Table of Contents
ToggleEYE INFECTIONS
Eye infections occur when bacteria, viruses, fungi, or other microorganisms invade the tissues of the eye or its surrounding structures.
These infections can range from mild to severe and may involve various parts of the eye, including the conjunctiva, cornea, eyelid, or internal ocular structures.
- Conjunctivitis: Conjunctivitis, commonly known as ‘pink eye’, is a widespread infection typically caused by bacteria or viruses. It is highly contagious and often affects children in schools or other group settings where it can easily spread from child to child. It gives the eye a pink or reddish tinge.
- Trachoma: Trachoma is a common infection in certain developing regions and is one of the leading causes of blindness in those areas. It can be spread by flies, and reinfection is a significant problem. Proper hygiene and access to treatment are crucial.
- Endophthalmitis: Endophthalmitis is a bacterial infection that affects the inside of the eye, often due to an injury or, rarely, after eye surgery. Without immediate and powerful antibiotic treatment, it can cause blindness. A type of mold can also cause this condition, although it is rare.
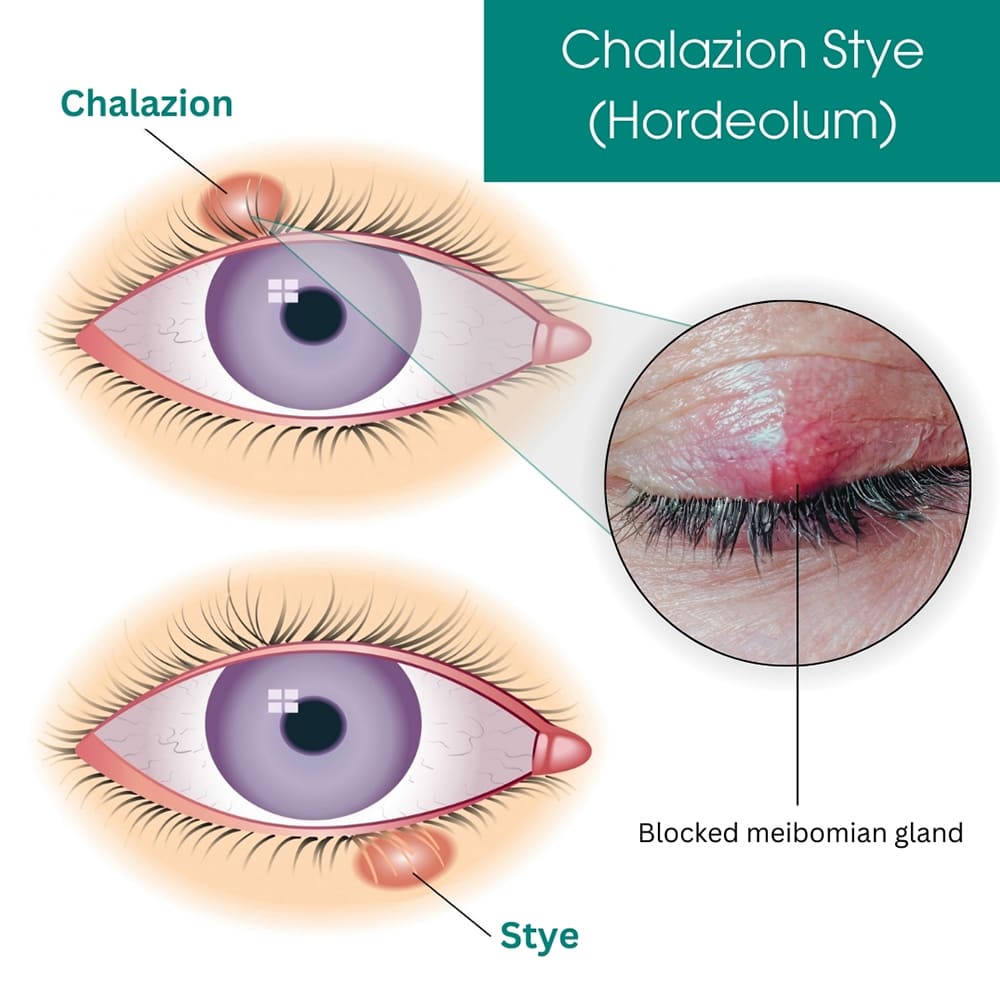
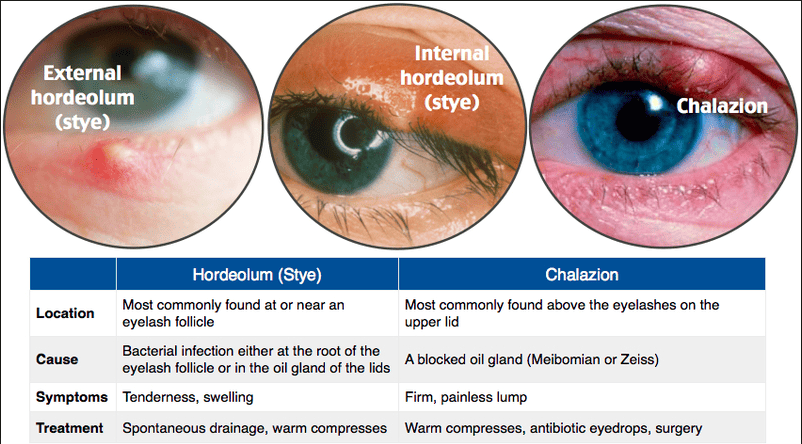
- Stye or Chalazion: These infections affect the inside of the eyelids.
- Dacryocystitis: This is an infection of the tear ducts, leading to inflammation and blockage of the tear drainage system.
- Corneal Ulcers: These can be caused by infections and may be associated with the use of contact lenses. Corneal ulcers are serious and can lead to severe vision loss if not treated promptly.
- Orbital Cellulitis: This infection attacks the soft tissue around the eyelids and is a serious emergency. It requires immediate treatment to prevent the infection from spreading.
- Keratitis: An infection or inflammation of the cornea. Can be caused by bacteria, viruses, fungi, or parasites. Symptoms: Pain, redness, blurred vision, photophobia, and corneal cloudiness.
- Blepharitis: An infection or inflammation of the eyelid margins. Commonly caused by bacterial infection, seborrheic dermatitis, or blocked oil glands. Symptoms: Crusty eyelids, redness, swelling, burning sensation, and itching.
- Uveitis: Inflammation of the uvea, often associated with autoimmune conditions or infections. Symptoms: Eye pain, redness, blurred vision, and photophobia.
STYE (HORDEOLUM)
A stye, also known as a hordeolum, is a localized infection of the hair follicle or the oil-producing (sebaceous) or sweat glands in the eyelid.
A stye, or hordeolum, is a localized, painful bacterial infection or inflammation of the glands or hair follicles at the edge of the eyelid.
Commonly caused by Staphylococcus aureus.
It often results from Staphylococcus aureus infection and can occur either externally (on the lid margin) or internally (within the eyelid).
Types of Stye
1. Internal Hordeolum: Affects the Meibomian glands, which are sebaceous glands located within the eyelid.
Clinical Characteristics:
- The infection occurs deeper within the eyelid, often making it more painful and tender.
- Swelling may involve the entire eyelid.
- The internal stye can sometimes evolve into a chalazion if it becomes chronic and non-infectious.
2. External Hordeolum: Involves the glands of Zeis (sebaceous glands) or Moll glands (sweat glands) at the base of the eyelash follicle.
Clinical Characteristics:
- Appears as a small, red, painful lump resembling a pimple on the edge of the eyelid.
- Usually less painful than an internal hordeolum.
- Often associated with localized swelling and redness around the affected area.
Causes of Stye Formation
- Bacterial Infection: Most commonly caused by Staphylococcus aureus.
- Blocked Glands: Blockage in the sebaceous glands (Meibomian, Zeis, or Moll glands) can trigger inflammation.
- Poor Eyelid Hygiene: Failure to remove makeup or debris from the eyelid margins.
- Contact Lens Misuse: Wearing lenses without proper cleaning or disinfection can introduce bacteria.
- Pre-existing Conditions: Conditions such as blepharitis, rosacea, or seborrheic dermatitis increase susceptibility.
- Immune System Deficiency: Reduced immunity can predispose individuals to bacterial infections.
Clinical Features
Early Symptoms:
- Mild itching and discomfort in the affected area.
- A sensation of fullness or heaviness in the eyelid.
Progressive Signs:
- Pain: Localized tenderness and pain, especially on palpation.
- Redness: Visible inflammation and redness at the eyelid margin or deeper within the eyelid.
- Swelling: Puffy, swollen eyelid, which may extend to the surrounding areas.
- Pus Formation: Formation of a yellowish, fluid-filled pustule near the edge of the eyelid.
- Soreness: Persistent irritation and soreness over the affected site.
Advanced Symptoms:
- Drainage of Fluid: Spontaneous rupture may release yellowish or white pus, leading to symptom relief.
- Visual Obstruction: Swelling may partially block vision in severe cases.
Management of Stye
1. General Care
Avoid Rubbing or Touching the Eye:
- Rubbing can introduce additional bacteria and exacerbate the infection.
- Rationale: Prevents spreading the infection to other areas of the eyelid or eye.
Warm Compresses:
- Apply a warm or hot compress (clean cloth dipped in warm water) for 10–15 minutes, 3–4 times a day.
- Rationale: Encourages drainage of pus, relieves pain, and reduces swelling.
2. Medications
Antibiotic Eye Ointments:
- Tetracycline 1% eye ointment applied 2–4 times daily until 2 days after the symptoms subside.
- Rationale: Reduces bacterial load, speeds up healing, and prevents further spread of infection.
Analgesics:
- Oral pain relievers like ibuprofen or paracetamol for pain relief.
- Rationale: Helps manage discomfort and swelling.
3. Eyelash Removal
- Removal of loose or infected eyelashes may be performed by a healthcare provider.
- Rationale: Prevents recurrent infections by removing the source of blockage or bacterial growth.
4. Hygiene Practices
- Clean the eyelid regularly using a sterile saline solution or lid-cleaning wipes.
- Avoid sharing towels, makeup, or other personal items to prevent the spread of bacteria.
5. Lifestyle Modifications
- Maintain proper hygiene when wearing and handling contact lenses.
- Discontinue makeup use until the stye resolves.
6. Referral to a Specialist
- In cases where the stye does not resolve or becomes recurrent, refer the patient to an ophthalmologist.
- Persistent or worsening symptoms may require surgical drainage or further investigation.
Potential Complications of Stye
- Chalazion Formation: A chronic, painless lump that can form after an internal stye resolves but leaves a residual blocked gland.
- Preseptal Cellulitis: Infection spreading to the surrounding eyelid tissues, leading to redness, swelling, and warmth.
- Recurrent Styes: Especially common in individuals with underlying conditions like blepharitis or rosacea.
Prevention of Stye
- Good Eyelid Hygiene: Regular cleaning of the eyelid margins with gentle cleansers or baby shampoo diluted with water.
- Avoid Eye Contamination: Do not touch or rub the eyes with unclean hands. Avoid using expired or contaminated eye makeup products.
- Contact Lens Care: Follow proper cleaning, storage, and replacement practices for contact lenses.
- Manage Underlying Conditions: Treat chronic eyelid conditions like blepharitis or seborrheic dermatitis to prevent blockage of the glands.
- Boost Immune Health: Maintain a healthy diet, adequate hydration, and overall wellness to reduce susceptibility to infections.

TRACHOMA
Trachoma is a chronic infection of the outer eye caused by Chlamydia trachomatis, transmitted through direct personal contact, shared towels and cloths, and flies that have come into contact with the eyes or nose of an infected person. It is a common cause of blindness.
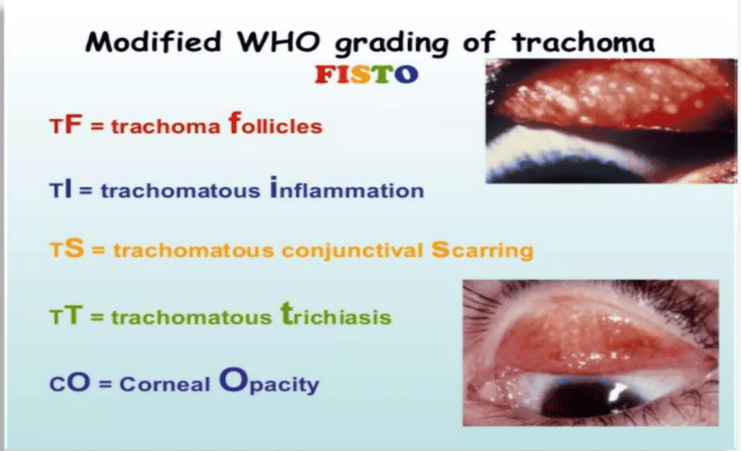
Staging of Trachoma
Stage I: Trachomatous follicles- follicular (TF). Presence of five or more follicles in the upper tarsal conjunctiva. Follicles are whitish grey or yellow elevations, paler than the surrounding conjunctiva.
Stage II: Trachomatous inflammation – intense (TI). The upper tarsal conjunctiva is red, rough, and thickened. The blood vessels, normally visible, are masked by a diffuse inflammatory infiltration or follicles.
Stage III: Trachomatous scarring (TS). Follicles disappear, leaving scars: scars are white lines, bands, or patches in the tarsal conjunctiva.
Stage IV: Trachomatous trichiasis (TT). Due to multiple scars, the margin of the eyelid turns inwards (entropion); the eyelashes rub the cornea and cause ulcerations and chronic inflammation.
Stage V: Trachomatis corneal opacity (CO). The cornea gradually loses its transparency, leading to visual impairment and blindness.
Treatment and Management of Trachoma:
Community Diagnosis: Essential to establish whether the disease is of public health importance in the community. If so, the SAFE strategy should be the appropriate approach.
The SAFE strategy stands for:
- Surgery for trachomatous trichiasis (S): Trachomatous trichiasis is the blinding stage of trachoma where the eyelashes turn inwards and rub against the eyeball, causing constant pain and light intolerance. Surgery is performed to correct this condition and prevent further damage to the cornea.
- Antibiotics (A): The application of antibiotics, especially the highly effective azithromycin, is a component of the SAFE strategy. Antibiotics are used to clear the infection and reduce the transmission of Chlamydia trachomatis. Mass drug administration of azithromycin is often conducted in endemic communities to treat and prevent trachoma.
- Facial cleanliness (F): Promoting facial cleanliness is an important preventive measure to reduce the transmission of trachoma. This includes proper hygiene practices such as washing the face with clean water and soap, especially focusing on the eyes and nose, to remove discharge and prevent the spread of infection.
- Environmental improvement (E): Improving access to water and sanitation is essential in reducing the transmission of trachoma. Inadequate access to water and sanitation facilities contributes to the spread of the disease. Environmental improvement measures aim to provide clean water, proper sanitation, and hygiene education to communities at risk
Stages I and II:
Clean eyes and face several times per day.
Antibiotic therapy: The treatment of choice is azithromycin PO:
- Children over 6 months or over 6 kg: 20 mg/kg single dose
- Adults: 1 g single dose
Failing the above, 1% tetracycline eye ointment: one application 2 times daily for 6 weeks
In children under 6 months or 6 kg: erythromycin PO (20 mg/kg 2 times daily for 14 days)
Stage III: No treatment
Stage IV: Surgical treatment
- While waiting for surgery, if regular patient follow-up is possible, taping eyelashes to the eyelid is a palliative measure that can help protect the cornea. In certain cases, this may lead to permanent correction of the trichiasis within a few months.
- The method consists of sticking the ingrowing eyelashes to the external eyelid with a thin strip of sticking plaster, making sure that the eyelid can open and close perfectly. Replace the plaster when it starts to peel off (usually once a week); continue treatment for 3 months.
- Note: Epilation of ingrowing eyelashes is not recommended since it offers only temporary relief and re-growing eyelashes are more abrasive to the cornea.
Stage V: No treatment
Prevention:
Improved Hygiene Practices:
- Encourage regular face and hand washing with clean water and soap.
- Promote the use of clean towels and avoid sharing personal items like towels and washcloths.
- Teach proper disposal of nasal and eye secretions to prevent contamination.
Access to Clean Water and Sanitation:
- Improve access to clean water sources for drinking, washing, and sanitation purposes.
- Ensure proper sanitation facilities, including toilets and latrines, to reduce the spread of infection.
Environmental Improvement:
- Control fly populations by implementing fly control measures, such as proper waste management and fly traps.
- Reduce overcrowding in households to minimize the risk of transmission.
- Improve housing conditions to prevent the accumulation of dust and dirt.
Antibiotic Treatment:
- Administer antibiotics, such as azithromycin, to affected individuals and communities to clear the infection.
- Implement mass drug administration programs in endemic areas to treat and prevent trachoma.
Surgical Intervention:
- Provide surgical treatment for advanced trachoma, known as trachomatous trichiasis, to prevent further damage to the cornea.
- Surgery can reposition the eyelashes to prevent them from rubbing against the cornea.

OPHTHALMIA NEONATORUM
Ophthalmia neonatorum, also known as neonatal conjunctivitis, is any eye infection in the first 28 days of life.
Pathophysiology:
Inflammation of the conjunctiva causes erythema, blood vessel dilation, tearing, and drainage. This reaction tends to be more serious due to reduced tear secretion, decreased immune function, decreased lysozyme activity, and the relative absence of lymphoid tissue of the conjunctiva. Neonate tears also lack immunoglobulin IgA.
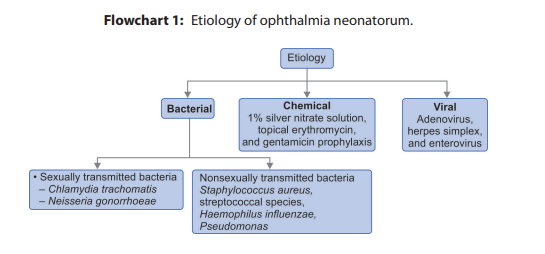
Etiology:
- Bacterial Infections: Bacterial infections are one of the major causes of septic neonatal conjunctivitis. The most common bacterial agent historically was Neisseria gonorrhoeae, which is a sexually transmitted infection. Others,
- Chlamydia trachomatis (most common): 5-14 days
- Neisseria gonorrhoeae: 3-5 days
- Staphylococcus aureus
- Pseudomonas aeruginosa
- Streptococcus spp. (including S. haemolyticus, S. pneumoniae)
- Other bacteria include Klebsiella, Proteus, Enterobacter, Serratia, and Eikenella corrodens.
- Viral Infections: Viral infections can also cause ophthalmia neonatorum, although they are less common than bacterial infections. Viral agents that can lead to neonatal conjunctivitis include herpes simplex virus, adenovirus, and enterovirus.
- Chlamydial Infection: Chlamydia trachomatis is a sexually transmitted infection that can be acquired by the mother and transmitted to the newborn during delivery. Babies born to women with untreated chlamydial infection have a 30-50% chance of developing ophthalmia neonatorum. Chlamydia trachomatis can also colonize the respiratory tract, leading to pneumonitis in some cases.
- Chemical Conjunctivitis: Aseptic neonatal conjunctivitis can be caused by exposure to certain chemicals. In the past, silver nitrate solution was used for prophylaxis, but it has been replaced by erythromycin ointment or povidone iodide in many places. Chemical conjunctivitis is becoming less common due to these changes
Presentation/Clinical Manifestations of Ophthalmia Neonatorum:
The presentation varies depending on the causative agent, but common features include:
- Eyelid swelling: Often the first sign, varying in severity from mild edema to significant swelling that may make it difficult to open the eyes.
- Discharge: Purulent (thick, yellow-green) discharge is characteristic of bacterial infections, while chlamydial infections may present with a less purulent, watery discharge that can become purulent later.
- Conjunctival redness (hyperemia): The conjunctiva will appear inflamed and red.
- Photophobia (light sensitivity): The infant may cry when exposed to light.
- Corneal involvement: In severe cases, the cornea (the transparent front part of the eye) can become cloudy or ulcerated, leading to permanent vision impairment or blindness. This is particularly true with gonococcal infections.
- Bilateral symptoms, affecting both eyes.
- Edema (swelling) of the eyelids, which may impede examination of the ocular surfaces.
- Mucopurulent conjunctivitis, characterized by a watery discharge that progresses to a copious purulent discharge in the case of chlamydial infection.
- Conjunctival edema (chemosis).
- Conjunctival pseudomembrane in severe cases.
- Corneal involvement, especially in cases of Neisseria gonorrhoeae infection, which can lead to corneal perforation.
- Epithelial edema, superficial keratitis, and possible corneal ulceration.
Ophthalmia Neonatorum: Prevention and Management
Prevention: Prevention strategies target reducing the risk of infection before, during, and after birth.
1. Antenatal (During Pregnancy):
- Regular screening for vaginal infections: Conduct regular examinations to detect vaginal discharges indicative of infections like gonorrhea and chlamydia.
- Treatment of vaginal infections: Ensure prompt and appropriate treatment of any identified vaginal infections in pregnant women using appropriate antibiotics.
- Management of high-risk pregnancies: Address conditions that may increase the risk of premature labor or prolonged rupture of membranes.
- Prevention and management of anemia: Address maternal anemia, as it can weaken the immune system and increase the risk of infection.
- Health education: Educate mothers on the importance of hygiene, including handwashing, perineal cleanliness, and avoidance of touching the eyes unnecessarily.
2. Intrapartum (During Labor):
- Sterile technique: Maintain strict sterile techniques during labor and delivery. All personnel should practice thorough hand hygiene.
- Avoid unnecessary eye swabbing: Avoid routine swabbing of the baby’s eyes during delivery unless absolutely necessary, as this can introduce infection. If swabbing is deemed necessary (e.g., for assessment), use separate sterile swabs for each eye, cleaning from the inner canthus outward.
- Isolation of infected mothers: Isolate mothers with purulent vaginal discharge to prevent transmission.
- Prophylactic antibiotics for prolonged rupture of membranes: Consider prophylactic antibiotics for mothers with prolonged rupture of membranes (PROM) exceeding 12 hours to reduce the risk of neonatal infection.
3. Postnatal (After Birth):
- Hand hygiene: Healthcare providers should perform thorough handwashing before and after handling newborns.
- Eye cleaning: Cleanse the baby’s eyes with sterile water or half-strength saline solution using a separate sterile cotton swab for each eye, cleaning from the inner to the outer canthus. Discard swabs after use.
- Avoid contact with birth fluids: Prevent the baby’s face from coming into contact with amniotic fluid.
- Educate mothers: Instruct mothers on proper hand hygiene before handling the baby and avoid touching the baby’s eyes.
- Prophylactic eye drops (during epidemics): In areas experiencing outbreaks of ophthalmia neonatorum, consider prophylactic eye drops (e.g., 1% silver nitrate or 10% sulfacetamide) immediately after birth. This practice is debated and requires careful consideration of potential side effects and local guidelines.
Management of Ophthalmia neonatorum:
Aims of Management:
The primary aims of management are to:
- Eradicate the infection.
- Prevent corneal damage and scarring.
- Preserve vision.
- Prevent transmission to others (e.g., other family members).
Management in a Maternity Centre (Limited to Mild Cases ONLY – Referral is usually necessary):
- Admission and Isolation: Admit the baby and isolate them to prevent infection spread. Position the baby on its side with the affected eye downward. Use mosquito nets to protect the baby from flies. Separate and disinfect all used materials before sending them to the laundry.
- Eye Cleaning: Cleanse the eyes with normal saline or cooled boiled water using a separate sterile swab for each eye.
- Topical Antibiotics: Apply antibiotic eye ointment (e.g., tetracycline or erythromycin) to both eyes. If ointments are unavailable, consider using diluted crystalline penicillin (see dosage instructions below).
Dosage of Diluted Crystalline Penicillin (If Ointments Unavailable – ONLY under direct medical supervision, and ideally as a temporary measure before hospital transfer):
- 100,000 IU vial: Dilute with 4 ml sterile water. Use 5 drops in each eye every 5 minutes for 6 times, then 5 drops every 10 minutes for 6 times, then 5 drops every 30 minutes for 6 times, then 5 drops every hour for 3 days.
- 500,000 IU vial: Dilute with 20 ml sterile water. Adjust dosage proportionately.
- Systemic Antibiotics (with strong caution, only when referral is significantly delayed and under medical supervision): Consider intramuscular crystalline penicillin 50,000 units/kg body weight every 12 hours for 7 days. This should be a last resort and is only acceptable if hospital transfer is delayed and a qualified medical professional has made the decision and is monitoring the infant’s response.
- Referral: Refer the patient to a hospital for definitive diagnosis (gonorrhea testing, culture and sensitivity) and treatment as soon as possible.
Referral: Refer all suspected cases of ophthalmia neonatorum, especially those with purulent discharge or corneal involvement, to a hospital.
- Assessment and Referral: Thoroughly assess the infant’s eyes. Any infant with suspected ophthalmia neonatorum, especially with purulent discharge or corneal involvement, requires immediate referral to a hospital with ophthalmology services. Do not attempt to manage significant cases in a maternity centre.
- Initial Cleaning (before referral): Gently cleanse the eyes with sterile saline or water to remove excess discharge. Use a separate cotton swab for each eye.
Management in Hospital:
- Diagnostic Testing: The physician will order an eye swab for culture and sensitivity to identify the causative organism.
- Eye Cleaning: Continue meticulous eye cleaning as previously described.
- Antibiotic Treatment: The physician will prescribe appropriate systemic and topical antibiotics based on the culture results. This may include intravenous antibiotics for severe infections. Penicillin may be used in gonococcal infections, as may other antibiotics like cefotaxime or ceftriaxone.
- Topical Antibiotic Ointments: Use Neomycin or tetracycline eye ointment to prevent eyelid adhesion.
Medical Management: Purulent discharge in the eyes of the newborn baby
→ Take history and examine
1. Rx for the baby:
- Always wear gloves.
- Cover the inflamed eye with gauze before opening for your protection.
- Clean the eye with saline or water.
- Apply tetracycline eye ointment hourly for 24 hours, then 8-hourly for 10 days.
PLUS:
- Ceftriaxone 125 mg IM stat.
- OR Erythromycin syrup 15 mg/kg body weight 6 hourly x 2/52.
2. Rx for the mother:
- Ceftriaxone 250 mg IM stat.
- PLUS: Erythromycin 500 mg for 7 days.
3. Rx for partners:
- Ciprofloxacin 500 mg stat.
- Septrin 5 tablets BD x3/7.
PLUS:
- Doxycycline 100 mg BD x7/7.
- OR Tetracycline 500 mg 6×7/7.
Educate on compliance:
- Schedule for a return visit.
- Provide mother and partner with condoms and counsel on risk reduction.
Incase of specific causative organisms;
Gonococcal Ophthalmia Neonatorum:
- The infant should be isolated for the first 24 hours of treatment.
- Eyes are irrigated every 1-2 hours with sterile isotonic saline until the discharge clears.
- For culture-positive cases or severe infections, systemic antibiotic therapy is indicated. Ceftriaxone (25-50 mg/kg IV or IM) or cefotaxime (100 mg/kg IM or IV) is usually administered as a single dose for localized infection; a 7-day course is recommended for disseminated infection.
Chlamydial Ophthalmia Neonatorum:
- Oral erythromycin suspension (40 mg/kg/day divided into four doses) is administered for 14 days.
- Topical treatment alone is insufficient; systemic therapy is essential to prevent systemic spread.
Herpes Simplex Ophthalmia Neonatorum:
- The infant requires isolation. Systemic acyclovir (20 mg/kg every 8 hours IV) for two weeks is the standard treatment.
- Topical therapy with 3% vidarabine or 0.1% iododeoxyuridine ointment (five times daily for 10 days) may be added.
- Severe cases necessitate immediate ophthalmological consultation.
Nursing Care (Maternity Centre and Hospital):
- General hygiene: Maintain meticulous hygiene, including handwashing, clean linens, and a clean environment.
- Eye care: Continue frequent eye cleaning as previously described.
- Comfort measures: Provide comfort measures to reduce the infant’s discomfort.
- Frequent eye cleaning: Gently cleanse the eyes with sterile saline or water every 2–4 hours, using a separate swab for each eye.
- Medication administration: Administer topical medications as prescribed, ensuring correct dosage and frequency.
- Monitoring: Closely monitor the infant’s response to treatment, including assessment of eyelid swelling, discharge, and corneal clarity.
- Pain management: Provide comfort measures as needed, such as cuddling and soothing techniques.
- Education: Educate the parents on the importance of adherence to the prescribed treatment regimen, proper eye cleaning techniques, and the need for follow-up appointments.
Complications:
- Corneal ulceration and scarring: This can lead to permanent visual impairment or blindness.
- Perforation of the cornea: A serious complication that requires surgical intervention.
- Endophthalmitis: Infection of the internal structures of the eye.
- Meningitis (rare, but possible, particularly with gonococcal infection): Infection of the membranes surrounding the brain and spinal cord.
- Sepsis: A life-threatening bloodstream infection.

CONJUNCTIVITIS (RED EYE)
Conjunctivitis is defined as the inflammation of the conjunctival membrane of the eye.
Types of Conjunctivitis:
- Bacterial Conjunctivitis: Caused by bacteria such as Staphylococcus or Streptococcus.
- Viral Conjunctivitis: Often caused by adenovirus.
- Allergic Conjunctivitis: Triggered by allergens like smoke, cosmetics, and medicines.
Causes of Conjunctivitis:
Bacterial:
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus pneumoniae
- Haemophilus influenzae
- Less commonly, sexually transmitted infections like Chlamydia and Gonorrhea.
Viral:
- Adenovirus
- Enteroviruses
- Herpes simplex virus
- Herpes zoster ophthalmicus
- Molluscum contagiosum
- Measles
- Mumps
- Rubella
- Infectious mononucleosis
- HIV
Allergic:
- Pollen
- Animal dander
- Dust mites
Signs and Symptoms of Conjunctivitis:
Bacterial:
- Pinkness or redness in the eye
- Burning, itching, a sensation of grittiness, or mild pain or discomfort in the eye
- Increased watering of the eye
- Thick, sticky, often yellowish discharge; can form a “crust” at night
- Swollen eyelids
- Slight sensitivity to bright light
- Swelling of lymph nodes in front of the ears
Viral:
- Pinkness or intense redness of the eye
- Burning, grittiness, or mild pain
- Watery discharge with a small amount of mucus
- Crustiness around the eyelids upon waking
- Swollen, red eyelids
- Slight sensitivity to bright light
- Swelling of lymph nodes in front of the ears
- Other viral infection symptoms like a runny nose or sore throat
Allergic:
- Watery eyes
- Itchy eyes
- Swollen and red eyelids
- Slight photophobia
Management of Conjunctivitis:
Bacterial:
- Apply chloramphenicol or gentamicin eye drops 2 or 3 hourly for 2 days, then reduce to 1 drop every 6 hours for 5 days.
- Change treatment based on culture and sensitivity results.
- Gonococcal conjunctivitis should be treated aggressively and in line with STI management guidelines.
- Limit the use of steroid eye drops to short durations.
- Mild cases often clear up within 1-2 weeks without special medical treatment.
- Clean discharge with a clean cloth, sterile pad, or cotton wool soaked in water.
- Apply lubricating eye drops (artificial tears) and avoid contact lenses until the infection clears.
Viral:
- Usually, no specific treatment is required, but antibiotic ointment can reassure the patient.
- In serious cases, systemic corticosteroids like prednisolone may be used.
- Apply a cold or warm compress, clean discharge with warm water, and use lubricating eye drops.
- Avoid contact lenses until the infection clears.
Allergic:
- Apply a cold compress to soothe symptoms.
- Use topical steroids for persistent cases but only for short periods.
- Maintain facial hygiene.
- Betamethasone or hydrocortisone eye drops every 1-2 hours until inflammation is controlled then applied 2 times daily.

