Table of Contents
ToggleAnticonvulsants
Anticonvulsants / antiepileptic drugs are a type of drugs that are used to prevent or treat seizures or convulsions by controlling abnormal electrical activity in the brain.
Common Terms
- Absence seizure: type of generalized seizure that is characterized by sudden, temporary loss of consciousness, sometimes with staring or blinking for 3 to 5 seconds; formerly known as a petit mal seizure
- Antiepileptic: drug used to treat the abnormal and excessive energy bursts in the brain that are characteristic of epilepsy.
- Convulsion: tonic–clonic muscular reaction to excessive electrical energy arising from nerve cells in the brain.
- Epilepsy: collection of various syndromes, all of which are characterized by seizures.
- Generalized seizure: seizure that begins in one area of the brain and rapidly spreads throughout both hemispheres
- Partial seizures: also called focal seizures; seizures involving one area of the brain that do not spread throughout the entire body.
- Seizure: sudden discharge of excessive electrical energy from nerve cells in the brain
- Status epilepticus: state in which seizures rapidly recur; most severe form of generalized seizure
- Tonic–clonic seizure: type of generalized seizure that is characterized by serious clonic–tonic muscular reactions and loss of consciousness, with exhaustion and little memory of the event on awakening; formerly known as a grand mal seizure
A seizure is a sudden burst of uncontrolled electrical activity in the brain that occurs when neurons become excessively active.
Seizures can be generally classified into two major groups depending on where they begin in the brain;
- Focal seizures affect initially only a portion of the brain typically one hemisphere and may occur with or without impairment of awareness.
- Generalized seizures affect both sides of the brain at the same time and almost always cause loss of consciousness.
Seizures can be viewed as the result of an imbalance between inhibitory and excitatory processes in the brain that produces either too little inhibition or too much excitation.
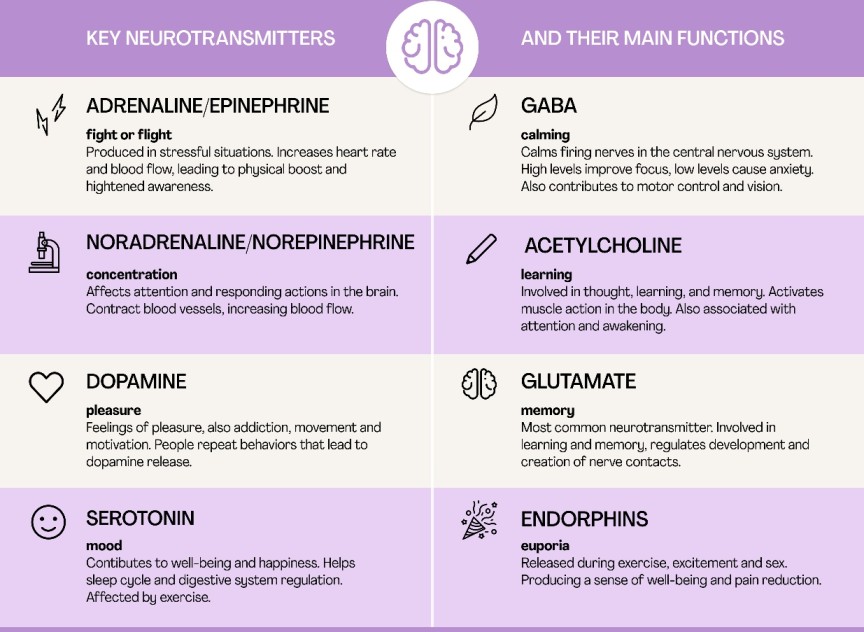
Inhibition and Excitation neurotransmitters.
- Excitatory. Excitatory neurotransmitters “excite” the neuron and cause it to “fire off the message,” meaning, the message continues to be passed along to the next cell. Examples of excitatory neurotransmitters include glutamate, epinephrine and norepinephrine.
- Inhibitory. Inhibitory neurotransmitters block or prevent the chemical message from being passed along any farther. Gamma-aminobutyric acid (GABA), glycine and serotonin are examples of inhibitory neurotransmitters.
- Modulatory. Modulatory neurotransmitters influence the effects of other chemical messengers. They “tweak” or adjust how cells communicate at the synapse. They also affect a larger number of neurons at the same time.
DRUGS FOR TREATING GENERALIZED SEIZURES
Hydantoins
- Ethotoin
- Fosphenytoin
- Phenytoin
Barbiturates and Barbiturate-Like Drugs
- Mephobarbital
- Phenobarbital
- Primidone
Benzodiazepines
- Clonazepam
- Diazepam
Succinimides
- Ethosuximide
- Methsuximide
Oxazolidinediones
- Trimethdiaone
- Paramethadione
Sulfonamides
- Acetazolamide
- Zonisamide
Valproates / Valproic Acid Derivatives.
- Valproic acid
- Sodium Valproate
- Divalproex sodium
DRUGS FOR TREATING PARTIAL SEIZURES
Carboxamides
- Carbamazepine
- Oxcarbazepine
Gaba analogs
- Pregabalin
- Gabapentin
Triazines
- Lamotrigine
Fructose derivatives
- Topiramate
DRUGS FOR TREATING GENERALIZED SEIZURES
Drugs typically used to treat generalized seizures stabilize the nerve membranes by blocking channels in the cell membrane or altering receptor sites.
Because they work generally on the central nervous system (CNS), sedation and other CNS effects often result. Various drugs are used to treat generalized seizures, including hydantoins, barbiturates, barbiturate-like drugs, benzodiazepines, and succinimides. These drugs affect the entire brain and reduce the chance of sudden electrical
outburst.
Hydantoins
Hydantoins include ethotoin (Peganone), phenytoin (Dilantin). Because hydantoins are generally less sedating than many other antiepileptics, they may be the drugs of choice for patients who are not willing to
tolerate sedation and drowsiness. They do have significant adverse effects; thus, less toxic drugs, such as benzodiazepines, have replaced them in many situations.
Indications of Hydantoins
- Treatment of tonic–clonic and psychomotor seizures.
- Short-term control of status epilepticus, prevention of seizures after neurosurgery.
Dose
Phenytoin
- Adult: 100 mg Orally t.d.s., up to 300–400 mg/d; 10–15 mg/kg IV
- Children: 5–8 mg/kg per day Orally; 5–10 mg/kg IV in divided doses
Contraindications of Hydantoins
- Presence of allergy to any of these drugs to avoid hypersensitivity reactions.
- Are associated with specific birth defects and should not be used in pregnancy or lactation unless the risk of seizures outweighs the potential risk to the fetus.
- Women of childbearing age should be urged to use barrier contraceptives while taking these drugs.
Adverse effects
- Nystagmus
- ataxia
- slurred speech
- depression
- confusion
- drowsiness
- lethargy
- fatigue
- constipation
- dry mouth
- anorexia
- cardiac arrhythmias and changes in blood pressure
- urinary retention
- loss of libido.
Barbiturates and Barbiturate-Like Drugs
The barbiturates and barbiturate-type drugs inhibit impulse conduction in the ascending reticular activating system (RAS), depress the cerebral cortex, alter cerebellar function, and depress motor nerve output. They stabilize nerve membranes throughout the CNS directly by influencing ionic channels in the cell membrane, thereby decreasing excitability and hyperexcitability to stimulation.
Indications
- Treatment of tonic–clonic and absence seizures.
- Are also used as anxiolytic/hypnotic agent.
- Emergency control of status epilepticus and acute seizures associated with eclampsia, tetanus, and other conditions.
- Treatment of cortical focal seizures
Dose
Phenobarbital
- Adult: 60–100 mg/d Orally; 200–320 mg IM or IV for acute episodes, may be repeated in 6 hours; reduce dose with elderly and with renal or hepatic impairment.
- Children: 3–6 mg/kg per day Orally; 4–6 mg/kg per day IM or IV; 15–20 mg/kg IV over 10–15 min for status epilepticus.
Contraindications, Adverse effects, same as hydantoins
Benzodiazepines
The benzodiazepines may potentiate the effects of GABA, an inhibitory neurotransmitter that stabilizes nerve cell membranes. These drugs, which appear to act primarily in the limbic system and the RAS, also cause muscle relaxation and relieve anxiety without affecting cortical functioning substantially. The benzodiazepines stabilize nerve membranes throughout the CNS to decrease excitability and hyperexcitability to stimulation.
Indications
- Treatment of absence and myoclonic seizures.
- Treatment of severe convulsions, clonic–tonic seizures, status epilepticus; treatment of alcohol withdrawal and tetanus
- Relieves tension, preoperative anxiety.
- Administered to patients who do not respond to succinimides.
- Being studied for use in the treatment of panic attacks, restless leg movements during sleep, hyperkinetic dysarthria(where you have difficulty speaking because the muscles you use for speech are weak), acute manic episodes, multifocal tic disorders, and neuralgias.
Dose
Diazepam
- Adult: 2–10 mg Orally b.d. to q.i.d.; or 0.2 mg/kg PRN, may repeat in 4–12 h, 2–20 mg IM or IV
- Geriatric or debilitated patients: 2–2.5 mg, Orally b.d.; or 2–5 mg IM or IV.
- Pediatric: 1–2.5 mg Orally t.d.s to q.i.d.; or 0.3–0.5 mg/kg
Contraindications and adverse effects for benzodiazepines are the same as those
discussed for hydantoins.
DRUGS FOR TREATING PARTIAL SEIZURES
Partial seizures may be simple (involving only a single muscle or reaction) or complex (involving a series of reactions or emotional changes. Drugs used in the treatment of partial seizures include carbamazepine. Some of the drugs used to treat generalized seizures have also been found to be useful in treating partial seizures
The drugs used to control partial seizures stabilize nerve membranes in either of two ways—directly, by altering sodium and calcium channels, or indirectly, by increasing the activity of GABA, an inhibitory neurotransmitter, and thereby decreasing excessive activity.
Carbamazepine and oxcarbazepine are used as monotherapy, and the
remaining drugs are used as adjunctive therapy
Carbamazepine
Indications
- Drug of choice for treatment of partial seizures and tonic–clonic seizures.
- Treatment of trigeminal neuralgia, bipolar disorder.
Dose
- Adult: 800–1200 mg/d Orally in divided doses 6–8 hourly.
- Pediatric (> 12 yr): adult doses, do not exceed 1000 mg/d
- Pediatric (6–12 yr): 20–30 mg/kg per day Orally in divided doses t.d.s to q.i.d.
- Pediatric (<6 yr): 35 mg/kg per day Orally
Gabapentin
Indications
- Used as adjunct in treating partial seizures
- Treatment of postherpetic pain in adults and children ages 3–12 yr of age, migraines, bipolar disorders
- Treatment of tremors of multiple sclerosis, and nerve-generated
pain states
Dose
- Adult: 900–1800 mg/d Orally in divided doses t.d.s
- Pediatric (3–12 yr): 10–15 mg/kg per day Orally in divided doses.
Contraindications
Contraindications to the drugs used to control partial seizures include the following conditions:
- presence of any known allergy to the drug
- bone marrow suppression, which could be exacerbated by the drug effects
- severe hepatic dysfunction, which could be exacerbated and could interfere with the metabolism of the drugs.
- Pregnancy; Carbamazepine, clorazepate, gabapentin, and oxcarbazine have been shown to be dangerous to a fetus and should not be used during pregnancy. Women of childbearing age should be advised to use contraception.
- Lactation; These drugs enter breast milk and can cause serious adverse effects in the baby. If any of these drugs is needed during lactation, another method of feeding the baby should be used.
Adverse Effects
- drowsiness
- fatigue
- weakness
- confusion
- headache
- insomnia
- GI depression, with nausea, vomiting, and anorexia
- upper respiratory infections.
- can also be directly toxic to the liver and the bone marrow, causing dysfunction.
Nursing Considerations for Patients Receiving Anticonvulsants.
- Assess for contraindications and cautions: any known allergies to these drugs to avoid hypersensitivity reactions,
- Assess for history of bone marrow suppression or renal stones, which could be exacerbated by these drugs
- History of renal or hepatic dysfunction that might interfere with drug metabolism and excretion.
- Assess for current status of pregnancy or lactation, which are contraindicated or require caution when using these drugs.
- Inspect the skin for color and lesions to determine evidence of possible skin effects;
- Assess pulse and blood pressure and auscultate heart to evaluate for possible cardiac effects;
- Assess level of orientation, affect, reflexes, and bilateral grip strength to evaluate any CNS effects;
- Monitor bowel sounds and urine output to determine possible gastrointestinal or genitourinary effects.
- Assess the patient’s renal and liver function, including renal and liver function tests, to determine the appropriateness of therapy and determine the need for possible dose adjustment.
- Monitor the results of laboratory tests such as urinalysis and CBC with differential to identify changes in bone marrow function.
Nursing Diagnoses
Nursing diagnoses related to drug therapy might include the following:
- Acute Pain related to GI and CNS effects
- Disturbed Thought Processes related to CNS effects
- Risk for Injury related to CNS effects
- Risk for Infection related to bone marrow suppression effects
- Deficient Knowledge regarding drug therapy
Implementation With Rationale
- Administer the drug with food to alleviate GI irritation if GI upset is a problem.
- Monitor CBC before and periodically during therapy to detect and prevent serious bone marrow suppression.
- Protect the patient from exposure to infection if bone marrow suppression occurs.
- Discontinue the drug if skin rash, bone marrow suppression, unusual depression, or personality changes occur to prevent further serious adverse effects.
- Discontinue the drug slowly, and never withdraw the drug quickly, because rapid withdrawal may precipitate seizures.
- Arrange for counseling for women of childbearing age who are taking these drugs. Because these drugs have the potential to cause serious damage to the fetus, women should understand the risk of birth defects and use barrier contraceptives to avoid pregnancy
- Provide safety measures to protect the patient from injury or falls if CNS changes occur.
- Provide patient teaching, including drug name and prescribed dosage, as well as measures for avoidance of adverse effects, warning signs that may indicate possible problems, and the need for periodic laboratory testing and monitoring and evaluation to enhance patient knowledge about drug therapy and to promote
compliance.
Evaluation
- Monitor patient response to the drug (decrease in incidence or absence of seizures).
- Monitor for adverse effects (CNS changes, GI depression, bone marrow suppression, severe dermatological reactions,
liver toxicity, renal stones). - Evaluate the effectiveness of the teaching plan (patient can give the drug name and dosage and name possible adverse effects to watch for and specific measures to prevent them; patient is aware of the risk of birth defects and the need to carry information about the diagnosis and use of this drug).
- Patients being treated with antiepileptic are often on long term therapy, which requires compliance with their drug regimen and restrictions associated with their disorder and the drug effects. Educate the patients about this.
MULTIPLE CHOICE QUESTIONS
Select the best answer to the following.
- When teaching a group of students about epilepsy, which of the following should the nurse include?
a. Always characterized by grand mal seizures.
b. Only a genetic problem.
c. The most prevalent neurological disorder.
d. The name given to one brain disorder. - Which of the following would the nurse be least likely to include as a type of generalized seizure?
a. Petit mal seizures.
b. Febrile seizures.
c. Grand mal seizures.
d. Complex seizures. - Which instruction would the nurse encourage a patient receiving an antiepileptic drug to do?
a. Give up his or her driver’s license.
b. Carry a Medical form identification.
c. Take antihistamines to help dry up secretions.
d. Keep the diagnosis a secret to avoid prejudice. - Drugs that are commonly used to treat grand mal seizures include;
a. barbiturates, benzodiazepines, and hydantoins.
b. barbiturates, antihistamines, and local anesthetics.
c. hydantoins, phenobarbital, and phensuximide.
d. benzodiazepines, phensuximide, and valproic acid. - The drug of choice for the treatment of partial seizures is
a. valproic acid.
b. methsuximide.
c. carbamazepine.
d. ethosuximide. - Focal or partial seizures
a. start at one point and spread quickly throughout the brain.
b. are best treated with benzodiazepines.
c. involve only part of the brain.
d. are easily diagnosed and recognized. - One drug that is used alone in the treatment of partial seizures is
a. carbamazepine.
b. topiramate.
c. lamotrigine.
d. gabapentin. - Treatment of epilepsy is directed at
a. blocking the transmission of nerve impulses into the
brain.
b. stabilizing overexcited nerve membranes
c. blocking peripheral nerve terminals.
d. thickening the meninges to dampen brain electrical activity.

I want to answere the questions
I need some quiz other wise it was agood topic
I need some questions
This is so helpful
I really appreciate