Furunculosis refers to the condition characterized by the recurrent or multiple presence of furuncles (also known as boils).
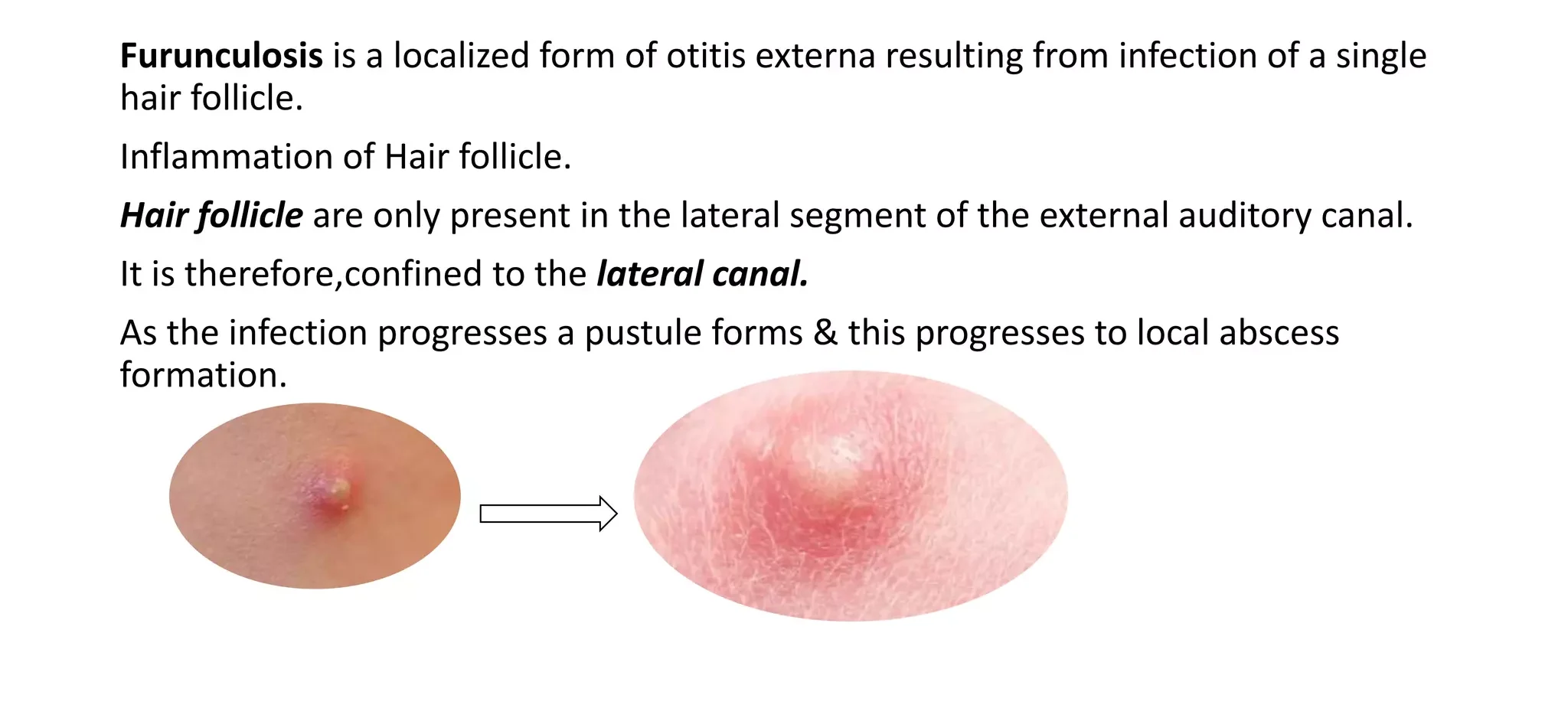
A furuncle (or boil) is an acute, deep-seated, red, hot, tender nodule that develops in a hair follicle, usually resulting from bacterial infection. It begins as a painful, firm papule (small, raised bump) and evolves into a larger, fluctuating, pus-filled lesion with a necrotic (dead tissue) core that eventually ruptures or is incised, expelling pus and necrotic material.
- Folliculitis: A superficial inflammation of the hair follicle, often less severe and not as deep as a furuncle. A furuncle can develop from an untreated or progressing folliculitis.
- Carbuncle: A deeper and more extensive infection involving multiple adjacent hair follicles, forming a cluster of interconnected furuncles with multiple draining heads. Carbuncles are typically larger, more painful, and often associated with systemic symptoms (e.g., fever, malaise). Furunculosis, when it involves multiple lesions or recurrence, can sometimes involve carbuncles.

Furunculosis of the external ear canal refers to the development of one or more furuncles (boils) within the hair-bearing skin of the cartilaginous portion of the external auditory canal. It is a localized, acute, and painful infection originating in a hair follicle and its associated sebaceous gland within the ear canal.
- An ear furuncle presents as a painful, red, swollen nodule inside the ear canal. As the infection progresses, it fills with pus, leading to a "head" that may spontaneously rupture, draining purulent material.
- This condition is a form of folliculitis that has progressed deeply, creating an abscess within the hair follicle.
The primary cause of furunculosis of the external ear canal is a bacterial infection of a hair follicle.
- Staphylococcus aureus: This bacterium is by far the most common causative organism. It is a common commensal (normal inhabitant) of the skin and nasal passages, but can become pathogenic when there's a break in the skin barrier or impaired local immunity.
- Less commonly, other bacteria like Streptococcus pyogenes may be involved.
These factors either introduce bacteria into the ear canal or create an environment conducive to bacterial growth and infection.
- Self-inflicted Trauma: This is perhaps the most significant risk factor.
- Improper Ear Cleaning: Using cotton swabs (Q-tips), fingernails, hairpins, pen caps, or other sharp objects to clean or scratch the ear canal can cause micro-abrasions or small cuts in the delicate skin.
- Scratching: Intense itching (e.g., due to eczema, allergies, or fungal infections) can lead to scratching and subsequent skin breakdown.
- Instrumentation: Ill-fitting hearing aids, earplugs, or earbud headphones can cause chronic irritation or minor trauma.
- Swimming ("Swimmer's Ear"): Prolonged exposure to water can lead to maceration (softening and breakdown) of the ear canal skin, making it more permeable to bacteria. It can also wash away protective cerumen.
- Humid Climates: Living in a hot, humid environment can increase sweating and moisture in the ear.
- Lack of Cerumen (Earwax): Cerumen has protective antibacterial and antifungal properties. Excessive cleaning or conditions that reduce cerumen can remove this natural barrier.
- Dermatological Conditions: Conditions like eczema, psoriasis, or seborrheic dermatitis affecting the ear canal can compromise the skin barrier and increase susceptibility to infection.
- Diabetes Mellitus: Individuals with diabetes are more prone to infections, including skin infections, due to impaired immune function and higher glucose levels which can support bacterial growth.
- Immunocompromised States: Conditions that weaken the immune system (e.g., HIV/AIDS, chemotherapy, long-term corticosteroid use) increase the risk of infections.
- Malnutrition: Poor nutritional status can impact immune response.
The pathophysiology of an ear furuncle involves a sequence of events, starting with bacterial invasion and progressing through inflammation, pus formation, and eventual resolution. It is essentially a deep infection of a hair follicle.
- Predisposing Event (Initiation):
- The process typically begins with a breach in the integrity of the hair follicle or surrounding skin. This is most commonly due to minor trauma, such as scratching the ear canal with a fingernail, inserting foreign objects (e.g., cotton swabs), or irritation from hearing aids.
- This trauma creates a microscopic entry point for bacteria.
- Other factors like maceration from excessive moisture can also weaken the skin barrier, making it more permeable.
- Bacterial Invasion and Colonization:
- Once the skin barrier is compromised, opportunistic bacteria, overwhelmingly Staphylococcus aureus, which are common inhabitants of the skin (especially the nasal vestibule and external ear), invade the hair follicle.
- The bacteria begin to multiply within the warm, moist, and nutrient-rich environment of the hair follicle.
- Inflammatory Response:
- The host's immune system recognizes the invading bacteria and initiates an acute inflammatory response.
- Vasodilation: Blood vessels in the area dilate, increasing blood flow, which causes the characteristic redness (erythema) and warmth.
- Increased Capillary Permeability: Fluid, proteins, and immune cells (neutrophils, macrophages) leak from the capillaries into the surrounding tissue, leading to swelling (edema) and tenderness.
- Pain: The swelling and inflammatory mediators (e.g., prostaglandins, bradykinin) stimulate nerve endings, causing significant pain, which is particularly severe in the confined, rigid cartilaginous portion of the external ear canal.
- Abscess Formation (Pus Development):
- As the infection progresses, neutrophils aggressively attack the bacteria. Both live and dead bacteria, dead neutrophils, tissue debris, and inflammatory exudate accumulate, forming pus.
- This collection of pus, walled off by the body's immune response, forms an abscess within the hair follicle – this is the core of the furuncle.
- The furuncle typically starts as a red, firm, tender papule or nodule and then becomes more fluctuant (soft and compressible) as pus accumulates.
- Necrotic Core: The intense inflammation and bacterial toxins can lead to localized tissue death (necrosis) within the center of the furuncle, forming a "core" or "plug."
- Maturation and Resolution:
- The furuncle continues to enlarge and become more painful until it "points" – a visible head of pus develops on the surface.
- Spontaneous Rupture or Incision: Eventually, the pressure from the accumulated pus leads to the spontaneous rupture of the furuncle, discharging the pus and necrotic core. Alternatively, it may be surgically incised and drained.
- Drainage: Once the pus is drained, the pain typically subsides rapidly as the pressure is relieved.
- Healing: Following drainage, the inflammatory response subsides, and the remaining cavity heals by granulation and re-epithelialization. Scarring may or may not occur, depending on the depth and severity of the infection.
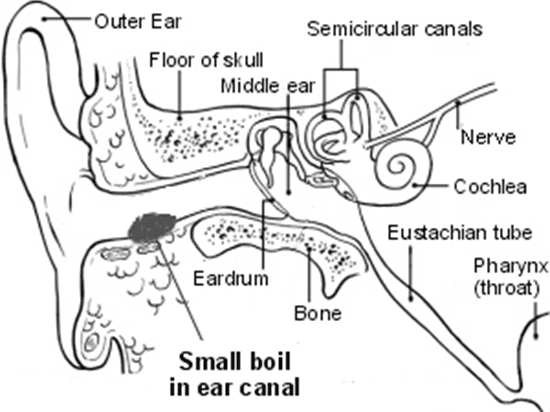
Furuncles in the external ear canal are specifically limited to the areas where hair follicles are present.
The external ear canal is divided into two main parts:
- Cartilaginous Portion (Outer One-Third): This is the outer, more elastic part of the ear canal, continuous with the auricle (the visible part of the ear).
- This is the primary site for ear furuncles.
- This section is lined with skin that contains hair follicles, sebaceous glands (produce oil), and ceruminous glands (produce earwax).
- Furuncles occur here because this is where the hair follicles, which are the origin of the infection, are located.
- The skin in this area is thicker and more prone to trauma from self-cleaning or foreign objects.
- Bony Portion (Inner Two-Thirds): This is the inner, rigid part of the ear canal, leading up to the tympanic membrane (eardrum).
- Furuncles generally DO NOT occur in the bony portion.
- The skin lining this section is very thin, tightly adherent to the bone, and lacks hair follicles and sebaceous glands. Therefore, the primary structures necessary for furuncle formation are absent here.
- Infections in this part of the ear canal are more likely to be diffuse otitis externa (swimmer's ear), which is a broader inflammation of the skin lining.
The clinical manifestations of an ear furuncle are primarily local and characterized by symptoms related to inflammation and pressure within the confined space of the ear canal.
- Intensity: Pain is typically intense, throbbing, and constant. It is disproportionately severe compared to the size of the lesion due to the unyielding cartilaginous walls of the ear canal.
- Aggravating Factors: The pain is significantly exacerbated by:
- Chewing or talking: Movement of the temporomandibular joint (jaw) near the ear canal.
- Touching the tragus or auricle: Especially pulling on the pinna (outer ear) or pressing on the tragus (the small cartilaginous flap in front of the ear canal). This is a key diagnostic sign that differentiates it from otitis media.
- Inserting anything into the ear.
- Radiation: Pain may radiate to the jaw, temple, or neck.
- Localized Swelling: A visible or palpable localized swelling or bump may be present within the outer ear canal.
- Diffuse Swelling: In severe cases, the swelling can be extensive enough to occlude the ear canal, and may even cause some edema of the surrounding periauricular tissues.
- Tenderness: The area around the furuncle is exquisitely tender to touch.
- Localized Redness and Swelling: An otoscopic examination will reveal a well-demarcated, often bright red, painful, and tender swelling or nodule within the cartilaginous portion of the external ear canal. The skin overlying the furuncle will be inflamed.
- Presence of a "Head" or Pustule: As the furuncle matures, a yellowish or whitish "head" (pustule) may become visible at the center of the swelling, indicating the collection of pus. A black "core" of necrotic tissue might also be seen.
- Spontaneous Rupture and Drainage: A mature furuncle may spontaneously rupture, releasing a small amount of purulent (pus-filled) and sometimes bloody discharge into the ear canal. This often brings significant pain relief.
- Normal Tympanic Membrane (usually): In an isolated furuncle, the tympanic membrane (eardrum) typically appears normal unless there is an underlying or coexisting otitis media (which is less common). However, visualization of the tympanic membrane may be difficult or impossible due to the severe swelling of the ear canal.
- Low-grade fever
- Malaise
- Regional lymphadenopathy: Swelling and tenderness of lymph nodes around the ear (preauricular or postauricular).
The diagnosis of an ear canal furuncle is primarily clinical, based on a thorough history and physical examination. Laboratory tests are usually not required unless there are unusual circumstances or concerns about systemic involvement.
- Onset and Nature of Pain:
- Sudden onset of severe, localized ear pain.
- Exacerbation of pain with jaw movement (chewing, talking), and especially with manipulation of the auricle or tragus.
- The pain is often described as throbbing.
- Associated Symptoms:
- Sensation of ear fullness or blockage.
- Any hearing changes (usually transient conductive hearing loss).
- Presence of discharge (if the furuncle has ruptured).
- Any systemic symptoms like fever or malaise (less common).
- Predisposing Factors:
- Recent history of ear canal trauma (e.g., using cotton swabs, scratching with fingernails, inserting foreign objects).
- Recent swimming or water exposure.
- History of dermatological conditions affecting the ear (e.g., eczema).
- Underlying medical conditions, especially diabetes mellitus or immunocompromise.
- Previous episodes of ear furuncles.
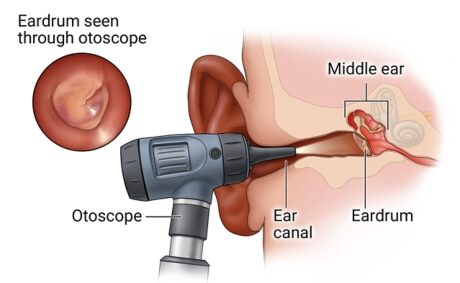
This is the cornerstone of diagnosis.
- External Ear (Auricle and Periauricular Area):
- Inspection for any redness, swelling, or tenderness around the ear.
- Palpation of the tragus and pinna: Exquisite tenderness upon manipulation of the tragus or pulling the auricle upwards and outwards is a classic sign of external otitis, including furunculosis.
- Check for regional lymphadenopathy (swollen lymph nodes) in the preauricular or postauricular areas.
- Otoscopy (Examination of the Ear Canal and Tympanic Membrane):
- Visualization: Using an otoscope, the examiner will carefully inspect the external auditory canal. This can be challenging due to pain and swelling.
- Key Findings:
- Localized Redness and Swelling: A discrete, red, swollen, and very tender lesion will be seen in the cartilaginous (outer one-third) portion of the ear canal.
- Pustule/Head: A yellowish-white "head" (pustule) may be visible at the apex of the swelling, indicating the collection of pus. A central "core" might also be noted.
- Ear Canal Occlusion: The furuncle may be large enough to partially or completely occlude the ear canal, making visualization of the tympanic membrane difficult or impossible.
- Tympanic Membrane: If visible, the tympanic membrane usually appears normal, which helps differentiate furunculosis from acute otitis media (where the eardrum would be bulging, red, and possibly perforated).
- Culture and Sensitivity Testing:
- Not routinely performed for uncomplicated furuncles.
- May be considered in cases of recurrent furunculosis, unresponsive to standard treatment, in immunocompromised patients, or if there's concern about unusual pathogens or antibiotic resistance. A swab of any discharge or material obtained after incision and drainage would be sent to the lab.
- Blood Tests:
- Complete Blood Count (CBC): Usually not necessary. May show a mild elevation in white blood cells (leukocytosis) in severe cases or with systemic involvement, but this is rare for a localized furuncle.
- Blood Glucose: If diabetes is suspected or known to be poorly controlled, blood glucose or HbA1c levels may be checked as diabetes is a significant risk factor for recurrent infections.
It's important to differentiate an ear furuncle from other conditions that cause ear pain and swelling, such as:
- Diffuse Otitis Externa: More generalized inflammation of the ear canal skin, less localized pain.
- Acute Otitis Media: Infection behind the eardrum, usually with bulging and red eardrum, pain not typically exacerbated by tragal pressure.
- Mastoiditis: Infection of the mastoid bone, characterized by pain, swelling, and redness behind the ear.
- Perichondritis: Infection of the cartilage of the outer ear.
The primary goals of treatment are to relieve pain, eradicate the infection, facilitate drainage of pus, and prevent recurrence. Treatment involves a combination of local measures, pain control, and antibiotics.
- Pain Relief: Due to the severe pain, adequate analgesia is crucial from the outset.
- Drainage: Promoting the drainage of pus is key to resolving the infection.
- Antibiotics: To target the bacterial infection.
- Local Measures: To reduce inflammation and promote healing.
- Analgesia (Pain Management):
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter options like ibuprofen or naproxen are often effective for mild to moderate pain and also help reduce inflammation.
- Acetaminophen (Paracetamol): Can be used alone or in combination with NSAIDs.
- Stronger Analgesics: In cases of severe pain, especially initially, prescription analgesics (e.g., opioids) may be necessary, but usually for a short duration.
- Local Heat Application:
- Warm Compresses: Applying warm, moist compresses to the outer ear can help to reduce pain, promote vasodilation, and encourage the furuncle to "point" and drain spontaneously. This should be done carefully to avoid burning the skin.
- Antibiotics:
- Topical Antibiotics (Limited Role): Topical antibiotic creams or ointments (e.g., fusidic acid, mupirocin) may be applied if the furuncle is very small and superficial, but their penetration into a deep-seated infection is often limited. They are more effective after drainage.
- Systemic Antibiotics (Oral): These are the mainstay of antibiotic treatment, especially given that Staphylococcus aureus is the primary pathogen.
- Choice of Antibiotic:
- Antistaphylococcal Penicillins: Dicloxacillin or flucloxacillin (where available).
- First-generation Cephalosporins: Cephalexin.
- Clindamycin or Trimethoprim-sulfamethoxazole (TMP-SMX): These are good alternatives, particularly if Methicillin-Resistant Staphylococcus aureus (MRSA) is suspected or prevalent in the community, or if the patient is penicillin-allergic.
- Duration: Typically a 7-10 day course, but this can vary based on severity and response to treatment.
- Indications for Systemic Antibiotics: All but the most superficial and resolving furuncles. Particularly indicated for larger furuncles, those with surrounding cellulitis, patients with systemic symptoms (fever), immunocompromised individuals, or diabetics.
- Choice of Antibiotic:
- Thorough cleaning of the ear by wicking
- Then, apply an antibiotic like chloramphenicol ear drops 0.5% 2 drops 8hrly for 14 days.
- If severe, add Caps cloxacillin 250-500mgs QID for 5 days, In children 12.5-25mgs per kg body weight.
- Steroids like betamethasone ear drops
- Analgesics for pain like PCT Ig tds for 3 days or Ibuprofen
- You can also use warm icepacks to relieve pain
- If the cause is fungal; Use clotrimazole solution apply O.D for 4-8 Weeks Or Fluconazole 200mg O.D for 10 days.
- Proper drying the ear by ear wicking is very important
- Incision and Drainage (I&D):
- Indication: This is often the most effective treatment for a mature, fluctuant furuncle. Once a furuncle has "pointed" and formed a collection of pus, surgical incision and drainage provides immediate pain relief by decompressing the abscess and removes the source of infection.
- Procedure:
- Local anesthetic is injected around the furuncle.
- A small incision is made at the most fluctuant or pointed part of the furuncle.
- Pus and necrotic debris are drained.
- A small wick or packing may be inserted into the cavity to ensure continued drainage and prevent premature closure. This is usually removed within 24-48 hours.
- Culture: If drainage is performed, a sample of pus can be sent for culture and sensitivity testing, especially in recurrent or recalcitrant cases.
- Local Debridement/Wick Placement (Post-Drainage):
- After drainage, the ear canal may be gently cleaned.
- A small piece of gauze or an ear wick impregnated with an antibiotic (e.g., polymyxin B/neomycin/hydrocortisone) may be placed to keep the canal open, promote drainage, and deliver topical antibiotics.
- Avoid Manipulation: Advise the patient to strictly avoid inserting anything into the ear canal (e.g., cotton swabs, fingers) to prevent further trauma and re-infection.
- Keep Ear Dry: During the healing phase, advise the patient to keep the ear dry when showering or bathing (e.g., by using cotton wool lightly smeared with petroleum jelly).
- Identify and Address Risk Factors:
- Diabetes Control: For diabetic patients, optimizing blood glucose control is crucial.
- Skin Conditions: Manage underlying dermatological conditions like eczema.
- Hygiene: Emphasize proper ear hygiene and avoidance of trauma.
- Nasal Decolonization (for recurrent cases): If recurrent furunculosis is a problem, the patient may be a nasal carrier of Staphylococcus aureus. Mupirocin nasal ointment applied to the nostrils twice daily for a few days can help decolonize the nose and reduce the source of infection.
- Follow-up is important to ensure the infection is resolving and to remove any wicks.
- Monitor for complications.
Based on the clinical manifestations and pathophysiology,
- Acute Pain related to inflammation, tissue swelling, and pressure from the furuncle within the confined ear canal, evidenced by patient's report of severe ear pain, facial grimacing, guarding behavior, and tenderness on palpation of the tragus/auricle.
- Risk for Infection (Spread or Recurrence) related to compromised skin integrity (due to trauma, drainage), presence of Staphylococcus aureus, and potential for inadequate self-care practices.
- Impaired Comfort related to ear pain, swelling, and potential hearing impairment, evidenced by patient's restlessness, difficulty sleeping, or expressed frustration.
- Inadequate health Knowledge regarding disease process, treatment regimen, ear hygiene, and prevention of recurrence, evidenced by patient's questions, inaccurate statements, or observed ineffective self-care practices.
- Disrupted Body Image (potentially) related to visible swelling or discharge from the ear, particularly if prolonged or recurrent, evidenced by patient's verbalizations about appearance or social withdrawal (less common for a single furuncle, but possible).
- Risk for Impaired Hearing related to obstruction of the external auditory canal by swelling or discharge.
| Intervention | Rationale |
|---|---|
| Assess pain regularly | Use a pain scale (e.g., 0-10) to monitor intensity, quality, and aggravating/alleviating factors. Rationale: Provides objective data for pain management and effectiveness of interventions. |
| Administer prescribed analgesics | Provide NSAIDs, acetaminophen, or stronger pain medications as ordered. Rationale: Reduces pain and inflammation, improving patient comfort. |
| Apply warm compresses to the affected ear | As prescribed or directed, ensuring the temperature is safe and not too hot. Rationale: Promotes vasodilation, reduces inflammation, and encourages localization/drainage of the furuncle, offering symptomatic relief. |
| Educate patient on positioning | Advise resting with the affected ear elevated or avoiding direct pressure on it. Rationale: Reduces pressure on the inflamed area, potentially lessening pain. |
| Minimize manipulation of the ear | Instruct patient to avoid touching, rubbing, or inserting anything into the affected ear. Rationale: Prevents further irritation and exacerbation of pain. |
| Intervention | Rationale |
|---|---|
| Administer prescribed oral antibiotics | Ensure patient understands the importance of completing the full course of antibiotics, even if symptoms improve. Rationale: Eradicates the bacterial infection, preventing spread and recurrence. |
| Educate on proper ear hygiene | Instruct patient to avoid inserting cotton swabs, fingers, or other objects into the ear canal. Rationale: Prevents trauma to the delicate skin, which is a primary entry point for bacteria. |
| Emphasize hand hygiene | Before and after touching the ear area, especially if drainage is present. Rationale: Prevents introduction of new pathogens or spread of existing ones. |
| Instruct on keeping the ear dry | Advise using cotton balls lightly coated with petroleum jelly during showering/shampooing. Rationale: Excessive moisture can macerate skin and promote bacterial growth. |
| Monitor for signs of worsening infection | Redness, increased swelling, fever, increased pain, or purulent discharge. Rationale: Early detection allows for prompt adjustment of treatment. |
| For draining furuncles | Instruct on gentle cleaning of exudate from the external ear, avoiding forcing anything into the canal. Rationale: Maintains cleanliness and prevents crusting which can impede drainage. |
| Intervention | Rationale |
|---|---|
| Provide a quiet and calm environment | Minimize external stimuli that might heighten discomfort. Rationale: Promotes rest and reduces stress associated with pain. |
| Offer diversional activities | As appropriate and tolerated by the patient. Rationale: Distracts from pain and discomfort. |
| Encourage rest | Advise patient to get adequate rest to aid in healing. Rationale: Body uses energy for healing during rest. |
| Address hearing changes | Reassure patient that temporary hearing loss due to canal obstruction is common and will likely resolve with treatment. Rationale: Reduces anxiety and provides accurate information. |
| Intervention | Rationale |
|---|---|
| Explain the disease process | Use simple language to describe what a furuncle is, its cause, and how it's treated. Rationale: Empowers the patient to understand their condition and adhere to the treatment plan. |
| Provide detailed instructions on medication | Include name, dosage, frequency, route, potential side effects, and importance of completing the full course. Rationale: Ensures safe and effective medication use. |
| Demonstrate and reinforce ear care techniques | Show patient how to apply warm compresses or keep the ear dry, if applicable. Rationale: Promotes proper self-care. |
| Discuss prevention strategies | Emphasize avoiding ear canal trauma (e.g., no cotton swabs), managing underlying conditions (e.g., diabetes control), and keeping the ears dry. Rationale: Reduces the risk of recurrence. |
| Identify signs and symptoms requiring medical attention | Explain when to contact a healthcare provider (e.g., worsening pain, fever, spreading redness, no improvement). Rationale: Ensures timely intervention for complications or treatment failure. |
| Provide written instructions | Supplement verbal teaching with written materials. Rationale: Reinforces learning and provides a reference for the patient. |
| Intervention | Rationale |
|---|---|
| Assess hearing status | Note any reports of hearing loss. Rationale: Establishes baseline and monitors for improvement or worsening. |
| Reassure patient | Explain that hearing loss is typically temporary due to canal obstruction and will likely improve as swelling subsides and drainage occurs. Rationale: Reduces patient anxiety. |
| Encourage communication strategies | Advise speaking clearly and facing the patient if hearing is significantly impaired. Rationale: Facilitates effective communication despite temporary hearing impairment. |
- Regularly assess the patient's pain level and comfort.
- Monitor for signs of infection resolution or worsening.
- Evaluate patient's understanding of care instructions and adherence to the treatment plan.


Types of epistax and the differences
Anterior Epistaxis: This is the most common type of nosebleed and originates from the front part of the nasal septum. The septum is the thin wall of tissue that separates the two nostrils. Anterior nosebleeds are usually less severe and easier to control.
Posterior Epistaxis: This type of nosebleed originates from the back part of the nasal cavity, often deeper within the nose. Posterior epistaxis is less common but can be more challenging to manage due to the blood flow originating from larger blood vessels.
Traumatic Epistaxis: Nosebleeds caused by trauma or injury to the nose are known as traumatic epistaxis. This could result from a direct blow to the nose, accidental injury, or medical procedures.
Spontaneous Epistaxis: Spontaneous nosebleeds occur without any apparent external cause. They might be related to underlying medical conditions such as hypertension, blood clotting disorders, or inflammatory conditions like sinusitis.
Recurrent Epistaxis: When nosebleeds occur frequently over time, they are termed recurrent epistaxis. This could be due to chronic irritation, dryness of the nasal mucosa, or other underlying health issues.
Idiopathic Epistaxis: In some cases, nosebleeds have no identifiable cause and are referred to as idiopathic epistaxis. This term is used when the underlying reason for the nosebleed remains unclear even after medical evaluation.
Ts a great one ,,well discussed
Nursing interventions
Help me with the nursing interventions n nursing care plan
Ineed nurses interventions
Supperb
So benefiting.but describe management of a patient with prolonged epistaxis for 24hrs
Nursing care plan
Is it appropriate to put cold compress behind the head region,coz I have so fur seen several incidents where that is applied
well elaborated,isn’t silver nitrate used in nasal cauterization too?
what is the mode of action of TEO in relation to stoping nasal bleeding like as mentioned in the above notes ? otherwise the notes are so precise👏
Good noted ✅️