Table of Contents
ToggleLEUKEMIA
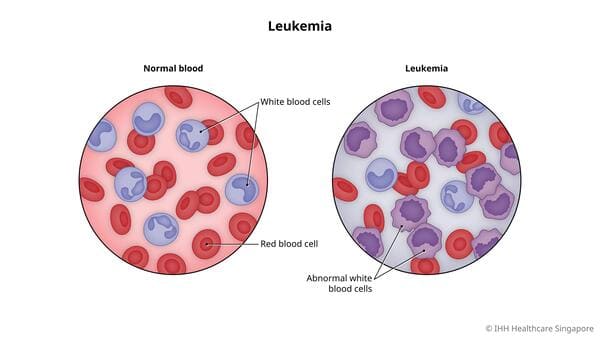
Definition: Leukemias are a group of hematologic disorders characterized by the dysfunctional proliferation and development of leukocytes. Leukemias are cancers of white blood cells or of cells that develop into white blood cells.
White blood cells develop from stem cells in the bone marrow. Sometimes the development goes awry, and pieces of chromosomes get rearranged. The resulting abnormal chromosomes interfere with normal control of cell division, so that affected cells multiply uncontrollably or are resistant to normal cell death, resulting in leukemia.
Types of Leukemia
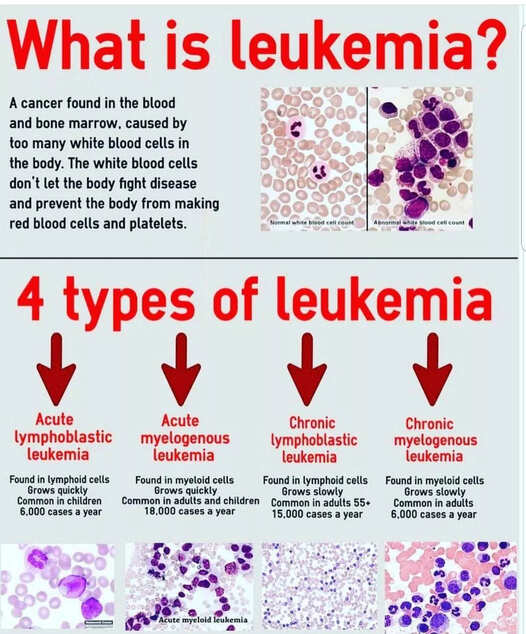
As such, the four major subtypes of leukemia are:
- Acute lymphoblastic leukemia (ALL): ALL occurs when primitive white blood cells of lymphoid origin reproduce without developing into normal B and T cells. It is the most common leukemia in pediatrics, accounting for up to 80% of cases in this group vs. 20% of cases in adults.
- Acute myelogenous leukemia (AML): AML is also characterized by the hyperplasia of blasts, but in this case, of myeloid origin. It accounts for half of the leukemia cases diagnosed in teenagers and people in their 20s. It is the most common acute leukemia in adults.
- Chronic lymphocytic leukemia (CLL): CLL occurs when mature but abnormal white blood cells of lymphoid origin undergo hyperplasia, leading to a monoclonal population of dysfunctional lymphocytes. Most cases occur in people between ages 60 and 70.
- Chronic myelogenous leukemia (CML): A monoclonal population of self-renewing, dysfunctional myeloid cells (e.g., neutrophils, basophils, eosinophils, macrophages) characterizes CML. Most cases occur in people between ages 25 and 60.
Note
- Acute vs. chronic: Acute leukemias are characterized by abnormal cells that are less mature, develop quickly, and leave the bone marrow as dysfunctional cells called “blasts.” These blasts crowd out healthy cells in the bone marrow, causing the rapid onset of symptoms. Blasts normally make up 1% to 5% of marrow cells, and having more than 20% blasts in the bone marrow is required for a diagnosis of acute leukemia. In contrast, chronic leukemias develop slowly and may take years to develop symptoms. They are composed primarily of more mature and functional cells, and there are generally not elevated numbers of blasts.
- Myeloid vs. lymphoid: Hematopoietic stem cells give rise to two types of blood cells: myeloid and lymphoid. Myeloid cells include monocytes, macrophages, neutrophils, basophils, eosinophils, erythrocytes, and megakaryocytes. Lymphoid cells include T cells, B cells, and natural killer cells. So myeloid leukemia affects myeloid cells and lymphoid leukemia affects lymphoid cells.
Causes of Leukemia
Several risk factors are associated with a higher risk of developing leukemia:
- Exposure to ionizing radiation is associated with an increased risk of multiple subtypes of leukemia.
- Exposure to benzene is a risk factor for leukemia in adults, particularly AML.
- Previous exposure to chemotherapy, especially alkylating agents and topoisomerase inhibitors, increases the risk for acute leukemia later in life.
- A history of any hematologic malignancy is a risk factor for subsequently developing another subtype of leukemia.
- Viral infections (e.g., human T-cell leukemia virus, Epstein Barr virus) are linked with subtypes of ALL.
- Several genetic syndromes (e.g., Down syndrome, Fanconi anemia, Bloom syndrome, Li-Fraumeni syndrome) are associated with an increased risk of AML and ALL.
Clinical manifestations
- Fever
- Lethargy
- Bone pain or tenderness
- Myalgia
- Malaise or generalised body weakness
- Moderate to severe infections which may be recurrent
- Unexplained or unintentional weight loss
- Recurrent nosebleeds
- Tendency to bleed or bruise easily
- Petechiae – tiny red spots on the skin
- Excessive sweating, especially at night (nocturnal hyperhidrosis)
- Chronic Fatigue
- On palpation, you may feel lymph node swelling and enlargement of the liver and spleen i.e. Hepatosplenomegaly
- When you auscultate the patient’s lungs, you may hear decreased breath sounds, shallow and rapid respirations, a rapid heart rate, and a systolic ejection murmur.
- Musculoskeletal symptoms (especially in the spine and long bones) can also be clues to the diagnosis.
- Shortness of breath,
- Symptoms related to thrombocytopenia, such as excessive bruising or heavy menstrual cycles.
NB: Chronic leukemia subtypes occur almost exclusively in adults. Many patients are asymptomatic at the time of diagnosis, identified only incidentally after:
- a) Marked leukocytosis is discovered on a CBC performed for another reason.
- b) Hepatosplenomegaly and lymphadenopathy can be appreciated in some cases while bleeding and bruising are less common, presenting features relative to acute leukemia subtypes.
Test and Diagnosis
- Medical history and physical exam,
- CBC and blood smear – peripheral WBC count varies widely from 1,000 to 100,000/mm3 and may include significant numbers of abnormal immature (blast) cells, anemia may be profound; platelet count may be abnormal and coagulopathies may exist.
- Bone marrow aspiration and biopsy – cells also studied for chromosomal abnormalities (cytogenetics) and immunologic markers to classify type of leukemia further.
- Lymph node biopsy – to detect the spread.
- Lumbar puncture and examination of cerebrospinal fluid for leukemic cells (especially ALL).
Management
Medical Management
- Chemotherapy – uses drugs to kill cancer cells. The most common chemotherapy protocols for leukemia may include combinations of anti-tumor antibiotics, vinca alkaloids, and other systemic anti-cancer therapy (SACT) medications.
- Targeted Therapy – uses drugs that attack specific abnormalities in the cancer cell
- Immunotherapy – utilizes the immune system to attack the leukemia cells; examples include immune system modulators and checkpoint inhibitors
- Radiotherapy. Radiotherapy uses radiation or high-powered energy beams such as protons and X-rays to kill the cancer cells. This can last from 3 days to 6 weeks.
- External beam radiation – aims the energy beams at the affected body area
- Brachytherapy – places radioactive material inside the body in order to perform radiation therapy
- Chimeric antigen receptor (CAR)-T Cell Therapy. This is a specialized treatment which involves the harvesting of the patient’s T-cells, engineering them to fight the leukemia cells, and infusing them back to the patient’s body.
- Bone Marrow Transplant. BMT is a procedure wherein the unhealthy bone marrow of the leukemia patient is removed and replaced by healthy stem cells which will cause a regeneration of healthy bone marrow to produce normal blood cells. It is also known as stem cell transplant.
Nursing interventions/management
1. Assessment of the patient
- a. Carrying out history of the presenting signs and symptoms e.g. fever, chronic fatigue, bleeding disorders among others.
- b. Taking vital observation e.g. TPR/BP and general examination to exclude other diseases
- c. Alerting the doctor who will order for investigations and admission, there the nurse will assist the patient throughout the process.
2. Managing fever (patient has 37.6 and above temperature, chills)
- a. Assess the patient’s vital signs at least every 4 hours.
- b. Remove excessive clothing, blankets, and linens. Adjust the room temperature.
- c. Administer and monitor the prescribed antibiotics and anti-pyretics.
- d. Assess the mental status of the patient because elevated temperatures can alter the function of the mind.
- e. Offer a tepid sponge bath.
- f. Elevate the head of the bed
3. To relieve acute pain
- a. Assess pain.
- b. Place patient at complete rest pain episode.
- c. Instruct patient to notify nurse immediately when pain occurs.
- d. Assess and document patient response to medication to provides information about disease progression and also aids in evaluating effectiveness of interventions, and may indicate need for change in therapeutic regimen.
- e. Identify precipitating event, if any: frequency, duration, intensity, and location of pain which will helps differentiate this chest pain, and aids in evaluating possible progression to unstable angina.
- f. Stay with patient who is experiencing pain or appears anxious to allay anxiety
- g. Maintain quiet, comfortable environment and also restrict visitors as necessary to prevent mental stress.
4. To manage fatigue
- a. Ask the patient to rate fatigue level (mild, moderate, or severe fatigue) to assess the patient’s activities of daily living, as well as actual and perceived limitations to physical activity inorder to create a baseline of activity levels, degree of fatigability, and mental status related to fatigue and activity intolerance.
- b. For patients with grade 3 fatigue (severe fatigue), consider discussing having a treatment break with the oncology team because anti-cancer therapies such as chemotherapy treatments may increase the fatigue levels in a cancer patient, disabling them to perform even the most basic daily activities such as eating and bathing. Having a treatment break may be needed to allow the patient to recuperate before receiving further doses.
- c. Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with rest and sleep to gradually increase the patient’s tolerance to physical activity.
- d. Teach deep breathing exercises and relaxation to allow the patient to relax while at rest. To allow enough
5. To maintain healthy normal weight (patients complains of anorexia, unexplained weight loss)
- a. Explore the patient’s daily nutritional intake and food habits (e.g., meal times, duration of each meal session, snacking, etc.) inorder to create a baseline of the patient’s nutritional status and preferences.
- b. Create a daily weight chart and a food and fluid chart. Discuss with the patient the short term and long-term nutrition and weight goals.
- c. Help the patient to select appropriate dietary choices to increase dietary fiber, caloric intake and alcohol and coffee intake inorder to promote nutrition and healthy food habits, as well as to boost the energy levels of the patient. Dietary fiber can help reduce stool transit time, thus promoting regular bowel movement.
- d. Refer the patient to the hematology/oncology dietitian to provide a more specialized care for the patient in terms of nutrition and diet in relation to newly diagnosed leukemia.
- e. Symptom control: Administer the prescribed medications for abdominal cramping and pain, such as anti spasmodics. Promote bowel emptying using laxatives as prescribed for constipation. On the other hand, provide advice on taking anti-diarrheal medications for diarrhea.
6. Preventing and Managing bleeding:
- a. Watch for signs of minor bleeding, such as petechiae, ecchymosis, conjunctival hemorrhage, epistaxis, bleeding gums, bleeding at puncture sites, vaginal spotting, and heavy menses.
- b. Be alert for signs of serious bleeding, such as headache with change in responsiveness, blurred vision, hemoptysis, hematemesis, melena, hypotension, tachycardia, dizziness.
- c. Test all urine, stool, emesis for gross and occult blood.
- d. Monitor platelet counts daily.
- e. Administer blood components as directed.
- f. Keep patient on bed rest during bleeding episodes.
7. Patient Education and Health Maintenance:
- a. Teach signs and symptoms of infection and advise whom to notify.
- b. Encourage adequate nutrition to prevent emaciation from chemotherapy.
- c. Teach avoidance of constipation with increased fluid and fiber, and good perineal care.
- d. Teach bleeding precautions.
- e. Encourage regular dental visits to detect and treat dental infections and disease.
8. Preventing infection: (due to lowered immunity)
- a. Frequently monitor the client for pneumonia, pharyngitis, esophagitis, perianal cellulitis, urinary tract infection, and cellulitis, which are common in leukemia and which carry significant morbidity and mortality.
- b. Monitor for fever, flushed appearance, chills, tachycardia; appearance of white patches in the mouth; redness, swelling, heat or pain in the eyes, ears, throat, skin, joints, abdomen, rectal and perineal areas; cough, changes in sputum; skin rash.
- c. Check results of granulocyte counts. Concentrations less than 500/mm3 put the patient at serious risk for infection.
- d. Avoid invasive procedures and trauma to skin or mucous membrane to prevent entry of microorganisms.
- e. Use the following rectal precautions to prevent infections: Avoid diarrhea and constipation, which can irritate the rectal mucosa, avoid the use of rectal thermometers, and keep perineal are clean.
- f. Care for the patient in private room with strict hand washing practice.
- g. Encourage and assist patient with personal hygiene, bathing, and oral care.
- h. Obtain cultures and administer antimicrobials promptly as directed.
Complications
Leukemia may cause several complications, which may include:
- Recurrent infections due to low levels of immunity
- Unintentional weight loss
- Anemia
- Bleeding problems
- Metabolic abnormalities – may lead to organ failure, particularly in the kidneys
- Central nervous system impairment
- Cataracts
- Infertility
- Increased risk of other types of cancer
- Mental health problems
- Poor quality of life
- Renal dysfunction
- Tumor lysis syndrome
- Nutritional depletion
- Mucositis