Changes in the newborn at birth
Changes in the newborn at birth are a number of changes that an infant’s body undergoes to allow it to survive outside the womb and adapt to life in a new environment.
During intrauterine life, the fetus receives oxygen and nutrients by absorption through the placenta. It does not use its lungs or the digestive organs. Similarly, it excretes carbon dioxide and other waste products through placental structures into the mother’s blood.
It is protected from many harmful factors/organisms by the placenta, and it is kept in a warm environment.
Size and Growth: The term infant weighs about 3000g. Boys weigh approximately 250g more than girls. Infants of less than 2500g are classified as ‘low birth.’ During the first 3–5 days, up to 10% of birth weight is lost. This is regained by 7–10 days. In the first month, average weight gain per week is 200g.
Skin: The newborn skin is immature, with a thin epithelial layer and incompletely developed sweat and sebaceous glands. Combined with the high surface area to body mass ratio, this renders the baby prone to heat and water losses. Numerous benign skin lesions occur, e.g. a greasy protective layer, the vernix caseosa.
Temperature Regulation: The neonate has a low metabolic activity resulting in a poor ability to produce heat. The infant enters a much cooler environment than to which it is used. Its body is wet and thus liable to lose heat through evaporation. Receptors on the baby’s skin send messages to the brain that the baby’s body is cold. The baby’s body then creates heat by shivering and by burning stores of brown fat, a type of fat found only in fetuses and newborns.
Head: The average occipito-frontal head circumference is 35 cm. Two soft spots or fontanels are present. The anterior fontanel closes at 18 months of age, and the posterior closes by 6–8 weeks.
Respiratory System: Changes that occur at birth allow the newborn to convert from dependence on the placenta to breathing air for the exchange of respiratory gases. In utero, the airways and lungs are filled with fluid that contains surfactant. The lung fluid is removed by the squeezing of the thorax during vaginal delivery and by reduced secretion and increased absorption mediated by fetal catecholamine during labor and after birth. Surfactant lines the air–fluid interface of the alveoli and reduces the surface tension, thereby facilitating lung expansion. This is associated with a fall in pulmonary vascular resistance. The rate is variable and normally ranges between 30 and 60 breaths/min. Brief self-limiting apnoeic spells might occur during sleep.
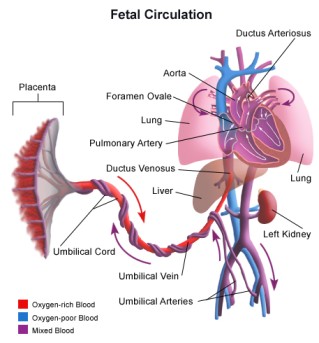
Cardiovascular System: Major changes in the lungs and circulation allow adaptation to extra-uterine life. In the fetal circulation, the right-sided (pulmonary) pressure exceeds the left-sided (systemic) pressure. Blood flows from right to left through the foramen ovale and ductus arteriosus. At birth, these relationships reverse: Left-sided (systemic) pressure rises with clamping of umbilical vessels. Right-sided (pulmonary) pressure falls as the lungs expand, and the rising pressure triggers a prostaglandin-mediated vasodilatation. The foramen ovale and ductus arteriosus close functionally shortly after birth. The ductus closes due to muscular contraction in response to rising oxygen tension.
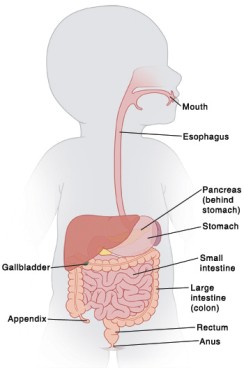
Gastrointestinal System: At term, the secretory and absorbing surfaces are well developed, as are digestive enzymes, with the exception of pancreatic amylase. Meconium is usually passed within 6 hrs, and delay beyond 24 hrs is considered abnormal. Normally, meconium is replaced by yellow stool by day 3-4.
Liver: In the fetus, the liver acts as a storage site for sugar (glycogen) and iron. When the baby is born, the liver has various functions: It produces substances that help the blood to clot. It begins breaking down waste products such as excess red blood cells. It produces a protein that helps break down bilirubin. Immaturity of the liver enzymes responsible for conjugation of bilirubin is responsible for the ‘physiological jaundice’ which can occur from the second day of life.
Genitourinary System: The infant should void within the first 24 hours of life.
Immune System: The neonatal immune system is incomplete compared to older children and adults: Impaired neutrophil reserves. Diminished phagocytosis and intracellular killing capacity. Decreased complement components. Low IgG2, leading to infections with organisms. The presence of maternal antibody in babies born greater than 30 weeks’ gestational age provides some protection against infection.
Central Nervous System: The central nervous system (CNS) is relatively immature at birth. Newborn infants sleep for a total of 16–20 hours each day. The touch of a nipple on the baby’s face initiates the sequence of rooting and the complex coordination of lip, tongue, palate, and pharynx required for sucking and swallowing. Crying (without tears) is the main means of communication.

