Table of Contents
ToggleLevels of disease prevention
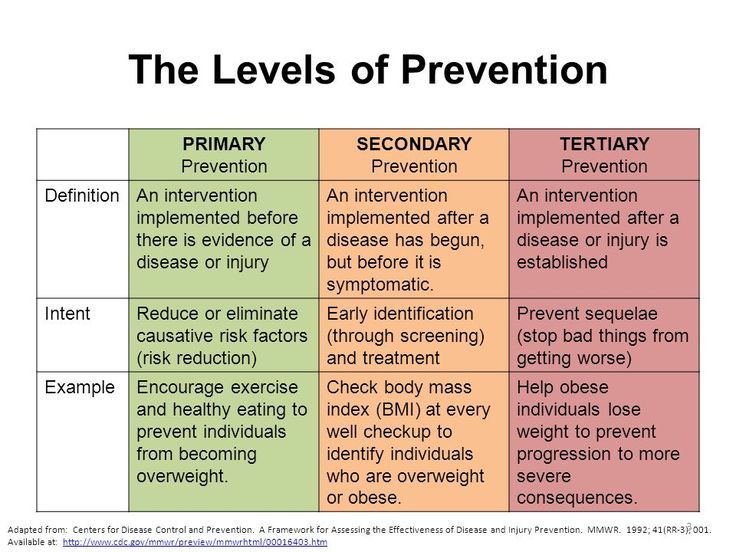
Primary (1°) prevention
- Is prevention that proceeds disease or days function and is applied to patients considered physically and emotionally healthy.
- It is aimed at intervention before pathological diseases have begun during the stage of susceptibility.
- It includes activities that are directed at using the probability of specific illness or body function.
- 1° prevention includes both general health promotions and specific protection.
General health promotions include e.g.
- Health education
- Good standard of nutrition adjusted to developmental stages of life.
- Attention to personality development.
- Provision of adequate housing and recreation and agreeable working conditions.
- Genetic screening
- Marriage and sex education
- Periodic selective examination.
Specific Protection refers to measures aimed at protecting individual against specific agents e.g. immunization,
- Vaccination
- Attention to personal hygiene for self-care.
- Use of environment sanitation e.g. chlorination of well
- Protection from accidents e.g. Wearing helmets.
- Use of specific nutrients
- Protection or avoidance of allergens
- Protection from carcinogens.
Any particular disease or health problem is a result of intervention between a number of specific or associated risks that can be classified as Agent; Host and Environmental factors.
The interaction can be understood by visualizing the concepts or positive health and disease.
Secondary prevention (2°)
Focuses on the individuals who are experiencing health problems or illness and who are at risk for developing conditions or worsening conditions.
Its efforts seek to detect disease early and treat if promptly.
The goal is to cure the disease at the earliest stage when cure is impossible to slow its progression as well as prevent conditions of limit disability.
The activities directed at:-
- Case finding measures, individual and mass
- screening surveys
- Selective Exam
- Cure and prevention of disease process to prevent spread of communicable disease, prevent conditions and short the period of disability.
- Adequate TX to arrest disease process with prevents conditions.
- Provision of facilities to limit disability and prevent death.
Tertiary (3°) prevention
Occurs when the defect or disability is permanent.
It includes limitations of rehabilitation for those persons who have already experienced residual damage.
Tertiary prevention activities focus on the middle to latter phases of clinical disease.
When irreversible pathological damage produces disability (e.g. smoke exercise). Here the activities of restoration and rehabilitation will include:-
- Provision of hospital and community facilities for training and education to maximize use of remaining capacities.
- Education of the public and industries to use rehabilitated –
- Mother and father Meoble extent.
- Selective placement
- Work therapy and hospital
In 3° prevention, mainly the activities are directed at rehabilitation rather than diagnoses and treatment. Case at this level aims to help the patient to achieve a high level of functioning as possible despite the limitation caused by illness or impaired functions.
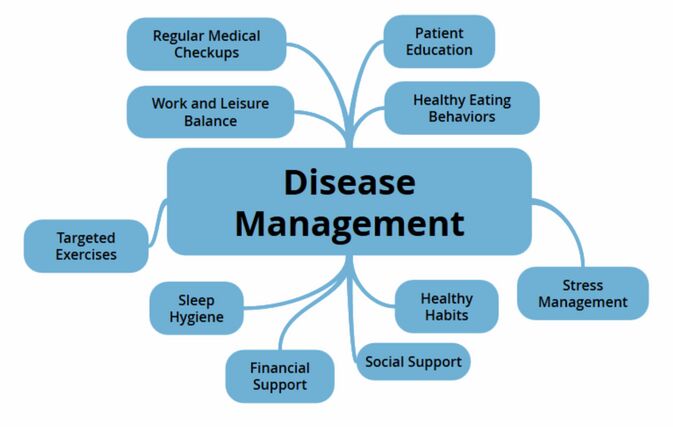
Management of diseases
Clinical diagnostic principles and treatment:
- History taking and recording
- Physical examination
- Tests and studies
- Treatment which involves first aid, nursing care, medical treatment, surgical treatment, preventive treatment/health education/discharge advice.
History taking and recording
This is the process of gathering information concerning the patient’s health problem as he arrives from home to the hospital.
Factors to be considered before history taking are commenced:
- The clinician/nurse taking history should be understood by the patient in order for a good problem account to be taken and recorded.
- The language to be used in history taking should be simple, clear and understandable to the patient.
- Where the interpreter is involved, the patient should be given time to express him or herself.
- The interviewer should not as far as possible ask questions which do not have definite answers and the questions should be related to the suspected disease which may lead to the diagnosis but not off topic questions.
- The interviewer should not just stop at presenting complaint and assumes that that is all for the history but should go deeper than that since the presenting complaint may just be only a small part of the problem.
- The history should be taken from the right source, i.e., the patient her self, close family member who has been with the patient since the illness started or a mother in case of a child, or from the incident report from the first aider/health centre/ those who found the patient and helped him to reach the hospital.
- Allow the patient to present the complaints in the way he/she feels it and only fill in the necessary information which should include whatever has been disclosed concerning the patient and his/her attitudes.
- There must be privacy during history collection to avoid concealing more otherwise vital information that could have helped in the diagnosis.
- The history should be detailed, clear and chronological with significant information. It should include the interpretation of the present situation and should indicate the result they expect from consultation.
- History taking should be done is such a way that the patient/attendant learns from the interview so that he is made to discover what could have gone wrong such that the illness has occurred.
Physical examination
Introduction
Physical examination can be done through inspection, palpation, percussion and auscultation and this may need a stretcher or just the laps of the mother for the case of a small child/a baby.
- Inspection: this is the act of visually observing the patient to note any significant physical change.
- Palpation: this is the use of sense of touch to assess factors such as texture, crepitance, temperature, moisture, vibration or pulsation, swelling, rigidity or spasticity, organ location and size, presence of lumps or masses, and presence of tenderness or pain. Different parts of the hands are used for palpation.
- Percussion: this is striking the patient’s skin to determine the density, size and location of the underlying structure. A tap on the skin sets the body wall in motion: and the quality of sound produced describes the organ below, i.e. the density of air versus solid matter of the different structures. The sounds of the different notes on the percussed areas may either be of normal clear, hollow quality, low pitched one, or much lower & louder in the lung areas where there is much air, or it may be dull: soft, high-pitched, muffled thud over the spleen and liver. The sound may be absolutely dull/flat sound where there is no air especially over the thigh muscles or large tumors.
- Auscultation: this is used to assess sounds produced by the heart, lungs, and bowel. Abnormalities can be detected as different sounds are interpreted and compared to the normal sounds produced by the above organs.
General principles of Inspection
- Approaching the patient: whenever possible, ample time is allowed for the examiner and the patient to become acquainted. Patient should be treated as an individual with respect and dignity. The beliefs and other values should be considered. Encourage a good examiner-client relationship.
- Observations/inspection: this starts at the time the patient is entering the examination room/screen/hospital ward. The purpose is to note any significant physical characteristics. It is the point-specific scrutiny of the patient as a whole/system by system. It must be purposeful, focused, and unhurried.
- First observe the movement/gait and the way he/she is coming or being brought in, i.e., walking straight/limping/supported/rolled on a wheel chair/or on a stretcher. This tells you about how weak the patient is/how severe his condition is and the type of treatment/action he/she needs.
- Observe general appearance: is the face sad/sick looking, crying in deep pain/grimacing or vise versa.
- Carry out ABC plan of assessment: but you should be careful for your own safety before starting the assessment.
- Respiration: check if the breathing is normal/dyspnoiec and respiratory characteristics
- Dehydration, malnutrition and anemia: skin turgor/wrinkles, hollow cheek and jutting prominences, thirst, presence of secretions-saliva, urine, history of vomiting/diarrhea/bleeding/not eating and drinking for sometimes?
- Check for mental outlook: consciousness, confusion and hallucinations, alertness, orientation or unconsciousness. Observe the head for injuries, bleeding, and swelling. Do the same for the eyes, nose and ears, also the pupils for the size and their reaction to light.
- Smell for: breathe in case of alcohol/poisonous intake/acetone smell especially in patients who are unconscious.
- Take the vital signs: temperature, pulse, respiration, blood pressure and weight
- Look for muscle: for weakness, paralysis and spasms.
Process of examination
- Undressing: the majority of patients resent the removal of clothes even for examination purposes, i.e., the bras, pants and knickers. Most females look shy. The reason for clothe removal must be explained to the patient and confidentiality be ensured. The patient should then be told to lie on the stretcher in an anatomical position.
- Examination: usually it is better to start with an area unlikely to be having pain or a site of a patient’s complaints. The ears, eyes throat should be last in children. Before performing a disagreeable painful or embarrassing examination, tell the patient what is likely to happen and how the patient can assist, tell him that the examination is necessary and it will be performed as fast as possible and that during examination, some specimen has to be taken like vaginal smears.
Order of examination
Head
- Check the hair for quantity, thickness, texture, distribution, infestation. The texture is very important when conditions like hyper/hypothyroidism, or HIV/AIDS/chronic wasting diseases that cause protein loss, drugs, or alopecia are implicated.
- Check the scalp for scaliness, parasites, lumps, lesions, and nits. Note also the skin color, cyanosis, pallor in the face, jaundice, and mucous membrane, and edema.
- Observe the general size and contour of the skull and note any deformity, lumps and tenderness especially when checking for hydrocephalus, microcephalus or acromegally. Check for facial expression, symmetry of the facial structures (stroke and hypertension).
- Eyes: ask if patient is able to see/has blurred vision esp. in hypertension and diabetes mellitus. Also look for photophobia, visual acuity (for long/short sightedness), any swelling, discharge, wounds, eye size, check pupil size and their reaction to light esp. in unconscious patients or those with injuries on the head.
- Ears: for size, skin lesions, swelling, tenderness and pain on the pinna. Look for redness, wounds in the middle ear and discharge (note the color whether bloody, purulent, serous, etc) for they have different indications.
- Nose: check for any deformity, asymmetry, inflammation, wounds, discharge, patency of each nostril, smelling test.
- Mouth and throat: inspect the lips for color, moisture, lumps, ulcers, cracking. Certain diseases affect the lips including dehydration. Note the color of the mucous membrane in the tongue, smoothness (for the dorsal surface of the tongue is normally roughened from the presence of papillae), check for rashes and fungal infections, sores and wounds. Check the gum for swelling; bleeding, discoloration, retraction, etc. check the throat for the swellings of thyroid glands, salivary glands, range of movement and strength of cervical bones and muscles.
Thoracic cavity
- On inspection, look for shape (barrel chest-horizontal ribs+ large antero-posterior diameter or scoliosis-an S-shaped curvature, lordosis/sway-back=an anterior curvature of the lumbar spine, and kyphosis-an exaggerated posterior curvature of the thoracic spine= hump back).
- Observe the skin and muscles to determine the level of nutrition.
- Check for any respiratory movement, wounds and penetrations.
- Note respiratory abnormalities such as dyspnoea, tachypnoeic, bradypnea, irregular, shallow, slow breathing, apnea, cheyne stoke’s breathing.
- Look for chest sounds by use of percussion and auscultation ( decreased and absent sounds occur in bronchial obstruction by foreign bodies, secretions, mucus plug), and percussion notes( resonance = normal, hyperresonace = emphysema, dull = abnormal density in the lungs caused by pneumonia, pleural effusion, Atelectasis or tumor).
- Do breast examination for size, dimples, nodules, sores, swelling, etc. Do also cardiovascular examination.
Abdomen by use of inspection, auscultation, percussion and palpation:
- Check the abdomen for distension, scars, rigidity, tenderness and pain, enlargement of the organs, ascites, skin turgor and folding. Nb: the abdomen is auscultated first after inspection and before percussion and palpation so that the auscultatory findings are not altered by increased or decreased peristalsis
- Pelvis: check it for position, size and proportion to detect any abnormality.
- Extremities (both lower and upper extremities): note the color, presence of clubbing of the fingers and toes in chronic illnesses, hair distribution, venous pattern, swellings, ulcers, temperature, palpate the blood supply to the extremities, check for range of movement abilities at the joints and observe for muscle strength, any deformity and inequality.
- Skin: check for color, texture, rashes, scales, desquamation, scars, swollen nodes, edema, sensation, temperature, wounds, etc.
Neurological examination
This involves assessing for the level of consciousness by calling him/her, shaking, shouting in the ears, pressing a nail bed for pain stimuli and see how he/she is responding, checking for papillary reaction to light and size, or by use of Glasgow coma scale, check for the senses of smell, taste, site, touch, muscle weakness, paralysis, reflexes, etc.
Investigations/tests & studies
Tests are procedures carried out from the laboratory to identify the pathogenic microbes while studies are investigations which need interpretation.
The types of tests that can be done in the laboratory include:
- Urine: this may be collected either in a sterile way to identify the microbes such as; E.coli, enterococci, staphylococci, hemolytic streptococci, mycobacterium tubercle, parasites such as schistosoma haematobium, trichomonas vaginalis, urea, Creatinine, etc. clean urine may also be collected to check for amount, color, consistency, specific gravity, glucose, albumin, pH, acetone, etc.
- Blood: this may be removed for various tests such as complete blood count, erythro-sedimentation rate, Hb, grouping and cross-match, smears, urea, renal and liver function tests, glucose, etc.
- Stool: this is removed to identify the ova, cysts, occult blood, mucus, microbes, worms, etc.
- Discharges: vaginal, urethral, cervical, pus, sputum, skin smears are taken for gram staining, etc.
- Punctures: this is when cavities are gone into and their secretions are aspirated and taken to the laboratories for analysis; e.g. thoracentesis, paracentesis, lumbar punctures, knee aspirations, etc.
Studies done to diagnose diseases include:
- Biopsies: this depends on the disease suspected and pieces of affected tissues are removed and taken for histological studies to identify the different cell types found in the tissue questioned especially if cancerous cells are suspected.
- Radiography: use of x-rays to detect any deformity/breakage in the bones; find abnormal lungs, distended loops of the gut, to show the size and shape of the heart.
- Ultra sound scan: use of sound waves emitted by the machine to produce an image of an anatomical structure which may either be normal/abnormal in size or structure.
- Endoscopies: this involves the insertion of tubes with light source at their tips and a viewing lens at the other side, into the tubular structures to view their walls for wounds, swellings, inflammations. These include: bronchoscopy, cystoscopy, endoscopy, etc.
- Use of radiopaque dyes: this is when radiopaque substances are injected into the tubular structures to coat up the walls of these organs so that when their radiograph is taken, blocked tubes, narrow ones are identified and actions are taken appropriately. These include: angiography, urography, venography, etc.
- Computerized tomography: a much more expensive method of imaging than the ultra sound scanning that can be used for more finely and diagnostic procedures for tumors especially in the brain where ultra sound scanning may not give any information that may be of help.
- Magnetic resonance imaging (MRI): use of magnetic waves to provide information about kidney masses that can not be obtained by other methods. Here solid masses look different from cystic/hollow masses which contain fluid in them.
Treatment of diseases
Principles of treatment of diseases
- First aid treatment: this is the kind of treatment offered especially for the patients who come to the hospital/health centers when they are badly off and their condition is deteriorating to the dying point within minutes. Assess for your own safety, carry out ABCDE plan of resuscitation and assessment, and refer the patient for further management.
- Nursing care: This care given to the patient without the use of drugs and it depends on the condition of the patient on arrival. Airway care is catered for first, then circulation (shock, anaemia, dehydration), and then others may follow. Nursing care involves preparing the patient, your self and equipment, doing the procedure, clearing and making the patient comfortable including records and patient follow up and continuous assessment and monitoring of the patient.
- Medical treatment: is the treatment of diseases using drugs. This may have been given during emergency before the doctor’s arrival and those that the doctor may prescribe before or after laboratory results.
- Surgical treatment: the use of mechanical means of operation to cure diseases in situations that drugs may not cure the patient.
- Preventive treatment: this involves prevention of infections through notification, isolation, health education and giving prophylactic drugs. Screening of contacts may be done and drugs given to the infected ones and you protect the health workers and other contacts.

Nurses revision has actually solved half my academic problem, l really don’t know how to appreciate because my words alone can’t describe it. Otherwise thanks for the love.