To understand Hodgkin's disease and Non-Hodgkin's lymphoma, we must first define what lymphomas are as a group of diseases.
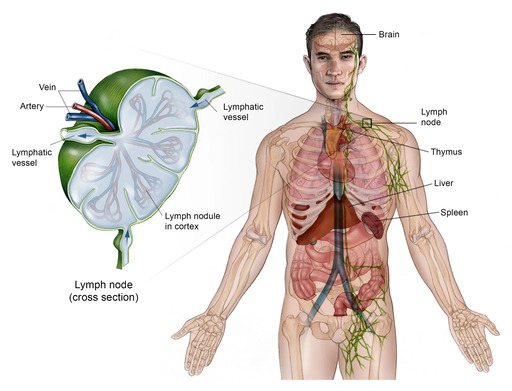
Lymphomas are a diverse group of cancers that originate in the lymphocytes, a type of white blood cell crucial for the immune system. These malignant lymphocytes typically arise in the lymphatic system, which is a network of tissues and organs that help rid the body of toxins, waste, and other unwanted materials. The primary components of the lymphatic system include the lymph nodes, spleen, thymus, bone marrow, and lymphatic vessels.
Hodgkin’s Lymphoma is a malignant disease in which the lymph glands are enlarged and there is an increase of lymphoid tissue in the liver spleen and bone marrow. This disease is fatal if not treated early It was described by a British physician called Thomas Hodgkin in 1832
- Origin in Lymphocytes: The cancerous cells are mutated lymphocytes (either B-lymphocytes or T-lymphocytes). These cells normally play a vital role in recognizing and fighting off infections and foreign invaders.
- Location: While they can originate in any part of the body that contains lymphatic tissue, they most commonly start in the lymph nodes, which are small, bean-shaped glands found throughout the body (e.g., in the neck, armpits, groin, chest, and abdomen).
- Growth Pattern: Unlike leukemias (which primarily involve the bone marrow and blood), lymphomas typically present as solid tumors within the lymphatic system. However, in advanced stages, they can spread to the blood, bone marrow, and other organs (e.g., liver, brain).
- Types: Lymphomas are broadly classified into two main categories:
- Hodgkin Lymphoma (HL): Characterized by the presence of a specific type of abnormal cell called the Reed-Sternberg cell.
- Non-Hodgkin Lymphoma (NHL): A much more diverse group that includes all lymphomas that are not Hodgkin Lymphoma.
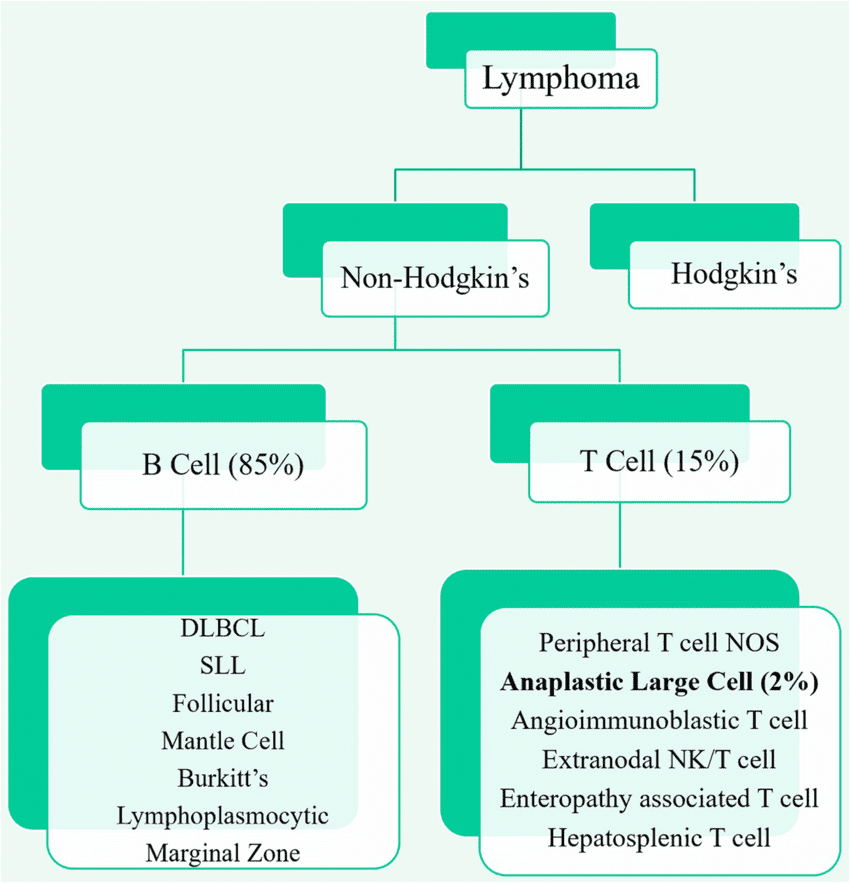
Lymphomas are broadly classified into two major categories based on specific pathological and clinical characteristics:
- Hodgkin Lymphoma (HL)
- Non-Hodgkin Lymphoma (NHL)
The distinction between these two types is critical because they differ significantly in their epidemiology, pathology, clinical presentation, and, importantly, their treatment approaches and prognosis.
- Defining Feature: The hallmark of Hodgkin Lymphoma is the presence of a unique, large, often multi-nucleated malignant cell known as the Reed-Sternberg cell (or a variant thereof) in a characteristic inflammatory background. These cells are typically derived from B-lymphocytes.
- Prevalence: It is less common than Non-Hodgkin Lymphoma, accounting for approximately 10-15% of all lymphomas.
- Age Distribution: Hodgkin Lymphoma has a bimodal age distribution, with peaks in young adulthood (ages 20-30) and in older adulthood (after age 55).
- Spread Pattern: Tends to spread in an orderly fashion, typically from one lymph node group to contiguous lymph node groups. This predictable pattern often allows for earlier detection and more localized disease.
- Prognosis: Generally considered one of the most curable cancers, especially when diagnosed in earlier stages.
- Defining Feature: Non-Hodgkin Lymphoma encompasses all lymphomas that lack the characteristic Reed-Sternberg cells. This group is incredibly heterogeneous, meaning it includes many different types of lymphoma with diverse origins, behaviors, and prognoses.
- Prevalence: Much more common than Hodgkin Lymphoma, accounting for approximately 85-90% of all lymphomas.
- Age Distribution: The incidence generally increases with age, with most cases occurring in older adults.
- Cell Origin: Can originate from either B-lymphocytes (most common, ~85%) or T-lymphocytes (~15%).
- Spread Pattern: Tends to spread in a less orderly and more unpredictable fashion, often disseminating to non-contiguous lymph node groups and extranodal sites (organs outside the lymphatic system) early in the disease course.
- Prognosis: Varies widely depending on the specific subtype, grade (aggressiveness), and stage at diagnosis. Some types are indolent (slow-growing) and may be managed for years, while others are aggressive and require immediate, intensive treatment.
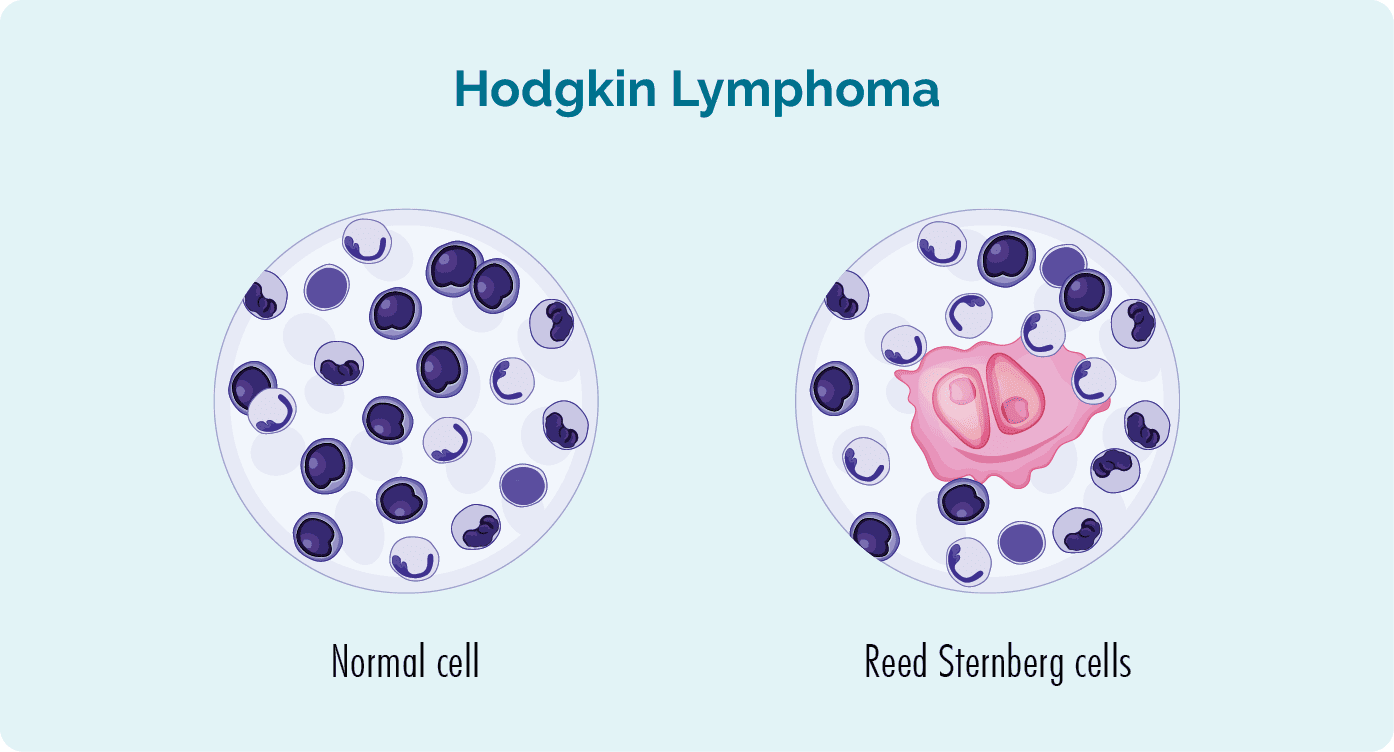
Hodgkin's Lymphoma (HL), also known as Hodgkin Disease, is a type of cancer that originates in the lymphatic system. It is distinctly characterized by the presence of a specific type of cancerous cell called the Reed-Sternberg (RS) cell.
- Malignant Cell of Origin: The defining feature is the Reed-Sternberg cell. These are large, often multinucleated cells with prominent nucleoli, frequently described as having an "owl's eye" appearance due to their bilobed nuclei and central nucleoli. While RS cells are the malignant component, they constitute only a small proportion (typically 0.5-10%) of the cells within the affected lymph node.
- Microenvironment: The vast majority of the tumor mass in Hodgkin's Lymphoma consists of a reactive cellular infiltrate (normal lymphocytes, plasma cells, eosinophils, histiocytes, and fibroblasts) that surrounds and interacts with the RS cells. This rich inflammatory microenvironment is characteristic.
- Cellular Lineage: Most Reed-Sternberg cells are derived from germinal center B-lymphocytes that have undergone malignant transformation, but have lost their typical B-cell phenotype and often express markers usually associated with other cell types.
- Clinical Behavior: HL typically presents with painless lymphadenopathy (enlarged lymph nodes), most commonly in the cervical (neck) or supraclavicular (above the collarbone) regions. It classically spreads in an orderly and contiguous fashion from one lymph node region to adjacent lymph node regions.
- Prognosis and Curability: Hodgkin's Lymphoma is one of the most curable cancers, especially with modern treatment protocols. The presence of RS cells and the characteristic inflammatory background are key to its diagnosis and differentiation from Non-Hodgkin Lymphoma, which guides treatment strategies and often results in a favorable outcome.
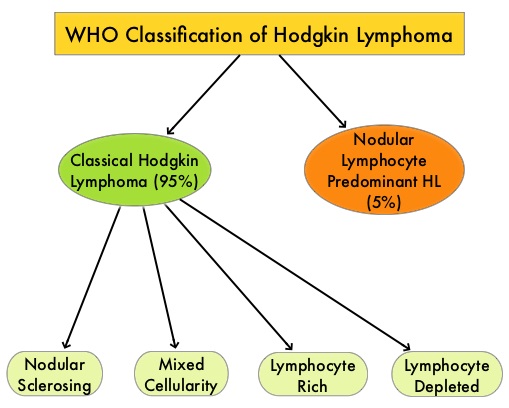
The World Health Organization (WHO) classification divides Hodgkin Lymphoma (HL) into two main types:
- Nodular Lymphocyte-Predominant Hodgkin Lymphoma (NLPHL)
- Classical Hodgkin Lymphoma (CHL), which is further subdivided into four histological subtypes.
- Prevalence: Accounts for about 5% of all Hodgkin Lymphoma cases.
- Characteristic Cell: Defined by the presence of unique large, often lobulated, pale-staining cells known as "popcorn cells" (or L&H cells – Lymphocytic and Histiocytic cells). These are variants of Reed-Sternberg cells, but are typically CD20-positive (a B-cell marker) and lack CD15 and CD30 (markers typical for classical RS cells).
- Microenvironment: The tumor cells are found within a background rich in small lymphocytes, often forming a nodular pattern.
- Clinical Features:
- More common in males.
- Typically presents with localized peripheral lymphadenopathy, often in the cervical, axillary, or inguinal regions.
- Usually has an indolent (slow-growing) course.
- Patients rarely present with "B symptoms" (fever, night sweats, weight loss).
- Has a tendency for late relapses and can transform into aggressive B-cell non-Hodgkin lymphoma (diffuse large B-cell lymphoma) in a small percentage of cases.
- Prognosis: Generally has an excellent prognosis, often better than classical HL.
- Prevalence: Accounts for the vast majority (95%) of Hodgkin Lymphoma cases.
- Characteristic Cell: Defined by the presence of typical Reed-Sternberg (RS) cells and their variants (e.g., lacunar cells, mummified cells). These cells are typically CD15-positive and CD30-positive, and usually CD20-negative or weakly positive.
- Microenvironment: RS cells are surrounded by a diverse inflammatory infiltrate.
- Clinical Features:
- Often presents with mediastinal and/or cervical lymphadenopathy.
- "B symptoms" are more common.
- Spreads contiguously through lymph node chains.
- * Most Common Subtype: Accounts for 60-80% of all CHL cases.
- * Characteristic Features: Presence of "lacunar cells" (RS variants that appear to sit in empty spaces or lacunae due to artifactual retraction during processing), often with broad bands of collagen fibrosis (sclerosis) that divide the lymph node into nodules.
- * Demographics: More common in adolescents and young adults, and more prevalent in women.
- * Clinical Presentation: Frequently involves mediastinal lymph nodes.
- * Prognosis: Generally excellent.
- * Second Most Common Subtype: Accounts for 15-30% of CHL cases.
- * Characteristic Features: A diffuse effacement of the lymph node architecture by a pleomorphic infiltrate containing numerous classical RS cells and various inflammatory cells (lymphocytes, plasma cells, eosinophils, histiocytes) without significant nodularity or sclerosis.
- * Demographics: More common in older adults, individuals with HIV, and those in developing countries.
- * Clinical Presentation: Often associated with "B symptoms."
- * Prognosis: Good, though sometimes slightly less favorable than NSCHL at advanced stages.
- * Less Common Subtype: Accounts for about 5% of CHL cases.
- * Characteristic Features: Contains a relatively high proportion of small lymphocytes and relatively few classical RS cells, which are often difficult to find. There is typically no nodularity or sclerosis.
- * Clinical Presentation: Often presents in early stages, with peripheral lymphadenopathy.
- * Prognosis: Excellent, often similar to NSCHL.
- * Rarest Subtype: Accounts for less than 1% of CHL cases.
- * Characteristic Features: Characterized by a paucity of lymphocytes and an abundance of classical RS cells, often with diffuse fibrosis or necrosis. Can be confused with diffuse large B-cell lymphoma.
- * Demographics: More common in older adults and those with HIV.
- * Clinical Presentation: Often presents in advanced stages with "B symptoms" and involvement of bone marrow, liver, and spleen.
- * Prognosis: Historically the least favorable prognosis among CHL subtypes, though outcomes have improved with modern therapy.
1. Painless Lymphadenopathy:
- This is the most common presenting symptom, occurring in about 80-90% of patients.
- Description: Firm, rubbery, discrete, non-tender, and mobile enlarged lymph nodes. They generally do not cause pain unless they grow very large and compress surrounding structures or are rapidly enlarging.
- Location:
- Cervical (neck) and supraclavicular (above collarbone) regions: Most frequently involved (60-80% of cases).
- Axillary (armpit) regions: Common.
- Inguinal (groin) regions: Less common as the primary site.
- Mediastinal (chest) involvement: Very common, especially with nodular sclerosis HL. Can be asymptomatic but may cause cough, shortness of breath, or chest discomfort if large enough to compress airways or blood vessels.
2. Orderly Spread: HL typically spreads in a contiguous fashion, meaning it moves from one lymph node group to an adjacent one.
Approximately one-third of HL patients, especially those with advanced disease, experience systemic symptoms collectively known as "B symptoms." The presence of B symptoms is important for staging and prognosis.
- Unexplained Fever:
- Temperature > 38°C (100.4°F) for three consecutive days, without any evidence of infection.
- Pel-Ebstein fever: A classic but rare pattern of high fever for several days alternating with afebrile periods of similar duration.
- Drenching Night Sweats: So severe that clothes and bedding need to be changed, occurring without an apparent environmental cause.
- Unexplained Weight Loss: Loss of more than 10% of body weight within the past six months, without dieting or other illness.
- Pruritus (Itching): Generalized, often severe, and non-specific itching, which can be quite distressing. The cause is not fully understood.
- Alcohol-Induced Pain: A classic but rare symptom where pain occurs in affected lymph nodes shortly after alcohol consumption. The mechanism is unknown.
- Fatigue: Generalized tiredness and lack of energy, often out of proportion to activity.
- Splenomegaly: Enlargement of the spleen, indicating splenic involvement, found in about 30% of patients, usually palpable.
- Hepatomegaly: Enlargement of the liver, indicating hepatic involvement, less common than splenomegaly.
- Extranodal Disease: While HL is primarily a nodal disease, direct extension from adjacent lymph nodes (e.g., to lung, bone, pleura) or distant extranodal involvement (e.g., bone marrow, liver, bone) can occur, particularly in advanced stages.
- Immunosuppression: Patients with HL, particularly those with advanced disease or after treatment, can experience compromised cellular immunity, leading to increased susceptibility to infections (e.g., fungal infections, Herpes zoster).
The most widely used system for staging Hodgkin's Lymphoma is the Ann Arbor Staging Classification.
- Lymphatic Regions: The diaphragm is considered a key anatomical landmark. Lymph node involvement is categorized as occurring above or below the diaphragm.
- Contiguous Spread: As HL typically spreads contiguously, the number of involved regions and their location relative to the diaphragm are important.
- Extranodal Involvement: Involvement of organs outside the lymphatic system is denoted.
- Systemic Symptoms: The presence or absence of "B symptoms" (fever, night sweats, weight loss) is appended to the stage.
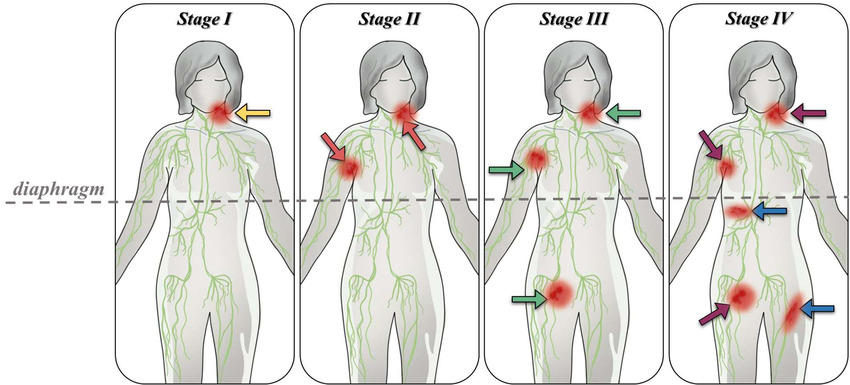
- Stage I: Involvement of a single lymph node region (e.g., one group of nodes in the neck) or a single extralymphatic organ site (IE). Location: Confined to one side of the diaphragm.
- Stage II: Involvement of two or more lymph node regions on the same side of the diaphragm, or localized involvement of a single extralymphatic organ or site and its regional lymph nodes (IIE). Location: Confined to one side of the diaphragm.
- Stage III: Involvement of lymph node regions on both sides of the diaphragm.
- III(1): Involvement of abdominal lymph nodes (e.g., spleen, celiac, portal, or peri-aortic nodes).
- III(2): Involvement of inguinal, mesenteric, or para-aortic lymph nodes.
- Spleen Involvement (S): If the spleen is involved, it is often denoted with 'S'.
- Stage IV: Diffuse or disseminated involvement of one or more extralymphatic organs, with or without associated lymph node involvement; or isolated extralymphatic organ involvement with distant (non-regional) lymph node involvement. Common Extralymphatic Sites: Bone marrow, liver, lung, bone.
- A: Absence of B symptoms.
- B: Presence of B symptoms.
- E: Involvement of a single extralymphatic organ or site.
- X: Bulky disease (large tumor mass).
| Condition | Why it's similar | Key difference |
|---|---|---|
| Non-Hodgkin Lymphoma (NHL) | Also presents with painless lymphadenopathy and can have B symptoms. | Histopathology (lack of Reed-Sternberg cells, different cellular morphology, immunophenotype) is the definitive differentiator. NHL is a much more heterogeneous group. |
| Metastatic Carcinoma | Enlarged, firm lymph nodes, often in the cervical or supraclavicular regions. | Biopsy will reveal epithelial cells (carcinoma) rather than lymphoid cells, and immunohistochemistry will show different markers. Often, there's a known primary tumor. |
| Leukemias (especially CLL) | Can cause generalized lymphadenopathy. | Primarily involve the bone marrow and peripheral blood. Diagnosis involves blood counts, bone marrow biopsy, and flow cytometry. |
| Sarcomas | Can present as masses that may be mistaken for lymph nodes. | Originates from connective tissue, not lymphoid cells. Histopathology is distinct. |
| Castleman Disease | A rare lymphoproliferative disorder causing localized or generalized lymphadenopathy. | Histopathology shows characteristic features distinct from lymphoma (e.g., hypervascularity, onion-skinning of follicles). |
| Infectious Mononucleosis (EBV) | Widespread lymphadenopathy, fever, fatigue, splenomegaly. | Acute onset, often with sore throat. Diagnosis by serology and atypical lymphocytes on blood smear. Biopsy shows reactive hyperplasia. |
| Tuberculosis (TB) Lymphadenitis | Chronic, often painless, progressive lymph node enlargement (cervical). | Diagnosis by PCR for Mycobacterium tuberculosis, culture, and histopathology showing granulomatous inflammation with caseous necrosis. |
| HIV Lymphadenopathy | Chronic, painless, generalized lymphadenopathy. | Positive HIV test. Biopsy shows follicular hyperplasia. |
| Toxoplasmosis | Cervical lymphadenopathy, sometimes with fever and fatigue. | Diagnosis by serology. Biopsy shows characteristic reactive changes. |
| Cat Scratch Disease | Localized lymphadenopathy following cat scratch/bite. | History of cat exposure. Diagnosis by serology or PCR. Biopsy shows characteristic suppurative granulomas. |
| Bacterial Lymphadenitis | Enlarged, often painful lymph nodes, signs of acute infection. | Acute onset, pain, redness, warmth. Resolves with antibiotics. |
| Sarcoidosis | Bilateral hilar lymphadenopathy and peripheral lymphadenopathy. | Biopsy shows non-caseating granulomas. Elevated ACE levels. |
| SLE or Rheumatoid Arthritis | Generalized lymphadenopathy, systemic inflammation. | Presence of other systemic autoimmune features and positive autoantibody tests (ANA, RF). |
- 1. ABVD Regimen:
- Components: Adriamycin (Doxorubicin), Bleomycin, Vinblastine, and Dacarbazine.
- Usage: The most common and standard first-line chemotherapy regimen.
- Side Effects: Nausea, vomiting, hair loss, fatigue, myelosuppression, cardiotoxicity (doxorubicin), and pulmonary toxicity (bleomycin).
- 2. BEACOPP Regimen:
- Components: Bleomycin, Etoposide, Adriamycin, Cyclophosphamide, Oncovin (Vincristine), Procarbazine, and Prednisone.
- Usage: A more intensive regimen for advanced-stage HL and unfavorable prognostic factors.
- Side Effects: Higher rates of myelosuppression, secondary malignancies, and infertility.
- 3. Other Regimens/Salvage Chemotherapy: For relapsed or refractory HL (e.g., ICE, DHAP, GVD), often followed by autologous stem cell transplantation.
- Involved-Site Radiation Therapy (ISRT): Targets only the initially involved lymph node regions. Used to consolidate remission and reduce local recurrence.
- Involved-Node Radiation Therapy (INRT): A more precise form of ISRT targeting only involved nodes.
- Brentuximab Vedotin (BV): An antibody-drug conjugate that targets CD30 on RS cells.
- PD-1 Inhibitors (e.g., Nivolumab, Pembrolizumab): Block the PD-1 checkpoint pathway to unleash the body's immune system against cancer cells.
- Usage: Standard for relapsed or refractory HL. Patients receive very high doses of chemotherapy followed by infusion of their own stem cells.
Non-Hodgkin Lymphoma (NHL) refers to a diverse group of cancers that originate in the lymphocytes. Unlike Hodgkin's Lymphoma, NHL encompasses a wide spectrum of lymphoid malignancies with varying cellular origins, histological features, clinical behaviors, and prognoses.
- Origin: NHL arises from either B lymphocytes (B-cells) or T lymphocytes (T-cells), and rarely from natural killer (NK) cells. The vast majority (~85-90%) are of B-cell origin.
- Absence of Reed-Sternberg Cells: The defining feature distinguishing NHL from HL is the absence of Reed-Sternberg cells.
- Heterogeneity: NHL is a collection of over 60 distinct subtypes varying in histology, immunophenotype, genetics, and clinical behavior.
- Spread Pattern: Unlike HL, NHL often spreads in a non-contiguous, unpredictable manner. It can involve distant lymph node sites and extranodal organs early in the disease course.
- Incidence: NHL is significantly more common than HL.
- Indolent (Slow-Growing): Grow slowly, often disseminated at diagnosis, may not require immediate treatment ("watch and wait"). Incurable but controllable. (e.g., Follicular Lymphoma, SLL/CLL).
- Aggressive (Fast-Growing): Grow rapidly, severe symptoms, require prompt treatment. Potentially curable. (e.g., DLBCL).
- Highly Aggressive (Very Fast-Growing): Grow extremely rapidly, require immediate intensive chemotherapy. (e.g., Burkitt Lymphoma).
- Indolent:
- Follicular Lymphoma (FL): Nodular growth, t(14;18) translocation (BCL2 overexpression). Widespread painless lymphadenopathy.
- Small Lymphocytic Lymphoma (SLL) / Chronic Lymphocytic Leukemia (CLL): Small, mature-looking lymphocytes.
- Marginal Zone Lymphoma (MZL): Can be extranodal (MALT lymphoma).
- Lymphoplasmacytic Lymphoma (Waldenström Macroglobulinemia): Secretes IgM paraprotein.
- Aggressive:
- Diffuse Large B-cell Lymphoma (DLBCL): Most common NHL. Large atypical B-cells, diffuse pattern. Rapidly enlarging.
- Mantle Cell Lymphoma (MCL): t(11;14) translocation (Cyclin D1). Aggressive course.
- Highly Aggressive:
- Burkitt Lymphoma (BL): t(8;14) involving MYC oncogene. Extremely rapid growth. Endemic (Africa), Sporadic, or Immunodeficiency-associated.
- Peripheral T-cell Lymphoma (PTCL, NOS): "Wastebasket" category, often aggressive.
- Anaplastic Large Cell Lymphoma (ALCL): Large pleomorphic T-cells, can be ALK-positive or negative.
- Mycosis Fungoides / Sézary Syndrome: Cutaneous T-cell lymphomas.
- Generalized Symptoms ("B Symptoms"): Fever, Night Sweats, Weight Loss. (Less frequent in indolent NHL).
- Lymphadenopathy: Painless swelling of lymph nodes. Can be generalized.
- Extranodal Disease: A hallmark differentiating NHL from HL. Common sites:
- GI Tract: Pain, bleeding, obstruction.
- Bone Marrow: Cytopenias (fatigue, bleeding, infection).
- Skin: Rashes, nodules, ulcers.
- CNS: Headaches, seizures, deficits.
- Spleen/Liver/Bone/Waldeyer's Ring.
Uses the Ann Arbor/Lugano Staging Classification, similar to HL but adapted for non-contiguous spread.
- Stage I: Single node region or single extralymphatic site.
- Stage II: Two or more regions on same side of diaphragm.
- Stage III: Regions on both sides of diaphragm.
- Stage IV: Diffuse/disseminated extralymphatic involvement.
International Prognostic Index (IPI): For aggressive NHL (e.g., DLBCL). Risk factors: Age > 60, Elevated LDH, Performance Status ≥ 2, Stage III/IV, Extranodal sites > 1.
- Biopsy (Gold Standard): Excisional Biopsy is crucial for morphology, Immunohistochemistry (IHC), Flow Cytometry, and Molecular Genetics (FISH/PCR).
- Imaging: PET-CT Scan (metabolically active disease), CT Scans, MRI (CNS).
- Labs: CBC, LFTs, KFTs, LDH (prognostic), Uric Acid, Beta-2 Microglobulin, Viral Studies (HIV, HBV, HCV, EBV).
- Procedures: Bone Marrow Biopsy, Lumbar Puncture (if CNS suspicion).
- Chemotherapy:
- CHOP Regimen: Cyclophosphamide, Hydroxydaunorubicin, Oncovin, Prednisone. Foundational for aggressive B-cell lymphomas.
- High-Dose Chemotherapy with ASCT.
- Immunotherapy:
- Rituximab (Anti-CD20): Monoclonal antibody targeting B-cells. Often added to CHOP (R-CHOP).
- Antibody-Drug Conjugates (ADCs).
- Immune Checkpoint Inhibitors.
- CAR T-cell Therapy: Genetically modified patient T-cells targeting cancer antigens (e.g., CD19).
- Bispecific Antibodies.
- Radiation Therapy: For local control or palliative care.
- Targeted Therapies: BTK Inhibitors (Ibrutinib), PI3K Inhibitors, BCL2 Inhibitors (Venetoclax), etc.
- "Watch and Wait": For asymptomatic indolent lymphomas.
Management of Hodgkin’s lymphoma
- Radiation therapy for localized disease
- Short course combination therapy with less extensive radiation
- Radiation is combined with chemotherapy to treat disseminated disease
- Cytotoxic drugs are combined with steroids
- Two regimens are used i.e
- MOPP
Oncorin/ vincristine------------------- day 1 and 8
Procarbazine------------------- day 1 and 14
Predisone------------------- day I and 14
- ABVD
Bleomycin------------------ day 1 and 15
Vinblastin------------------ day 1 and 15
Decarbazine------------------ day 1 and 15
- Nursing care is based on pancytopenia (A condition in which there is a lower-than-normal number of red and white blood cells and platelets in the blood.) and other drug effects
- Psychological support
- Nutrition support
- Regular hygiene to prevent infections
| Condition & Assessment | Interventions |
|---|---|
|
Neutropenia (Low WBCs/Risk of Infection) Assessment: Monitor ANC, temperature (q4h), signs of infection (chills, redness, swelling, sore throat). |
|
|
Thrombocytopenia (Low Platelets/Risk of Bleeding) Assessment: Monitor platelets, observe for bleeding (petechiae, purpura, epistaxis, hematuria, melena). Neuro status. |
|
|
Anemia (Low RBCs/Fatigue) Assessment: Monitor Hb/Hct, fatigue, pallor, dyspnea, tachycardia. |
|
| Condition & Assessment | Interventions |
|---|---|
|
Nausea and Vomiting Assessment: Frequency, severity, triggers. |
|
|
Mucositis/Stomatitis (Oral Sores) Assessment: Inspect mucosa daily for redness/lesions. Assess pain. |
|
|
Diarrhea/Constipation Assessment: Bowel habits, consistency. |
|
| Condition & Assessment | Interventions |
|---|---|
|
Fatigue Assessment: Severity, impact on ADLs. |
|
|
Peripheral Neuropathy Assessment: Numbness, tingling, burning, weakness. |
|
|
Skin Reactions (Radiation) Assessment: Redness, dryness, itching, peeling. |
|
|
Alopecia Assessment: Discuss expectations/emotional impact. |
|
| Complication & Assessment | Interventions |
|---|---|
|
Tumor Lysis Syndrome (TLS) Assessment: Electrolytes (K+, Phos, Ca), Uric acid, cardiac arrhythmias, muscle cramps, decreased urine output. |
|
|
Superior Vena Cava (SVC) Syndrome Assessment: Facial/neck edema, dyspnea, distended neck veins. |
|
|
Infections (Opportunistic) Assessment: Assess for fungal/viral infections. |
|
- Emotional Distress: Provide empathetic support, encourage verbalization, refer to support groups. Address body image changes (wigs, self-worth). Teach coping mechanisms.
- Patient Education: Disease/treatment plan, medication management, self-care strategies, signs to report (fever, bleeding), follow-up care, nutrition/hydration.
- Pain Management: Assess pain. Administer analgesics. Non-pharmacological methods.
- Sleep Promotion: Optimize environment, consistent times, sleep aids if prescribed.
Management of Non Hodgkin’s disease
Specialists who treat non-Hodgkin lymphoma include hematologists, medical oncologists, radiation oncologists, oncology nurses and a registered dietitian. The choice of treatment depends mainly on the following:- The type of non-Hodgkin lymphoma
- Stage of lymphoma
- How quickly the cancer is growing (whether it is indolent or aggressive lymphoma)
- Age of the patient
- Other patient’s health problems
- If a patient has indolent non-Hodgkin lymphoma without symptoms, treatment for the cancer is not initiated immediately. The treatment team watches the patient’s health closely so that treatment can start when symptoms begin
- Indolent lymphoma with symptoms needs chemotherapy and biological Radiation therapy may be used for people with Stage I or Stage II lymphoma
- In aggressive lymphoma, the treatment is usually chemotherapy and biological therapy People with lymphoma that comes back after treatment may receive high doses of chemotherapy, radiation therapy, or both, followed by stem cell transplantation
2. Chemotherapy uses drugs to kill cancer cells throughout the body; drug can be administered by oral route, intravenous or into spinal cord in phases depending on the cancer stage and nature of the drug. Drugs in initial stage cyclophosphamide and chlorambucil In recurrence CDVP (cyclophosphamide, doxorubicin, vincristine and prednisone) or CVPP (cyclophoshamide, vinchristine, procarbozine and prednisone) Side effects poor appetite, nausea and vomiting, diarrhea, trouble swallowing, or mouth and lip sores, hair loss, infections, bruise or bleeding easily, skin rashes or blisters, headaches, weakness and tiredness
3.Biological therapy:
- People with certain types of non-Hodgkin lymphoma may have biological therapy. This type of treatment helps the immune system fight cancer.
- Flu-like symptoms such as fever, chills, headache, weakness, and nausea may Most side effects are easy to treat. Rarely, a person may have more serious side effects, such as breathing problems, low blood pressure, or severe skin rashes.
4. Radiation therapy/ radiotherapy: uses high-energy rays to kill lymphoma cells. It can shrink tumors and help control Two types of radiation therapy are used for people with lymphoma:
- External radiation: A large machine aims the rays at the part of the body where lymphoma cells have collected. This is local therapy because it affects cells in the treated area only. Most people go to a hospital or clinic for treatment 5 days a week for several
- Systemic radiation: Some people with lymphoma receive an injection of radioactive material that travels throughout the body. The radioactive material is bound to monoclonal antibodies that seek out lymphoma The radiation destroys the lymphoma cells.
- External radiation to abdomen can cause nausea, vomiting, and diarrhea, on chest and neck there may be dry sore throat and difficult in swallowing, the skin may become red, dry, and People who get systemic radiation also may feel very tired, get infections and above signs worsen
5.Stem cell transplantation: If lymphoma returns after treatment, stem cell transplantation is considered. A transplant of blood-forming stem cells allows a patient to receive high doses of chemotherapy, radiation therapy, or both. The high doses destroy both lymphoma cells and healthy blood cells in the bone marrow. Transplant given through a flexible tube placed in a large vein in the neck or chest area after heavy chemotherapy. New blood cells develop from the transplanted stem cells. The stem cells may come from body of the patient (Autologous stem cell transplantation) or a donor who is a brother, sister or parent (Allogeneic stem cell transplantation) and Syngeneic stem cell transplantation for identical twins Supportive care aims at controlling pain and other symptoms, to relieve the side effects of therapy and to help the patient cope with the diagnosis. It includes
6. Nutrition: give calories to maintain a good weight, protein to keep promote strength. Eating well may help the patient feel better and have more
7. Activity: Walking, swimming, and other activities can keep the patient strong and Exercise may reduce nausea and pain and make treatment easier to handle. It also can help relieve stress
8. Follow-Up Care: regular checkups after treatment for non-Hodgkin The health team watches patient’s recovery closely and check for recurrence of the lymphoma. Checkups monitors change in health and treatment needs of the patient. Checkups may include a physical exam, lab tests, chest x-rays, and other procedures.
9. Social support: this can be provided by Doctors, nurses, and other members of the health care team who answer many questions about patient’s treatment, working, or other procedures.
Social workers can suggest resources for financial aid, transportation, home care, or emotional support. Support groups like patients or family members meet with other patients or their families to share what they have learned about coping with the disease and the effects of treatment. Groups may offer support in person, over the telephone, or on the Internet. A patient may want to talk with a member of the health care team about finding a support group.
10. Treat treatment side effects appropriately
- Helicobacter pylori is treated with antibiotics
- Surgical: this corrects stricture and obstruction
- Encourage bladder training , habit retraining and intake of oral fluids