Table of Contents
ToggleLARYNGITIS
Introduction
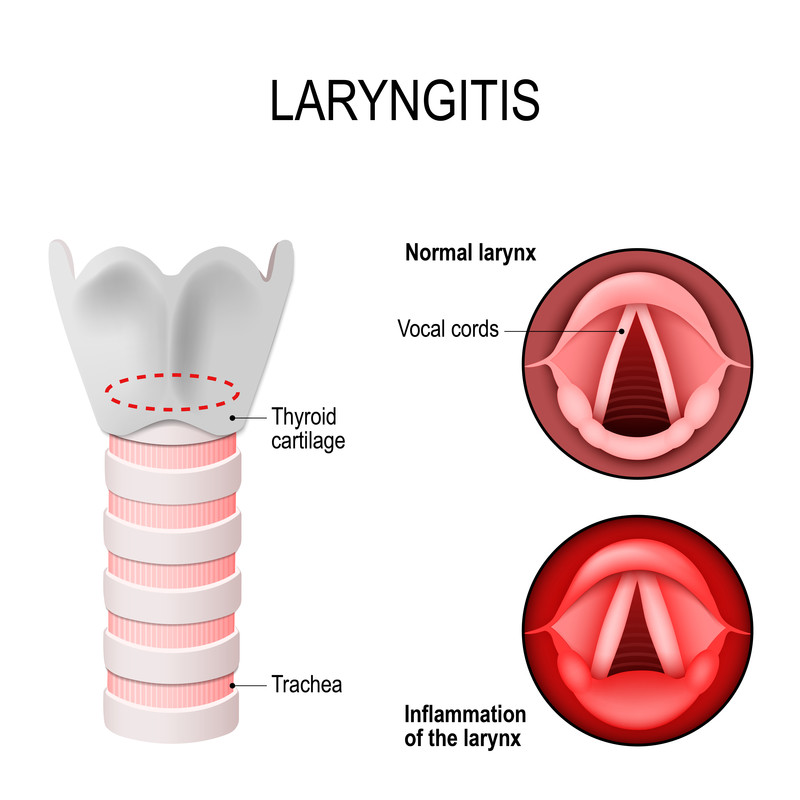
Laryngitis refers to inflammation of the larynx, commonly known as the voice box. The larynx contains the vocal cords, which vibrate to produce sound. When the vocal cords become inflamed or irritated, they swell, leading to a distorted voice or a complete loss of voice. It can present in both acute and chronic forms.
Types of Laryngitis
Laryngitis can be classified according to its duration:
- Acute Laryngitis: This is a common, often mild, and self-limiting condition that typically lasts for a period of 3 to 7 days, rarely exceeding two weeks. It usually has a sudden onset.
- Chronic Laryngitis: If laryngitis lasts for over 3 weeks, it is termed chronic laryngitis. This form of laryngitis is usually less severe but can be persistent and may indicate an underlying, ongoing irritant or medical condition.
Classification of Laryngitis according to cause
- Infectious Laryngitis: The cause is a pathogen, most commonly viruses, but sometimes bacteria or fungi.
- Non-infectious Laryngitis: Caused by non-pathogens such as vocal overuse, irritants (smoke, allergens), or conditions like gastroesophageal reflux disease (GERD).
Pathophysiology
The pathophysiology of laryngitis involves the inflammatory response of the laryngeal tissues, particularly the vocal cords.
- Acute laryngitis is characterized by inflammation and congestion of the larynx in the early stages. This inflammation can encompass the supra-glottic (above the vocal cords), glottic (vocal cords themselves), or subglottic (below the vocal cords) larynx, or any combination thereof, depending on the inciting agent.
- The inflammation leads to increased vascular permeability and fluid accumulation (edema) in the vocal cord tissues.
- As the inflammatory process progresses, white blood cells and other immune components arrive at the site of infection or irritation to remove pathogens or clear debris.
- This process enhances vocal cord edema, which adversely affects the normal vibration of the vocal folds, changing the amplitude, magnitude, and frequency of their dynamic movement.
- As the edema progresses, the phonation threshold pressure (the minimum subglottal pressure required to initiate vocal fold vibration) can increase. This means it becomes more difficult to generate adequate vocal fold vibration and produce clear sound.
- The patient develops phonatory changes (dysphonia or hoarseness) both as a result of the changing fluid-wave dynamics of the inflamed and edematous tissue, and as a result of both conscious and unconscious adaptation to attempt to mitigate these altered tissue dynamics (e.g., trying to push more air through).
- Sometimes edema is so marked that it becomes impossible to generate adequate phonation pressure, leading to frank aphonia (complete loss of voice). Such maladaptations (e.g., vocal strain) may result in prolonged vocal symptoms after an episode of acute laryngitis that can persist long after the inciting event has resolved.
- Acute laryngitis typically resolves within 2 weeks. Persistent symptoms beyond this timeframe may indicate a super-infection or a transition to chronic laryngitis, suggesting ongoing irritation or an underlying pathology.
Causes of Laryngitis
Acute Laryngitis
Infectious causes
- Viral agents: The most common cause of acute laryngitis. Viruses such as rhinovirus (common cold), parainfluenza virus, respiratory syncytial virus (RSV), coronavirus, adenovirus, and influenza virus are all potential etiologic agents (listed in roughly descending order of frequency). It is possible for bacterial super-infection to occur in the setting of viral laryngitis, which classically occurs approximately seven days after symptoms begin, leading to worsening symptoms.
- Bacterial organisms: Less common as primary causes but can be involved in superinfections. Common bacterial culprits include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Certain exanthematous febrile illnesses such as measles, chickenpox, and pertussis (whooping cough) are also associated with acute laryngitis symptoms, so it is prudent to obtain an accurate immunization history.
- Fungal infection: Laryngitis caused by fungal infections like Candida albicans is very rare in immunocompetent individuals. It is more often seen as chronic laryngitis in immunocompromised patients (e.g., those with HIV/AIDS, cancer patients undergoing chemotherapy) or in patients using inhaled steroid medications (e.g., for asthma or COPD) without proper rinsing of the mouth after use.
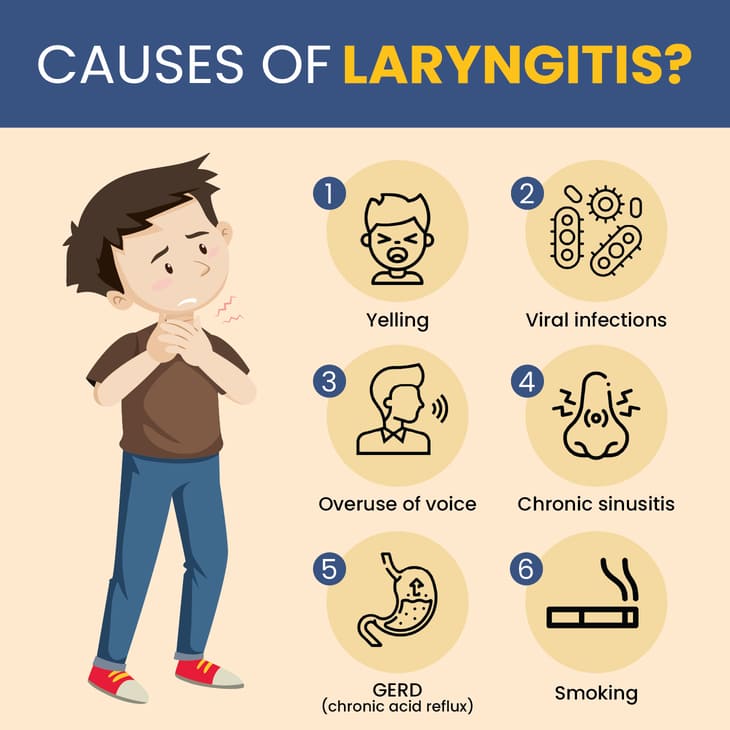
Non-infectious causes
Acute non-infectious laryngitis can be due to:
- Vocal trauma/abuse/misuse: Such as excessive shouting, singing, or prolonged talking.
- Allergies: Inhalation of allergens can cause inflammation of the laryngeal mucosa.
- Gastro-esophageal reflux disease (GERD) or Laryngopharyngeal Reflux (LPR): Stomach acid irritating the larynx.
- Asthma: Can sometimes cause irritation or inflammation in the larynx.
- Environmental irritants: Exposure to pollutants, chemical fumes, or dry air.
- Smoking: Direct irritation from tobacco smoke.
- Inhalational injuries: Such as inhaling smoke from fires.
- Functional/conversion disorders: Psychogenic causes where no organic pathology is found.
Chronic Laryngitis
A variety of factors can cause chronic laryngitis, often involving prolonged irritation or damage to the vocal cords:
- Long-term cigarette smoking: A major cause, as smoke directly irritates the vocal cords and can lead to swelling and changes in the laryngeal lining.
- Gastroesophageal reflux (GERD) or Laryngopharyngeal Reflux (LPR): Stomach acid moving up into the esophagus and irritating the larynx over time, often without typical heartburn symptoms.
- Excessive alcohol consumption: Can irritate the vocal cords.
- Chronic exposure to environmental irritants: Such as chemical fumes, dust, or allergens.
- Vocal abuse or overuse: Chronic strain on the voice due to professional use (singers, teachers) or habitual shouting.
- Chronic sinusitis or bronchitis: Postnasal drip can continuously irritate the larynx.
- Vocal cord lesions: Such as polyps, nodules (singer's nodes), cysts, or granulomas that form on the vocal cords due to chronic irritation or overuse.
- Neurological conditions: Affecting vocal cord movement (e.g., vocal cord paralysis).
- Allergies: Persistent allergic reactions.
- Pneumonia: Can sometimes be associated with persistent cough and laryngeal irritation.
- Thyroid dysfunction: Hypothyroidism can sometimes affect vocal cord function.
- Rare causes: Autoimmune diseases (e.g., rheumatoid arthritis affecting laryngeal joints), granulomatous diseases (e.g., sarcoidosis), or even early laryngeal cancer.
Clinical manifestations
Acute Laryngitis
In addition to symptoms of an upper respiratory tract infection (i.e., fever, cough, rhinitis), the patient primarily experiences dysphonia or a hoarse voice. The individual may also experience the following:
- Hoarseness of the voice: The hallmark symptom, ranging from mild to severe.
- Weakened voice or loss of voice (aphonia): Due to the vocal cords being too swollen to vibrate effectively.
- Rough or raspy voice quality.
- Constant tickling sensation or minor throat irritation.
- Dry cough: Often irritating and persistent.
- Odynophonia: Pain when speaking.
- Dysphagia: Difficulty swallowing.
- Odynophagia: Painful swallowing (less common than in pharyngitis).
- Dyspnea: Shortness of breath, especially if there is significant laryngeal swelling (more common in children with croup).
- Rhinorrhea: Runny nose (if associated with a common cold).
- Postnasal discharge: Mucus dripping down the back of the throat.
- Sore throat: May accompany other URI symptoms.
- Congestion: Nasal or chest congestion.
- Fatigue and malaise: General feeling of being unwell.
- Fever: Usually low-grade, if present.
Chronic Laryngitis
Symptoms are usually less acute but persistent:
- Persistent hoarseness: The primary and most common symptom, lasting for weeks or months.
- Loss of voice: May occur intermittently or be constant in severe cases.
- A raw or irritated throat sensation.
- A persistent dry cough.
- Frequent throat clearing.
- Feeling of a lump in the throat (globus sensation).
- Reduced vocal range or fatigue when speaking.
- Difficulty swallowing: Less common, but can occur if there's significant inflammation or associated conditions like GERD.
- Swelling of the lymph nodes in your neck: Not common in isolated chronic laryngitis, but may indicate an underlying infection or more serious condition.
- Fever: Generally absent in non-infectious chronic laryngitis.
Test and Diagnosis
Acute Laryngitis
Diagnosis is primarily clinical, based on patient history and physical examination.
- History: Presence of typical symptoms like hoarseness, often following an upper respiratory infection, and duration of symptoms usually less than 3 weeks.
- Physical examination: Examination of the throat may reveal redness or inflammation. Direct visualization of the larynx is usually not necessary for uncomplicated acute laryngitis.
- Laryngoscopy: Direct visualization of the larynx using a laryngoscope is generally reserved for cases of persistent symptoms, severe symptoms, or if there is concern for a more serious underlying condition. This allows the clinician to see inflamed and edematous vocal cords, sometimes with mucus or slight redness.
Chronic Laryngitis
Diagnosis requires a more thorough investigation to identify the underlying cause, as the symptoms persist for more than 3 weeks.
- History: Detailed history of chronic hoarseness, vocal habits, exposure to irritants (smoking, chemicals), symptoms of GERD, allergies, and any associated systemic conditions.
- Laryngoscopy: This is a crucial diagnostic tool for chronic laryngitis. It allows direct visualization of the vocal cords and surrounding structures. Findings may include:
- Redness and swelling of vocal cords.
- Presence of vocal cord nodules, polyps, cysts, granulomas.
- Changes suggestive of chronic reflux (e.g., posterior laryngeal erythema).
- Signs of Reinke's edema (swelling of the vocal cords due to smoking).
- Suspicious lesions that may indicate malignancy.
- Imaging studies:
- CT scan or MRI of the neck and throat: May be performed to rule out tumors, anatomical abnormalities, or spread of disease, especially if malignancy is suspected or if a mass is palpated.
- Laboratory tests:
- High throat swab for culture and sensitivity: If bacterial or fungal infection is suspected and visualized, a swab can be taken for culture to identify the pathogen and determine appropriate antibiotic/antifungal treatment.
- Full blood count (CBC): Can indicate signs of infection or other systemic issues.
- Allergy testing: If allergies are suspected as a contributing factor.
- pH monitoring: Esophageal pH monitoring (24-hour pH impedance study) can be done to confirm GERD or LPR, especially if symptoms are atypical or unresponsive to treatment.
- Biopsy: If any suspicious lesions are found during laryngoscopy, a biopsy may be taken for histopathological examination to rule out malignancy.
Management
Medical Management
Treatment is often supportive in nature and depends on the severity and underlying cause of laryngitis. The primary goals are to reduce inflammation, alleviate symptoms, and identify/address the root cause.
- Voice rest: This is the single most important factor for acute laryngitis. Use of the voice during laryngitis results in incomplete or delayed recovery and can worsen vocal cord damage. Complete voice rest is recommended, although it is almost impossible to achieve. If the patient needs to speak, they should be instructed to use a "confidential voice" – a normal phonatory voice at low volume without whispering or projecting, as whispering can strain the vocal cords more than soft speaking.
- Humidification: Inhaling humidified air (e.g., from a cool-mist humidifier, steam inhalation from a bowl of hot water, or a steamy shower) enhances moisture of the upper airway and vocal cords, which helps to soothe irritation, reduce swelling, and facilitate the removal of secretions and exudates.
- Avoidance of irritants: Smoking and alcohol should be strictly avoided as they significantly irritate the laryngeal mucosa and delay prompt resolution of the disease process. Exposure to environmental pollutants, dust, and allergens should also be minimized.
- Dietary modification: Dietary restrictions are recommended for patients with gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR). This includes avoiding caffeinated drinks, spicy food items, fatty food, chocolate, peppermint, citrus fruits, and carbonated beverages. Another important lifestyle modification is the avoidance of late meals; the patient should have meals at least 3 hours before sleeping to prevent nocturnal reflux. The patient should drink plenty of water to maintain hydration. While the efficacy of these dietary measures is well-established for classic GERD, their effectiveness in LPR is debated, but they are often still employed.
- Medications:
- Antibiotics: Antibiotic prescription for an otherwise healthy patient with acute viral laryngitis is currently unsupported and ineffective. However, for high-risk patients (e.g., immunocompromised) or patients with severe symptoms and confirmed bacterial infection (e.g., with signs of bacterial superinfection), antibiotics may be given. Some authors recommend narrow-spectrum antibiotics only in the presence of identifiable gram stain and culture.
- Antivirals: Rarely used for laryngitis unless a specific viral cause (e.g., severe influenza or herpes simplex) is identified and treatment is indicated.
- Antifungals: Fungal laryngitis can be treated with the use of oral antifungal agents such as fluconazole. Treatment is usually required for a three-week period and may be repeated if needed. This should be reserved for patients with confirmed fungal infection via laryngeal examination and/or culture.
- Mucolytics: Like guaifenesin, may be used for clearing thick secretions.
- Corticosteroids: May be prescribed in severe cases of acute laryngitis with significant vocal cord swelling causing severe hoarseness or mild airway compromise (e.g., croup in children) to rapidly reduce inflammation. Long-term use is generally avoided due to side effects.
- Anti-reflux medications: In addition to lifestyle and dietary modifications, LPR-related laryngitis is treated with anti-reflux medications. Medications that suppress acid production, such as H2 receptor blockers (e.g., ranitidine, famotidine) and proton pump inhibitors (PPIs) (e.g., omeprazole, lansoprazole, esomeprazole), are effective against gastroesophageal reflux. PPIs are generally found to be most effective for LPR. These may require higher doses or a twice-daily dosing schedule to be effective in this setting, and treatment often needs to be long-term.
- Analgesics/Antipyretics: Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage associated pain and fever.
- Voice Therapy: For chronic laryngitis, particularly that related to vocal abuse/misuse or vocal cord lesions, referral to a speech-language pathologist for voice therapy is crucial. Therapy teaches proper vocal hygiene, efficient voice production techniques, and strategies to prevent further vocal cord injury.
- Surgical Intervention: For chronic laryngitis caused by vocal cord polyps, nodules, cysts, or other lesions that do not resolve with conservative management, surgical removal may be necessary.
Nursing Interventions/Management
1. Assessment of the Patient
- a. Obtain a comprehensive history including the onset, duration, and nature of hoarseness or voice changes. Inquire about associated symptoms like cough, sore throat, difficulty swallowing, fever, and symptoms of upper respiratory infection or reflux.
- b. Assess for potential causes: recent illness, vocal overuse/abuse (e.g., shouting, singing), exposure to irritants (smoking, chemicals), allergies, and history of GERD.
- c. Perform vital sign assessment (Temperature, Pulse, Respiration, Blood Pressure) and a general physical examination. Note any signs of respiratory distress, stridor, or changes in voice quality.
- d. Document the patient's vocal habits, profession (if voice-demanding), and lifestyle (smoking, alcohol use).
- e. Inquire about any past medical history, current medications, and allergies.
2. Promoting Voice Rest and Vocal Hygiene
- a. Educate the patient on the critical importance of absolute voice rest during acute laryngitis. Explain that talking, whispering, and throat clearing can further irritate and damage vocal cords.
- b. Instruct the patient to use non-vocal communication methods (e.g., writing, gestures) as much as possible.
- c. Teach "confidential voice" if speaking is unavoidable: speak softly but not whisper, use natural pitch.
- d. Emphasize avoidance of vocal strain, shouting, screaming, and prolonged singing.
3. Managing Symptoms and Promoting Comfort
- a. Encourage increased fluid intake to keep vocal cords hydrated and thin secretions. Warm fluids (e.g., herbal tea with honey) or cool liquids may be soothing.
- b. Advise the use of a cool-mist humidifier in the patient's room, especially at night, to humidify the air and soothe the larynx.
- c. Instruct on proper steam inhalation techniques (e.g., leaning over a bowl of hot water with a towel over the head for 5-10 minutes, several times a day), ensuring safety to prevent burns.
- d. Administer prescribed analgesics (e.g., acetaminophen, ibuprofen) for pain relief and antipyretics for fever.
- e. Encourage throat lozenges or sprays to relieve irritation and dryness, if appropriate.
- f. Instruct on gargling with warm salt water to reduce throat discomfort.
- g. Advise avoiding irritants such as tobacco smoke (including secondhand smoke), alcohol, and caffeine, which can dry out and irritate the vocal cords.
4. Preventing and Managing Complications
- a. Monitor for signs of respiratory distress (e.g., increased respiratory rate, shortness of breath, stridor, retractions, cyanosis), especially in children, as laryngeal swelling can compromise the airway. Report immediately to the physician.
- b. For chronic laryngitis, educate the patient about the potential long-term effects of persistent inflammation (e.g., vocal cord nodules, polyps, or changes that could mask malignancy).
- c. Ensure the patient completes the full course of antibiotics if prescribed for bacterial laryngitis to prevent recurrence or resistance.
- d. For patients with GERD/LPR, reinforce adherence to dietary and lifestyle modifications (e.g., elevating the head of the bed, avoiding late meals, dietary triggers) and consistent use of anti-reflux medications.
5. Health Education and Patient Teaching
- a. Educate the patient and family about the causes, symptoms, and treatment of laryngitis, distinguishing between acute and chronic forms.
- b. Provide detailed instructions on proper vocal hygiene, including the importance of hydration, avoiding shouting/whispering, and resting the voice.
- c. Teach patients about identifying and avoiding personal triggers for laryngitis (e.g., allergens, irritants, vocal abuse).
- d. For patients with chronic laryngitis due to GERD, provide comprehensive education on anti-reflux measures.
- e. Emphasize the importance of follow-up care, especially if symptoms persist or worsen, or if there is concern for chronic conditions or malignancy.
- f. Advise seeking medical attention immediately for severe symptoms such as difficulty breathing, severe pain, or inability to swallow.
6. Referral and Collaboration
- a. Collaborate with the healthcare team, including physicians, speech-language pathologists (for voice therapy in chronic cases), and allergists or gastroenterologists if underlying conditions like allergies or GERD are present.
- b. Facilitate referrals to specialists as needed (e.g., otolaryngologist for laryngoscopy in chronic or atypical cases).
Complications
While acute laryngitis is usually benign and self-limiting, complications can arise, especially if the underlying cause is not addressed or in specific populations. Chronic laryngitis, due to persistent irritation, can lead to more significant issues.
- Airway Obstruction (especially in children): In infants and young children, significant swelling of the subglottic area (below the vocal cords) can lead to a condition called croup (laryngotracheobronchitis). This causes a characteristic "barking" cough, stridor (a high-pitched crowing sound during inhalation), and difficulty breathing, which can be life-threatening and require immediate medical attention. In adults, severe laryngeal edema can also rarely lead to airway compromise.
- Vocal Cord Lesions: Chronic inflammation, vocal abuse, or irritation can lead to the development of benign lesions on the vocal cords:
- Vocal Nodules (Singer's Nodes): Callus-like growths that result from chronic vocal cord abuse, leading to persistent hoarseness.
- Vocal Polyps: Softer, blister-like growths, often unilateral, that can result from a single traumatic vocal event or chronic irritation.
- Vocal Cysts: Fluid-filled sacs within the vocal cord.
- Granulomas: Inflammatory lesions, often associated with intubation trauma or LPR.
- Reinke's Edema: A severe swelling of the vocal cords, almost exclusively seen in heavy smokers, leading to a deep, husky voice.
- Chronic Hoarseness/Dysphonia: Persistent voice changes that significantly impact communication and quality of life, leading to vocal fatigue, pain, or professional limitations.
- Psychological Impact: Chronic voice problems can lead to frustration, social isolation, anxiety, or depression, especially in individuals whose profession relies on their voice.
- Misdiagnosis of Serious Conditions: Persistent hoarseness, especially in smokers or heavy drinkers, can be a symptom of laryngeal cancer. Untreated chronic laryngitis can delay the diagnosis of malignancy, which is a critical concern.
- Spread of Infection: If infectious laryngitis is not properly managed, especially bacterial cases, the infection can spread to other parts of the respiratory tract, leading to bronchitis, pneumonia, or other more systemic infections.
- Laryngeal Stenosis: In rare cases, chronic inflammation or repeated trauma can lead to scarring and narrowing of the larynx (stenosis), which can severely restrict airflow and may require surgical intervention.
It is crucial for persistent hoarseness (lasting more than 2-3 weeks), especially in adults, to be evaluated by an otolaryngologist (ENT specialist) to rule out serious underlying conditions, including malignancy.
Nursing management
1. Assessment of the patient
- a. Carrying out history of the presenting signs and symptoms e.g. fever, fatigue, throat pain and hoarseness of the voice among others.
- b. Taking vital observation e.g. TPR/BP and general examination to exclude other diseases
- c. Alerting the doctor who will order for investigations and admission, there the nurse will assist the patient throughout the process.
2. Managing fever (patient has 37.6 and above temperature, chills)
- a. Assess the patient’s vital signs at least every 4 hours.
- b. Remove excessive clothing, blankets, and linens. Adjust the room temperature.
- c. Administer and monitor the prescribed antibiotics and anti-pyretics.
- d. Assess the mental status of the patient because elevated temperatures can alter the function of the mind.
- e. Offer a tepid sponge bath.
- f. Elevate the head of the bed
3. To alleviate pain
- a. Assess the patient’s vital signs and characteristics of pain at least 30 minutes after administration of medication.
- b. Elevate the head of the bed and position the patient in semi Fowler’s.
- c. Administer prescribed analgesics
4. Ensuring clear airway
- a. Assess the patient’s vital signs and characteristics of respirations at least every 4 hours. Assess for signs of hypoxia.
- b. Place the patient on a side-lying or prone position.
- c. Suction secretions.
- d. Administer the prescribed medications (e.g. corticosteroids) and antibiotic medications.
5. To prevent infection
- a. Assess vital signs and observe for any signs of infection as well as for any signs of respiratory distress.
- b. Perform a focused assessment on the oropharyngeal region, particularly checking for any collection of abscess.
- c. Teach the patient how to perform proper hand hygiene.
- d. Administer antibiotics as prescribed.
6. Educate the patient about self-management
- a. Use a humidifier or inhale steam to alleviate dryness.
- b. Get vocal therapy to analyze and correct the way you use your voice and any abnormal speech patterns that place stress on your vocal cords and voice box.
- c. Drink lots of fluids.
- d. Gargle with 1/2 tsp. of salt and 1/2 tsp. of baking soda in 8 oz. of warm water.
- e. Rest your voice.
- f. Avoid screaming or talking loudly for long periods of time.
- g. Avoid decongestants, which can dry your throat.
- h. Suck on lozenges to keep your throat lubricated.
- i. Refrain from whispering, which can strain the voice.
Complications
- Epiglositis
- Pneumonia
- Chronic irritation of throat
- Throat cancer
- Chronic hoarseness of the voice