- Inspect and clean operation site if instructed.
- Theater is informed about the patient and the patient is then taken to the theater for operation.
- In the theater, partial thyroidectomy is done and the patient transferred to the recovery room.
- Ward staff are called to go for their patient.
MANAGEMENT: POST-THYROIDECTOMY (Incase of Surgery)
- On receiving information from the theater nurse, two nurses go to receive the patient.
- Patients vital observations are taken especially respiratory rate and pulse to confirm whether the patient is alive or dead.
- The patient is then transferred back to the ward and laid on a post operative bed after receiving theater instructions about the patient.
- Position in recovery position
- Observations taken 1/4 hourly, 1/2 hourly, 1 hourly until fully recovered.
- Post operative medications. As Doctor will prescribe the following
> Analgesics like – pethidine 50mg-100mg IM in 3 doses, then continues with
– IV tramadol 100mg tds X 1/7
– Sedatives like Diazepam 10-15mg - Specific nursing care: which include the following;
- Care of the tube: The drainage tube is removed not later than 48hrs after the operation according to discharges
- Care of the wound: Dressing are changed whenever soiled
- Stitches removed on the 3rd-4th day, only as instructed by the doctor. Ensuring constant drainage in a drainage bottle or dressing.
- Intubation if respiratory edema occurs.
- Close observation for hemorrhage.
- Creating a calm environment, possibly giving drugs to encourage sleep.
- Care of drain and sutures; changing drainage 24 hourly, sutures removed on the third or fourth day.
- Minimizing neck movement to reduce pain.
- Administering analgesics to reduce pain.
- Monitoring vitals every 2 hours to detect complications like thyroid storm or infections.
- Giving antibiotics; ceftriaxone 2g 24 hourly.
- Diet: High calories diet is ordered to satisfy hunger & to prevent tissue breakdown. Milk is encouraged to be taken then high carbohydrate diet, snacks
high in proteins, minerals and vitamins A, B6, and C are recommended. - Daily Nursing care. Oral care skin care. Bowel & bladder care
- Physiotherapy. Patient is encouraged to do some exercise of the throat and then do some deep breathing and coughing exercise.
- Psycho therapy
- Fluid monitoring. Fluid intake and output is monitored, maintained and recorded on patient fluid balance charts.
NURSING INTERVENTIONS
1. Assess Thyroid Function: Monitor the patient’s thyroid hormone levels and symptoms to evaluate the effectiveness of treatment and detect any changes in thyroid function.
2. Medication Administration: Administer prescribed medications, such as thyroid hormone replacement or antithyroid medications, ensuring accurate dosage, timing, and appropriate route of administration.
3. Educate Patients: Provide comprehensive education to patients and their families about their specific thyroid problem, including the condition, treatment plan, medication regimen, and potential side effects.
4. Monitor Vital Signs: Regularly monitor the patient’s vital signs, including heart rate, blood pressure, and temperature, to assess the impact of thyroid dysfunction and medication therapy.
5. Support Emotional Well-being: Offer emotional support and create a therapeutic environment to help patients cope with the emotional and psychological aspects of living with a thyroid problem.
6. Promote Comfort: Implement comfort measures to alleviate symptoms such as pain, fatigue, and muscle weakness. Encourage rest and provide pain management techniques as appropriate.
7. Nutritional Support: Collaborate with dietitians to develop appropriate dietary plans that support optimal thyroid function and address any specific nutritional needs or restrictions.
8. Monitor Weight and Fluid Balance: Regularly assess and monitor the patient’s weight and fluid balance to identify any changes or imbalances that may indicate thyroid dysfunction.
9. Assist with Thyroid Imaging: Coordinate and assist with thyroid imaging procedures, such as ultrasound or radioactive iodine uptake scans, ensuring patient comfort and safety.
10. Collaborate with Healthcare Team: Work collaboratively with physicians, endocrinologists, and other healthcare professionals to ensure coordinated care and effective communication regarding the patient’s thyroid problem and treatment plan.
11. Monitor for Side Effects: Monitor patients for any potential side effects or adverse reactions to medications, particularly those related to thyroid hormone replacement or antithyroid medications.
12. Educate on Self-Care: Teach patients self-care strategies to manage their condition effectively, including proper medication management, self-monitoring of symptoms, and recognizing signs of worsening thyroid dysfunction.
13. Provide Thyroidectomy Care: If the patient undergoes thyroidectomy (surgical removal of the thyroid gland), provide post-operative care, including wound care, pain management, and monitoring for complications.
14. Manage Thyroid Storm: In cases of thyroid storm (life-threatening condition with severe hyperthyroidism symptoms), closely monitor vital signs, administer medications as ordered (such as antithyroid medications and beta-blockers), and provide supportive care.
16. Advice on Discharge: Collaborate with the healthcare team to plan for the patient’s discharge, ensuring proper medication instructions, follow-up appointments, and education on long-term management and self-care.
Complications of Thyroidectomy:
- Hemorrhage due to hyper-vascularization of the thyroid gland.
- Thyroid crisis (thyroid storm) characterized by rapid pulse, raised temperature, sweating, and confusion.
- Tetany due to removal or trauma to parathyroid glands; characterized by tingling and numbness of the face, lips, and hands.
- Sore throat.
- Hoarseness due to damage to the recurrent laryngeal nerve.
- Hypothyroidism due to thyroid removal.
- Recurrent thyrotoxicosis.
- Respiratory obstruction due to laryngeal edema.
- Wound infection.
Advice on discharge. Advise the patient,
- To complete prescribed medications
- To do exercise to avoid complication of the neck
- On personal hygiene to prevent secondary infections.
- To eat a well balanced diet.
- To buy a cream like lanolin and rub it on the healed wound.
- To not take drugs when not prescribed by the physician
- To avoid high temperatures.
- To come back for review as indicated.
- Follow-up Care: Regular monitoring of thyroid function through blood tests. Adjustments in medication dosage as needed.
- Patient Education: Guidance on dietary restrictions and adherence to medication. Awareness of symptoms requiring prompt medical attention.
- Long-Term Management: Maintenance therapy based on the chosen treatment modality. Continuous monitoring for potential complications.
Thyroid Storm Management:
- Prompt Recognition: Immediate identification of extreme hyperthyroid symptoms.
- Resuscitation Measures: Intravenous beta-blockers like propranolol for rapid symptom control. Thioamide, such as methimazole, to inhibit thyroid hormone production.
- Additional Interventions: Administration of iodinated radiocontrast agent or iodine solution. Intravenous steroid, hydrocortisone, to address inflammation.
- Intensive Monitoring: Continuous assessment of vital signs and thyroid function. Adjustment of treatment based on response.
Complications of Hyperthyroidism/Thyrotoxicosis:
- Heart Problems: Elevated thyroid hormones can lead to increased heart rate (tachycardia) and irregular heart rhythms (arrhythmias), such as atrial fibrillation. Chronic strain on the heart may result in heart failure or other cardiovascular complications.
- Osteoporosis: Hyperthyroidism can accelerate bone turnover, leading to decreased bone density and an increased risk of osteoporosis. Imbalances in calcium and vitamin D metabolism may further contribute to bone loss.
- Thyroid Storm: In rare cases, untreated or severe hyperthyroidism can progress to a life-threatening condition known as thyroid storm. This involves a sudden and severe exacerbation of hyperthyroid symptoms, leading to high fever, extreme tachycardia, and organ failure.
- Eye Complications (Graves’ Ophthalmopathy): Graves’ disease, a common cause of hyperthyroidism, is associated with eye complications. Immune-mediated inflammation in the eye tissues can lead to proptosis (bulging eyes), double vision, and in severe cases, vision impairment.
- Skin and Hair Issues: Hyperthyroidism may affect skin and hair health. Thinning of the skin and fine, brittle hair are common symptoms. In some cases, individuals may experience skin changes such as redness or swelling.
- Psychological Complications: Chronic anxiety, emotional lability, and irritability associated with hyperthyroidism can contribute to psychological complications. Severe cases may lead to mental health issues such as depression or exacerbate pre-existing conditions.
- Menstrual Irregularities: Altered levels of thyroid hormones can impact the menstrual cycle in women. Menstrual flow may lighten, and periods may become irregular, with longer cycles than usual.
- Muscle Weakness and Wasting: Hyperthyroidism can lead to muscle weakness, especially in the upper arms and thighs. In severe cases, prolonged muscle breakdown may result in muscle wasting.
- Gastrointestinal Issues: Increased bowel movements and diarrhea are common symptoms of hyperthyroidism. Chronic gastrointestinal issues may lead to nutritional deficiencies and weight loss.
- Impaired Concentration and Memory: Cognitive function may be affected, causing difficulties in concentration and memory. The combination of anxiety and hormonal imbalances can contribute to cognitive impairment.
- Thyroid Crisis (Thyroid Storm): In extreme cases, uncontrolled hyperthyroidism can progress to a thyroid crisis or storm. This life-threatening condition involves a sudden surge in symptoms, including hyperthermia, cardiovascular collapse, and neurological dysfunction.
- Pregnancy Complications: Hyperthyroidism during pregnancy can pose risks to both the mother and the developing fetus. Complications may include preterm birth, low birth weight, and maternal heart issues.
- Liver and Kidney Dysfunction: Prolonged hyperthyroidism may impact liver and kidney function. Elevated thyroid hormones can affect organ metabolism and contribute to dysfunction over time.


Thanks so much,,for the great work,,,
Help with,,, the notes of “hyperparathyroidism
Thanks for the good presentation
Thank you
Thanx you so much
Good work, thanks