Table of Contents
TogglePeri-Operative Care (Summary)
Preparation for surgery should begin as soon as the doctor makes a diagnosis and decides that an operation is necessary. From that moment on, the patient and relatives are faced with the decision of accepting this treatment and its consequences or not.
Pre-Operative Care
Admission
- Explanation of the surgery: The patient is informed about the nature of the surgery, its purpose, and potential outcomes.
- Informed Consent: The patient provides written consent for both admission and the surgical procedure.
- Baseline Assessment: Vital signs (temperature, pulse, blood pressure, respiration), lab tests, and imaging studies are performed to establish a baseline for comparison post-surgery.
- Counseling and Reassurance: Patients receive emotional support and guidance to address anxieties and concerns.
- Addressing Patient Questions: Concerns are discussed, and questions are answered to reduce fear and anxiety.
- Spiritual Care: Patients can access spiritual support if desired, with access to religious leaders provided.
- Physical Examination: Weight, height, and nutritional status are assessed to ensure overall health.
- Site Preparation: The surgical area is marked and prepared, including shaving if necessary.
- Removal of Obstacles: Jewelry, dentures, and prosthetics are removed to prevent complications.
- IV Line Insertion: An IV line is placed to administer fluids and medications.
- Rehydration: IV fluids are given to ensure adequate hydration.
- Premedication: Prescribed medications are given to prepare the patient for surgery.
- Procedural Preparation: Procedures like nasogastric tube (NGT) placement, catheterization, and bowel irrigation are performed if needed.
- Rest and Sleep: Patients are encouraged to rest and sleep to ensure optimal recovery.
- Post-Operative Education: Patients are informed about anticipated activities and restrictions after surgery.
- NPO (Nil Per Os): Food and drink are withheld according to the doctor’s orders to prepare for surgery.
- Post-Operative Bed Preparation: The post-operative bed is prepared with necessary equipment like oxygen and suction apparatus.
Post-Operative Care
- Reception from Theater: The patient is received from the operating room with instructions from the surgical team.
- Vital Signs Monitoring: Temperature, pulse, blood pressure, respiration, and oxygen saturation are monitored regularly.
- Bleeding and Shock Monitoring: Closely observing for signs of bleeding and shock.
- Post-Operative Bed Admission: The patient is transferred to a warm, comfortable bed.
- IV Fluid and Medication Administration: Fluids and medications are administered via IV.
- Fluid Balance Chart: Fluid intake and output are meticulously recorded and monitored.
- Post-Operative Medications: Prescribed medications are administered as ordered.
- Bowel and Bladder Care: Support for bowel function and urinary elimination is provided.
- Rest and Sleep: Patients are encouraged to rest and sleep to promote healing.
- Drainage Management: Drains are properly managed and monitored to remove excess fluid.
- Pain Management: Pain medication is administered to provide comfort.
- Positioning: Patients are repositioned regularly to prevent pressure sores and promote comfort.
- Nutrition: Diet is adjusted based on patient tolerance and recovery stage.
- Wound Care: Surgical incisions are inspected and cleaned regularly.
- Bed Hygiene: The bed is kept clean and dry.
- Body and Skin Hygiene: Patients are assisted with hygiene to prevent infections.
- Physiotherapy: Breathing exercises and other physical therapy techniques are initiated to improve lung function and mobility.
- Psychological Care: Emotional support is provided to address anxiety, fear, and other psychological needs.
Advice on Discharge or Health Education
- Explanation of Surgery, Cause, and Prevention: The patient is given a clear understanding of the surgery, the underlying condition, and measures to prevent its recurrence.
- Treatment Completion: The importance of finishing the prescribed treatment plan is emphasized.
- Hygiene Maintenance: Patients are advised on maintaining good hygiene practices to prevent infections.
- Balanced Diet: The benefits of a balanced diet for overall health and recovery are explained.
- Rest and Sleep: Adequate rest and sleep are encouraged for optimal healing.
- Follow-up Appointment: The importance of attending scheduled follow-up appointments is stressed.
- Light Exercise and Activity Restriction: Patients are advised to engage in light exercise but avoid strenuous activities and heavy lifting.
Potential Complications
- Hemorrhage: Bleeding, either internal or external, may occur after surgery.
- Shock: A life-threatening condition characterized by a sudden drop in blood pressure and oxygen levels.
- Pain: Pain is a common post-operative experience, but it should be manageable with medication.
- Vomiting: Nausea and vomiting can occur due to anesthesia or changes in diet.
- Inability to Walk: Temporary difficulty in walking can result from anesthesia, pain, or muscle weakness.
- Paralytic Illness: A rare but serious complication that can affect breathing muscles.
- Constipation: Post-operative constipation is common, and measures to promote bowel function are often necessary.
- Hiccups: Hiccups can be persistent after surgery and can be uncomfortable.
- Burst Abdomen: A rare but serious complication where the surgical wound opens up.
- Incisional Hernia: A bulge or protrusion through the surgical incision.
- Infections: Infections can develop in the surgical wound or other parts of the body.
- Retention of Urine: Difficulty in urinating can occur due to anesthesia or other factors.
- Hypostatic Pneumonia: Pneumonia caused by fluid buildup in the lungs due to immobility.
EAR
- Outer Ear: The outer ear consists of the pinna (visible part of the ear) and the external auditory canal. The pinna helps collect sound waves and directs them into the ear canal.
- Middle Ear: The middle ear is an air-filled space behind the eardrum (tympanic membrane) that contains the three ossicles (tiny bones): the malleus (hammer), the incus (anvil), and the stapes (stirrup). These bones transmit sound vibrations from the eardrum to the inner ear.
- Inner Ear: The inner ear comprises the cochlea, vestibule, and semicircular canals. The cochlea is responsible for converting sound vibrations into electrical signals, which are then transmitted to the brain for interpretation. The vestibule and semicircular canals are involved in balance and spatial orientation.
Tumors of the Ear
Tumors are abnormal growths that can occur in any part of the body, including the ear.
They can be benign (non-cancerous) or malignant (cancerous).
Types of Ear Tumors:
1. Benign (Non-Cancerous) Tumors:
Ceruminous Gland Adenomas: These slow-growing tumors arise from the ceruminous glands in the ear canal, responsible for producing earwax. These glands produce cerumen, better known as earwax.
Symptoms:
- Hearing Loss: As the adenoma grows, it can block the ear canal, leading to conductive hearing loss.
- Feeling of Fullness in the Ear: The tumor can cause a feeling of pressure or fullness in the ear.
- Discharge: Some adenomas may produce a clear, watery discharge.
- Pain: In rare cases, the adenoma may become painful if it becomes inflamed or infected.
Causes: Unknown, but may be linked to genetic predisposition.
Acoustic Neuroma (Vestibular Schwannoma): This is a benign tumor that arises from the Schwann cells that surround the vestibulocochlear nerve (also called the eighth cranial nerve). This nerve is responsible for hearing and balance. It develops within the inner ear, in the area where the vestibulocochlear nerve exits the brainstem.
Symptoms:
- Gradual Hearing Loss: Often the first symptom, typically affecting one ear.
- Tinnitus: A persistent ringing, buzzing, or other sound in the ear.
- Dizziness and Balance Problems: Can cause vertigo (spinning sensation) or difficulty with coordination and balance.
- Facial Numbness or Weakness: In some cases, as the tumor grows, it can compress the facial nerve, causing facial weakness or numbness.
Causes: The exact cause is unknown, but it is not related to exposure to loud noises or any other environmental factors. It may be linked to genetic predisposition in some cases.
Cholesteatoma: This is a non-cancerous, but destructive, growth that develops in the middle ear space, behind the eardrum. It is formed from skin cells that migrate into the middle ear, usually due to chronic ear infections or trauma. The middle ear space, often behind the eardrum.
Symptoms:
- Hearing Loss: Often the first symptom, can be conductive (problems with sound transmission) or sensorineural (damage to the inner ear).
- Ear Pain: Can be constant or intermittent, sometimes severe.
- Ear Discharge: Often foul-smelling, and may contain pus or blood.
- Recurrent Ear Infections: Cholesteatomas can contribute to chronic ear infections.
- Facial Nerve Paralysis: In rare cases, a large cholesteatoma can compress the facial nerve, causing facial weakness or paralysis.
Causes:
- Chronic Otitis Media (Ear Infections): Repeated ear infections can lead to a buildup of pressure in the middle ear, allowing skin cells to migrate behind the eardrum.
- Trauma: Injury to the eardrum, such as a blow to the head, can create a pocket where skin cells can grow.
Keloids: Overgrowth of scar tissue following an injury or ear piercing. Keloids are firm, rubbery, and often have a shiny, smooth surface. They can range in color from pink or red to dark brown or black.
- Symptoms: Raised, firm, and often itchy scars.
- Causes: Overproduction of collagen in response to injury.
2. Malignant (Cancerous) Tumors:
Squamous Cell Carcinoma: This is the most common type of skin cancer that can affect the external ear.
|
Chondrosarcoma: A rare, malignant tumor of cartilage that can occur in the ear.
- Symptoms: A painless mass, pain, hearing loss, facial nerve paralysis, and bone destruction.
- Causes: Unknown, but may be related to radiation exposure or genetic predisposition.
Signs and Symptoms:
- Outer Ear: Scaly patches, pearly white lumps, ulcers that bleed, changes in skin texture.
- Ear Canal: Lumps, hearing loss, ear pain, numbness, drainage.
- Inner Ear: Ear pain, dizziness, hearing loss, tinnitus (ringing in the ear), headache.
Causes of Ear Tumors:
- Sun Exposure: Prolonged and unprotected sun exposure significantly increases the risk of skin cancers in the ear.
- Genetic Predisposition: Certain genetic conditions can increase the risk of developing various types of ear tumors.
- Chronic Ear Infections: Repeated ear infections can potentially contribute to the development of some ear tumors, particularly squamous cell carcinoma.
- Age: Some types of ear tumors are more common in older individuals.
- Trauma: Ear injuries or trauma can increase the risk of certain types of tumors.
- Exposure to Loud Noises: Prolonged exposure to loud noises may increase the risk of certain types of tumors, particularly acoustic neuromas.
- Lifestyle Factors: Smoking and alcohol consumption can increase the risk of some ear tumors.
Investigations:
- Physical Examination: A thorough examination of the ear by a doctor is essential.
- Biopsy: A sample of tissue is taken for microscopic examination to determine the type of tumor.
- Imaging Studies: CT scans and MRI scans provide detailed images of the ear and surrounding structures to assess the extent of the tumor.
- Audiometry: Hearing tests are used to evaluate hearing loss.
- Facial Nerve Testing: Testing is done to assess facial nerve function, which can be affected by some ear tumors.
Treatment:
- Surgery: Surgical removal of the tumor is the most common treatment for benign and malignant ear tumors.
- Radiation Therapy: Used to shrink or destroy tumors, especially when surgery is not possible or to prevent recurrence.
- Chemotherapy: May be used to treat widespread or advanced ear tumors.
- Targeted Therapy: Newer therapies that target specific proteins or pathways in tumor cells are being developed and may become more common.
Prevention:
- Sun Protection: Protect your ears from prolonged sun exposure by wearing a hat, sunglasses, and sunscreen with a high SPF.
- Ear Hygiene: Practice good ear hygiene to prevent infections.
- Hearing Protection: Wear earplugs or protective headphones when exposed to loud noises.
- Regular Checkups: Schedule regular checkups with a doctor to detect potential ear tumors early.
NOSE
1. External Nose: The external nose includes the nasal bones and cartilages covered by skin.
- It helps in filtering, warming, and moistening inhaled air.
2. Nasal Cavity: The nasal cavity is a hollow space behind the external nose that extends from the nostrils to the back of the throat (nasopharynx).
- It is lined with mucous membranes and contains the nasal septum (dividing the cavity into left and right sides), nasal turbinates (bony structures that increase the surface area and help with air filtration), and openings to the paranasal sinuses.
- At the entrance, Little’s area (also known as Kiesselbach’s plexus) is found on the anterior nasal septum, where epistaxis usually originates because of its vascular delicate structure.
3. Paranasal Sinuses: There are four pairs of paranasal sinuses: frontal, ethmoid, sphenoid, and maxillary sinuses.
- These air-filled cavities are connected to the nasal cavity and play a role in producing mucus, providing resonance to the voice, and reducing the weight of the skull bones.
Types of Tumors of the Nose:
Benign Tumors:
1. Nasal Polyps: Benign, soft, teardrop-shaped growths that develop in the nasal lining. These are not true tumors but rather an overgrowth of the tissue lining the nasal cavity.
Causes:
- Chronic inflammation due to allergies, sinusitis, aspirin sensitivity/drug sensitivity or immune disorders, cystic fibrosis, recurrent nasal sinus infections and other conditions.
Clinical Presentation:
- Nasal obstruction: Difficulty breathing through the nose, feeling like the nose is blocked.
- Anosmia/Loss of smell: Reduced or complete inability to smell.
- Postnasal drip: Mucus dripping down the back of the throat.
- Discharge: There may be nasal discharge which may be yellowish, mucoid or pus.
- Facial pain: Aching or pressure in the face, especially around the sinuses.
- Frequent headaches: Headaches that may be related to sinus pressure.
- Snoring: Loud breathing during sleep, often due to nasal obstruction.
- Sleep apnea: Pauses in breathing during sleep, which can be caused by obstruction.
- Facial pressure or fullness: A feeling of tightness or pressure in the face.
- Recurrent sinus infections: Frequent infections in the sinuses, often associated with inflammation.
- There may be signs and symptoms of allergy like Nasal congestion, runny nose/stuffy nose, sneezing, loss of taste or smell.
Diagnosis & Investigations:
- Physical examination: Through inspection of the nasal cavity and Grey freshly masses from nasal cavities which look like skinned grapes may be seen.
- Nasal endoscopy: A thin, flexible tube with a camera is inserted into the nose to visualize the polyps.
- CT scan or MRI: Imaging tests can show the size and location of the polyps and any associated sinus problems.
Management of Nasal Polpys:
Medical:
- Treat the cause: Addressing underlying conditions like allergies, sinusitis, or aspirin sensitivity.
- Antrum washout or antrostomy: Procedures to clear out the sinuses and improve drainage.
- Nasal corticosteroids: Reduce inflammation and shrink polyps. (e.g., betamethasone 50mg instilled twice daily into each nostril for 4 weeks, with the patient lying flat for 3 minutes after instillation).
- Antihistamines: Used to manage allergy-related inflammation.
- Saline irrigation: Using saline solution to flush out the nasal passages.
- Antibiotics: Prescribed for any bacterial infections.
Surgical:
Polypectomy: Removal of the polyps through surgery. This may be necessary if polyps are large, recurrent, or unresponsive to medical treatment.
Procedure:
- Local anesthesia: Spray lignocaine 2% into the nose and adrenaline 1:100,000, wait for 5 minutes.
- Open nostrils: Use a nasal speculum to open the nostrils under good lighting.
- Pass a polypectomy snare: Maneuver the snare to catch the polyp and remove its base.
- Repeat process: Repeat the procedure until all polyps are removed.
- Bleeding control: Pack the nose if excessive bleeding occurs.
General anesthesia: This may be used for more complex polypectomies or in cases where the patient is unable to tolerate local anesthesia.
Prevention:
- Avoiding triggers: Identifying and avoiding allergens and irritants, such as dust mites, pollen, smoke, and strong odors.
- Managing underlying conditions: Treating sinusitis, allergies, and other conditions that contribute to inflammation.
- Regular nasal hygiene: Using saline sprays, nasal irrigation, and other methods to keep the nasal passages clear.
2. Nasal Angiofibroma: Benign, vascular tumor that originates from the nasal cavity, most commonly in adolescent males. This tumor is made of blood vessels and connective tissue.
Causes: The exact cause is unknown, but hormonal influences are suspected. It may be related to puberty in males.
Clinical Presentation:
- Nasal obstruction: Difficulty breathing through the nose.
- Epistaxis (nosebleeds): Frequent and often heavy nosebleeds.
- Facial swelling: Swelling around the nose and face.
- Headache: Pain in the head, often caused by pressure from the tumor.
- Snoring: Loud breathing during sleep, often due to nasal obstruction.
- Sleep apnea: Pauses in breathing during sleep, which can be caused by obstruction.
- Difficulty breathing through the nose: Feeling like you can’t breathe comfortably through your nose.
- Repeated nosebleeds: Frequent and sometimes severe nosebleeds.
Diagnosis & Investigations:
- Physical examination: Inspect the nasal cavity
- Nasal endoscopy: A thin, flexible tube with a camera is inserted into the nose to visualize the tumor.
- CT scan or MRI: Imaging tests can show the size and location of the tumor.
- Haemogram: Blood tests
Management:
- Surgical: Removal of the tumor, often via an endoscopic approach.
- Radiation therapy: May be used as an adjunct to surgery or as a primary treatment in cases where surgery is not possible.
3. Nasal Papilloma: Benign, wart-like growth on the nasal lining, often caused by HPV (human papillomavirus). These are usually small but can grow larger.
Causes: HPV infection, specifically types 6 and 11.
Clinical Presentation:
- Nasal obstruction: Difficulty breathing through the nose.
- Epistaxis: Nosebleeds, which may be frequent or severe.
- Nasal discharge: Clear or white mucus coming from the nose.
- Smell disturbances: Reduced or complete inability to smell.
- Repeated nosebleeds: Frequent and sometimes severe nosebleeds.
- Postnasal drip: Mucus dripping down the back of the throat.
Diagnosis & Investigations:
- Physical examination: Visual inspection of the nasal cavity.
- Nasal endoscopy: A thin, flexible tube with a camera is inserted into the nose to visualize the papilloma.
- Biopsy: A small sample of the papilloma is taken for examination under a microscope to confirm the diagnosis.
General Management:
- Surgical: Removal of the papilloma, often with electrocautery or laser surgery.
- Antiviral medication: May be used for some types of HPV-related papillomas, but generally not as effective as surgery.
General Prevention:
- Avoiding exposure to HPV: This means practicing safe sexual practices and avoiding close contact with people who have HPV-related warts.
ADENOIDS AND ADENOIDITIS
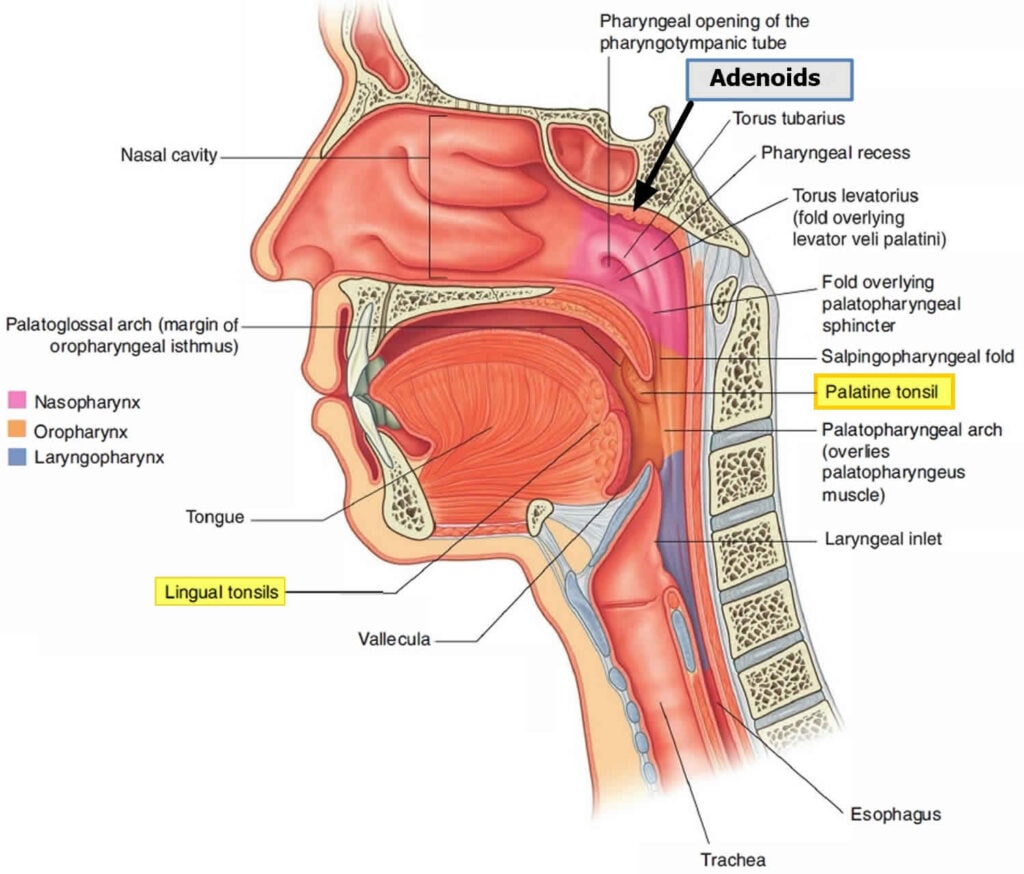
Adenoids, also known as pharyngeal tonsils, are lymphatic tissues located in the nasopharynx, the area at the back of the nose. Important in the immune system by trapping and destroying pathogens, particularly bacteria and viruses.
Adenoiditis is the inflammation and enlargement of the adenoids. This condition is common in children under 7 years old and often follows an episode of acute tonsillitis. The most frequent culprit behind adenoiditis is Group A beta-hemolytic streptococcus, the same bacteria often responsible for strep throat.
Symptoms of Adenoiditis:
- Nasal Obstruction: The enlarged adenoids block the nasal passages, leading to mouth breathing, difficulty breathing through the nose, and a stuffy feeling.
- Difficulty Eating: Pain caused by inflammation can make eating difficult, particularly for children.
- Snoring: Adenoid enlargement can obstruct the airway during sleep, resulting in noisy breathing and snoring.
- Jaw Deformities: Prolonged mouth breathing due to nasal obstruction can lead to changes in jaw development.
- Hearing Loss: The adenoids are located near the openings of the Eustachian tubes, which connect the middle ear to the back of the throat. Inflammation can block these tubes, leading to fluid buildup in the middle ear and hearing loss.
- Glue Ear: The accumulation of fluid in the middle ear behind the eardrum, known as glue ear, is a common consequence of adenoiditis.
- Recurrent Cough: Adenoiditis can trigger a persistent cough, often accompanied by drainage.
- Discharging Cough: Mucus from the inflamed adenoids can drain down the throat, causing a post-nasal drip and a cough with phlegm.
- Sleep Apnea: In severe cases of adenoid hypertrophy, the enlarged adenoids can completely block the airway during sleep, leading to episodes of apnea, where breathing temporarily stops.
Diagnosis of Adenoiditis:
- History and Physical examination: The diagnosis of adenoiditis relies on a thorough medical history and physical examination. A careful assessment of the patient’s symptoms and examination of the throat can reveal the presence of enlarged adenoids.
- Imaging: In some cases, imaging tests may be necessary to confirm the diagnosis and assess the severity of the adenoid enlargement. X-rays of the neck soft tissue, particularly a lateral view, can demonstrate narrowing of the nasopharynx due to enlarged adenoids.
Management of Adenoiditis:
The approach to managing adenoiditis depends on the severity of the symptoms and the patient’s age.
Mild Cases: If symptoms are mild and not significantly impacting daily life, conservative treatment may be sufficient. This includes:
Antihistamines: Chlorphenamine, an antihistamine, can help reduce inflammation and congestion. The dosage is 4 mg orally t.d.s, adjusted according to age, for a period of 7 days.
Topical Nasal Steroids: Nasal sprays containing corticosteroids like betamethasone can effectively reduce inflammation and improve nasal breathing.
- Underlying Infection: If an underlying bacterial infection is suspected, antibiotics may be prescribed. Ampicillin, a common antibiotic, is often used at a dosage of 500mg-1g every 6 hours.
- Pain Management: Pain relief can be achieved with analgesics like paracetamol (PCT) 500mg-1g three times a day or tramadol 75 mg for severe pain.
- Mouth Care: Encouraging good oral hygiene practices, such as regular brushing and flossing, can help prevent secondary infections and promote healing.
- Surgery (Adenoidectomy): If conservative treatment fails to alleviate symptoms, or if the adenoids significantly obstruct breathing or cause recurrent ear infections, surgery may be recommended. Adenoidectomy, the surgical removal of the adenoids, is typically performed after the age of one year.
Note: Adenoids usually shrink as a child grows older, so surgery is considered as a last resort.
Complications of Adenoiditis:
While adenoiditis is usually a temporary condition, it can lead to complications if left untreated:
- Otitis Media (Ear Infection): Blocked Eustachian tubes can result in recurrent ear infections.
- Recurrent Infections: Persistent inflammation can increase susceptibility to repeated infections, particularly in the respiratory system.
- Quinsy (Peritonsillar Abscess): A rare complication where an abscess forms around the tonsils, requiring drainage.
- Mastoiditis: In severe cases, infection can spread to the mastoid bone behind the ear, causing mastoiditis.
Cancerous Tumors:
4. Nasal Carcinoma/Sinus Cancer: Malignant tumor arising from the nasal lining, usually squamous cell carcinoma. This is a serious condition that can spread to other parts of the body if left untreated.
Causes: Exposure to tobacco smoke, industrial chemicals, radiation, and certain viruses (including HPV) are all risk factors.
Clinical Presentation:
- Nasal obstruction: Difficulty breathing through the nose.
- Epistaxis: Nosebleeds, which may be frequent or severe.
- Facial pain: Pain in the face, often related to pressure from the tumor.
- Nasal discharge: Mucus coming from the nose, which may be thick, bloody, or foul-smelling.
- Loss of smell: Reduced or complete inability to smell.
- Facial swelling: Swelling around the nose and face.
- Headache: Pain in the head, often caused by pressure from the tumor.
- Sinus pain: Pain and pressure in the sinuses.
- Facial pressure or fullness: A feeling of tightness or pressure in the face.
- Pain in the teeth: Pain in the teeth, especially the upper teeth.
- Loss of teeth: Loss of teeth due to tumor growth or pressure.
- Weight loss: Unexplained weight loss, which can be a sign of cancer.
- Fatigue: Feeling tired and weak.
- Neck mass: A lump in the neck, which can be a sign of cancer spreading to the lymph nodes.
General Diagnosis & Investigations:
- Physical examination: Visual inspection and examination of the nose, sinuses, and neck.
- Nasal endoscopy: A thin, flexible tube with a camera is inserted into the nose to visualize the tumor.
- Biopsy: A small sample of the tumor is taken for examination under a microscope to confirm the diagnosis.
- CT scan or MRI: Imaging tests can show the size, location, and spread of the tumor.
Management:
- Surgery: Removal of the tumor, often with radiation therapy or chemotherapy.
- Radiation therapy: May be used as primary treatment or as an adjunct to surgery.
- Chemotherapy: May be used to shrink the tumor before surgery or to treat advanced disease.
General Prevention:
- Avoiding tobacco use: The most important thing that can reduce the risk of nasal cancer.
- Limiting exposure to industrial chemicals: Wear appropriate safety gear when handling chemicals and avoid unnecessary exposure.
- Wearing appropriate safety gear: Wear protective gear such as respirators, masks, and gloves when exposed to hazardous materials.
- Regular dental check-ups: See your dentist regularly for check-ups and to identify any early signs of oral cancer, which can sometimes be related to nasal cancer.
THROAT:
a. Pharynx: The pharynx is a muscular tube located behind the nasal cavity and mouth.
- It is divided into three parts: nasopharynx (behind the nasal cavity), oropharynx (behind the mouth), and laryngopharynx (above the esophagus and larynx). The pharynx serves as a passage for both air and food.
b. Larynx: The larynx, commonly known as the voice box, is situated at the top of the trachea (windpipe).
- It houses the vocal cords, which are responsible for voice production. The larynx also helps protect the airway during swallowing by closing the epiglottis.
c. Tonsils and Adenoids: The tonsils (palatine tonsils) are located on each side of the back of the throat, while the adenoids (pharyngeal tonsils) are located in the upper part of the throat, behind the nose.
- They are part of the immune system and help fight infection.
Tumors of the Throat:
Benign Tumors:
1. Papilloma: A benign, wart-like growth that occurs on the mucous membrane of the throat, often caused by human papillomavirus (HPV).
Causes: HPV infection, especially types 6 and 11.
Clinical Presentation:
- Hoarseness: A change in voice quality, often described as raspy or rough.
- Dysphagia/Difficulty swallowing: A feeling of food getting stuck in the throat or discomfort when swallowing.
- Sore throat: A painful sensation in the throat that may be constant or intermittent.
- Cough: A dry or productive cough that may be persistent.
- Change in voice: A noticeable difference in how the voice sounds, such as hoarseness, breathiness, or a loss of vocal range.
- Sensation of something in the throat: A feeling of a lump or obstruction in the throat.
- Frequent throat clearing: A constant need to clear the throat to relieve a feeling of blockage.
- Dyspnea/Difficulty breathing: Shortness of breath, wheezing, or a feeling of being unable to take a full breath.
Diagnosis & Investigations:
- Physical examination: Visual assessment of the throat and neck for any visible signs of a papilloma.
- Laryngoscopy: A thin, flexible tube with a camera is inserted into the throat to visualize the papilloma.
- Biopsy: A small sample of the papilloma is taken for examination under a microscope to confirm the diagnosis and rule out cancer.
Management:
- Surgical: Removal of the papilloma using laser surgery, electrocautery, or cryosurgery. These procedures are usually minimally invasive and performed under local anesthesia.
- Antiviral medication: May be used for some types of HPV-related papillomas, but it is not always effective.
Prevention:
- Avoiding exposure to HPV: This involves practicing safe sexual practices, using condoms, and avoiding close contact with people who have HPV-related warts.
Cancerous Tumors:
2. Laryngeal Cancer: Malignant tumor arising from the larynx (voice box), usually squamous cell carcinoma.
Causes:
- Tobacco use (smoking and chewing): The most significant risk factor, both for developing and worsening laryngeal cancer.
- Heavy alcohol consumption: Increases the risk of developing laryngeal cancer, particularly when combined with tobacco use.
- Exposure to industrial chemicals: Certain chemicals like asbestos, formaldehyde, and nickel can increase the risk.
- HPV infection: Some types of HPV can contribute to the development of laryngeal cancer.
Clinical Presentation:
- Hoarseness: A persistent change in voice quality, often the first and most noticeable symptom.
- Difficulty swallowing: Pain or discomfort when swallowing, sometimes accompanied by a feeling of food getting stuck.
- Sore throat: A persistent sore throat, often described as scratchy or burning.
- Cough: A chronic or persistent cough that may be dry or produce phlegm.
- Neck pain: Pain in the neck, especially when swallowing or moving the head.
- Ear pain: Pain in the ear, often on the same side as the tumor.
- Difficulty breathing: Shortness of breath, wheezing, or a feeling of being unable to take a full breath.
- Fatigue: A feeling of persistent tiredness and weakness.
- Change in voice: Noticeable alteration in how the voice sounds, such as hoarseness, breathiness, or a loss of vocal range.
- Sensation of something in the throat: A feeling of a lump or obstruction in the throat.
- Frequent throat clearing: A constant need to clear the throat to relieve a feeling of blockage.
- Pain when swallowing: Discomfort or pain when swallowing food or liquids.
- Difficulty breathing: Shortness of breath, wheezing, or a feeling of being unable to take a full breath.
- Neck mass: A lump or swelling in the neck, often on one side.
- Loss of appetite: A decrease in appetite or a feeling of fullness quickly after eating.
- Unexplained weight loss: Significant weight loss without trying to lose weight.
- Chronic cough: A persistent cough that lasts for weeks or months.
Diagnosis & Investigations:
- Physical examination: Examination of the throat and neck for any visible signs of a tumor.
- Laryngoscopy: A thin, flexible tube with a camera is inserted into the throat to visualize the tumor.
- Biopsy: A small sample of the tumor is taken for examination under a microscope to confirm the diagnosis and determine the type of cancer.
- Imaging studies (CT scan, MRI, PET scan): These scans provide detailed images of the tumor and its location, helping to assess its size and spread. A positron emission tomography (PET) scan is a type of imaging test. It uses a radioactive substance called a tracer to look for disease in the body.
Management:
- Surgery: Removal of the tumor, often with radiation therapy or chemotherapy, depending on the stage and location of the cancer.
- Radiation therapy: May be used as primary treatment or as an adjunct to surgery to destroy any remaining cancer cells.
- Chemotherapy: May be used to shrink the tumor before surgery or to treat advanced disease that has spread to other parts of the body.
Prevention:
- Avoiding tobacco use: This is the most important step to reduce the risk of laryngeal cancer.
- Limiting alcohol consumption: Moderate alcohol consumption can reduce the risk, but heavy drinking significantly increases it.
- Avoiding exposure to industrial chemicals: Wear appropriate protective gear when handling hazardous substances.
- Receiving the HPV vaccine: Vaccination can help protect against certain types of HPV that can contribute to laryngeal cancer.
3. Pharyngeal Cancer/Throat cancer: Malignant tumor arising from the pharynx (throat), commonly squamous cell carcinoma.
Causes:
- Tobacco use (smoking and chewing): The primary risk factor.
- Heavy alcohol consumption: Increases the risk, particularly when combined with tobacco use.
- Exposure to industrial chemicals: Certain chemicals can increase the risk.
- HPV infection: Some types of HPV can contribute to the development of pharyngeal cancer which can be obtained through oral sex.
Clinical Presentation:
- Difficulty swallowing: Pain or discomfort when swallowing, sometimes accompanied by a feeling of food getting stuck.
- Sore throat: A persistent sore throat, often described as scratchy or burning.
- Ear pain: Pain in the ear, often on the same side as the tumor.
- Neck pain: Pain in the neck, especially when swallowing or moving the head.
- Hoarseness: A change in voice quality, often described as raspy or rough.
- Nasal obstruction: Difficulty breathing through the nose.
- Weight loss: Unexplained weight loss without dietary changes.
- Fatigue: A feeling of persistent tiredness and weakness.
- Sensation of something in the throat: A feeling of a lump or obstruction in the throat.
- Frequent throat clearing: A constant need to clear the throat to relieve a feeling of blockage.
- Earache: Pain in the ear, often on the same side as the tumor.
- Neck mass: A lump or swelling in the neck, often on one side.
- Chronic cough: A persistent cough that lasts for weeks or months.
Diagnosis & Investigations:
- Physical examination: Examine the throat and neck for any visible signs of a tumor.
- Laryngoscopy: A thin, flexible tube with a camera is inserted into the throat to visualize the tumor.
- Biopsy: A small sample of the tumor is taken for examination under a microscope to confirm the diagnosis and determine the type of cancer.
- Imaging studies (CT scan, MRI, PET scan): These scans provide detailed images of the tumor and its location, helping to assess its size and spread.
Management:
- Surgery: Removal of the tumor, often with radiation therapy or chemotherapy, depending on the stage and location of the cancer.
- Radiation therapy: May be used as primary treatment or as an adjunct to surgery to destroy any remaining cancer cells.
- Chemotherapy: May be used to shrink the tumor before surgery or to treat advanced disease that has spread to other parts of the body.
Prevention:
- Avoiding tobacco use: This is the most important step to reduce the risk of pharyngeal cancer.
- Limiting alcohol consumption: Moderate alcohol consumption can reduce the risk, but heavy drinking significantly increases it.
- Avoiding exposure to industrial chemicals: Wear appropriate protective gear when handling hazardous substances.
- Receiving the HPV vaccine: Vaccination can help protect against certain types of HPV that can contribute to pharyngeal cancer.
- Avoid Oral sex: Avoid engaging in oral sexual intercourse.
ADENOID HYPERTROPHY
Adenoid hypertrophy is a condition characterized by enlarged adenoids, a collection of lymphatic tissue located at the back of the nasal cavity.
This enlargement can lead to nasal obstruction, impacting breathing, sleep, and overall well-being.
Adenoids and Their Function
- The adenoids, also known as the pharyngeal tonsils, are part of the body’s immune system, acting as a first line of defense against infections.
- They are usually larger in children, playing a role in protecting them from respiratory infections.
- By the age of five, adenoids usually begin to shrink, becoming less prominent in the immune system’s function.

The adenoids are small masses of lymphatic tissue located in the upper airway, between the nose and the back of the throat. Along with the tonsils, the adenoids form part of the lymphatic system, which works to defend the body against microbes, absorb nutrients, maintain proper fluid levels, and eliminate certain waste products. The anatomical position of the adenoids allows them to help fight infection by preventing germs from entering the body through the mouth or nose.
Causes of Adenoid Hypertrophy
Adenoid enlargement can be attributed to various factors, including:
- Infections: Viral infections, such as Epstein-Barr virus, and bacterial infections, like group A Streptococcus, can trigger inflammation and swelling of the adenoids.
- Chronic Inflammation: Repeated acute infections or persistent infections can lead to chronic adenoid inflammation, resulting in hypertrophy.
- Allergies and Irritants: Allergens or irritants, when exposed to the adenoid tissue, can trigger an inflammatory response, causing enlargement.
- Gastroesophageal Reflux (GERD): Stomach acid refluxing into the esophagus can irritate the adenoid tissue, leading to inflammation and hypertrophy.
- Bacterial Infections: Several aerobic bacterial species have been implicated in adenoid hypertrophy, including:
- Alpha-, beta-, and gamma-hemolytic Streptococcus species
- Hemophilus influenzae
- Moraxella catarrhalis
- Staphylococcus aureus
- Neisseria gonorrhoeae
- Corynebacterium diphtheriae
- Chlamydophila pneumoniae
- Mycoplasma pneumoniae
Classifying Adenoid Hypertrophy
Adenoid hypertrophy can be classified based on its anatomical relationship with adjacent structures:
- Grade 1: No contact between adenoid tissue and vomer, soft palate, or torus tubaris.
- Grade 2: Adenoid tissue contacts the torus tubaris.
- Grade 3: Adenoid tissue contacts the torus tubaris and vomer.
- Grade 4: Adenoid tissue contacts the torus tubaris, vomer, and soft palate in resting position.
Additionally, adenoid hypertrophy can be classified based on its size in relation to surrounding tissues:
- Grade 1: Adenoid occupies less than 25% of the choanal area.
- Grade 2: Adenoid occupies 25-50% of the choanal area.
- Grade 3: Adenoid occupies 50-75% of the choanal area.
- Grade 4: Adenoid occupies 75-100% of the choanal area.

Clinical Features of Adenoid Hypertrophy
The symptoms of adenoid hypertrophy can vary depending on the severity of the condition. Common signs include:
- Nasal Obstruction: Difficulty breathing through the nose, leading to mouth breathing.
- Mouth Breathing: Dry lips and bad breath due to continuous breathing through the mouth.
- Nasal Congestion: Feeling like the nose is pinched or stuffed.
- Frequent Sinus Symptoms: Recurrent sinus infections, headaches, and facial pain.
- Snoring: Loud snoring, especially during sleep.
- Sleep Apnea: Restless sleep, frequent awakenings, and potentially obstructive sleep apnea.
Diagnosis of Adenoid Hypertrophy
- Physical Examination: Examine the nose and throat for signs of adenoid enlargement.
- Lateral Neck X-Ray: An X-ray of the neck can help visualize the size and shape of the adenoids.
- Palpation: Gently feeling the adenoids through the roof of the mouth.
- Nasal Endoscopy: A thin, flexible tube with a camera is inserted into the nose to visualize the adenoids.
- Transnasal Endoscopy: An otolaryngologist (ENT doctor) performs this procedure for a definitive diagnosis.
Management of Adenoid Hypertrophy
Treatment for adenoid hypertrophy depends on the severity of the symptoms:
Minimal Symptoms: No treatment may be needed.
Mild to Moderate Symptoms:
- Nasal Sprays: Saline or steroid nasal sprays can help reduce swelling and improve breathing.
- Antibiotics: If the condition is caused by a bacterial infection, antibiotics may be prescribed.
Severe Symptoms:
- Adenoidectomy: Surgical removal of the adenoids may be recommended if conservative measures are ineffective.
Complications of Adenoid Hypertrophy
If left untreated, adenoid hypertrophy can lead to various complications:
- Obstructive Sleep Apnea (OSA): Enlarged adenoids can block the airway during sleep, leading to frequent awakenings, daytime sleepiness, and other health issues.
- Chronic Otitis Media: The hypertrophied adenoids can block the Eustachian tube, leading to recurrent ear infections and fluid buildup in the middle ear.
- Recurrent Sinus Infections: Obstruction of the nasal passages can lead to frequent sinus infections.
- Mouth Breathing and Dental Issues: Continuous mouth breathing can cause dry mouth, bad breath, and dental malocclusions over time.
- Speech and Swallowing Problems: Enlarged adenoids can interfere with speech and swallowing, potentially causing nasal speech and difficulty swallowing.
- Failure to Thrive: In severe cases, the obstruction can lead to poor weight gain and growth in children.
Post-operative Care for Adenoidectomy
After surgery to remove the adenoids, nurses play a vital role in providing comprehensive care:
- Pain Management: Administering pain medication and providing comfort measures.
- Hydration and Nutrition: Encouraging fluid intake and offering soft, easy-to-swallow foods.
- Monitoring for Complications: Observing for signs of bleeding, infection, and respiratory distress.
- Rest and Recovery: Advise on adequate rest and gradual return to normal activities.


Helpful, precised
Am requesting for the common tumors of fhthe ear and their management, please
1. Acoustic Neuroma (Vestibular Schwannoma):
– Definition: A benign tumor that arises from the Schwann cells of the vestibular nerve, which connects the inner ear to the brain.
– Real-Life Example: Imagine a small benign growth pressing on a telephone line, disrupting the transmission of signals.
– Management: Treatment options include observation, surgical removal, or radiation therapy, depending on the tumor’s size, symptoms, and patient’s preference.
2. Glomus Tumor:
– Definition: A benign tumor that originates from the glomus bodies, which are responsible for regulating blood flow in the ear.
– Real-Life Example: Think of a small cluster of blood vessels growing within a pipe, potentially affecting the flow of water.
– Management: Surgical excision is the primary treatment, although embolization (blocking blood supply) or radiation therapy may be considered in certain cases.
3. Squamous Cell Carcinoma:
– Definition: A malignant tumor that arises from the skin cells lining the ear canal.
– Real-Life Example: Similar to skin cancer that can develop from excessive sun exposure on the face or body.
– Management: Treatment typically involves surgical removal of the tumor, followed by possible radiation therapy or chemotherapy, depending on the extent of the disease.
4. Basal Cell Carcinoma:
– Definition: A common type of skin cancer that can occur in the ear, originating from the basal cells of the epidermis.
– Real-Life Example: Like skin cancer that can develop from prolonged exposure to harmful ultraviolet (UV) rays.
– Management: Surgical excision is the primary treatment, and in some cases, radiation therapy or topical chemotherapy creams may be used.
5. Cholesteatoma:
– Definition: An abnormal collection of skin cells that accumulate in the middle ear, often due to chronic ear infections or eustachian tube dysfunction.
– Real-Life Example: Imagine a pocket forming within a pipe due to debris accumulation, potentially causing blockage or damage.
– Management: Surgical removal of the cholesteatoma is necessary to prevent complications, followed by appropriate ear care and treatment of underlying causes.
6. Paraganglioma:
– Definition: A rare tumor that originates from the paraganglia, specialized cells involved in regulating blood pressure and blood flow.
– Real-Life Example: Similar to a growth affecting the nerves responsible for controlling blood pressure in specific areas of the body.
– Management: Treatment options include surgical removal, radiation therapy, or embolization, depending on the tumor’s location, size, and symptoms.
Thanks for the notes
Thanks for the best notes
You are welcome, anything you would like us to improve?
Please include also pathophysiology in these conditions
Complications and nursing considerations for a patient with adenoid hypertrophy
Thank you for this
Nursing Care plan for this patients
Thanks so much, am requesting for a priority Nursing diagnosis for patients with adenoid hypertrophy
Ineffective Airway Clearance related to obstruction of the airway by enlarged adenoids
Thanks so much for the notes am really grateful the notes are well explained for every student to understand
Im requesting for the tumors affection ENT and their management thank you
Good notes, just request that you summarize more
Well understood the notes
Very interesting