HYDROCELE
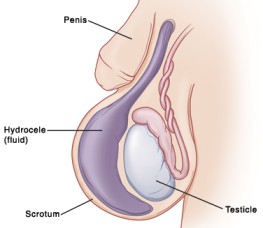
A hydrocele is a fluid collection within the tunica vaginalis of the scrotum or along the spermatic cord.
A hydrocele is accumulation of serous fluid within the tunica vaginalis that produces swelling in the inguinal region or scrotum.
It often presents as painless swelling in the scrotum. Provided there is no hernia present, hydrocoeles below the age of 1 year usually resolve spontaneously.
In infants it is usually as a result of incomplete closure of the processus vaginalis. It may or may not be associated with inguinal hernia. In older boys and men it may be idiopathic.
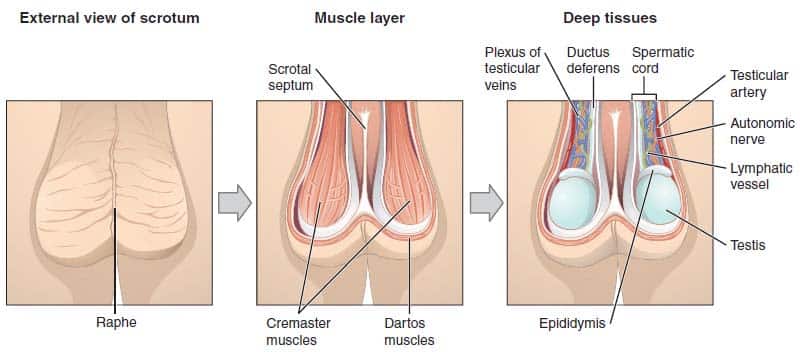
Anatomy of the Scrotum.
Scrotum, is a thin external sac of skin that is divided into two compartments; each compartment contains one of the two testes, the glands that produce sperm, and one of the epididymis, where the sperm is stored.
- The function of the scrotum is to protect the testes and to keep them at a temperature below the normal body temperature. The scrotum thus protrudes from the body wall. When contracted, it conserves heat; while relaxed it is smooth and elongated, permitting the circulation of air that effects cooling. The relatively cool temperature of the scrotum is thought to be important for the production of viable sperm.
- A vertical septum of subcutaneous tissue in the center divides it into two parts, each containing one testis.
- Smooth muscle fibers, called the dartos muscle, in the subcutaneous tissue contract to give the scrotum its wrinkled appearance. When these fibers are relaxed, the scrotum is smooth.
- The cremaster muscle consists of skeletal muscle fibers and controls the position of the scrotum and testes. When it is cold or a man is sexually aroused, this muscle contracts to pull the testes closer to the body for warmth.

Etiology/Causes of a Hydrocele
The causes of hydrocele can be categorized into four main factors:
- Excessive production of fluid within the sac: This occurs when there is an overproduction of fluid within the sac surrounding the testicle e.g. in acute/chronic epididymo-orchitis.
- Defective absorption of fluid: This refers to a situation where the normal absorption of fluid within the sac is impaired, leading to the accumulation of fluid e.g. in testicular tumors, Hematocele.
- Interference with lymphatic drainage of scrotal structures: Certain conditions, such in case of elephantiasis, torsion of testis, can disrupt the normal drainage of lymphatic fluid from the scrotal area, resulting in the development of a hydrocele.
- Connection with a hernia of the peritoneal cavity: In the congenital variety, a hydrocele may be associated with a hernia of the peritoneal cavity, leading to the presentation of a hydrocele of the cord e.g. in patent tunica vaginalis.
Risk Factors
- Direct Injury or inflammation of the testes
- Prematurity
- Testicular tumors
- Infections in the testicle or the epididymitis
Pathophysiology
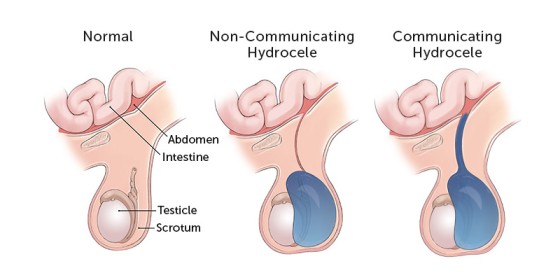
- During the seventh month of fetal development, the testicles move from the abdomen into the scrotum.
- When the testicle travels downward, a remnant piece of peritoneum wrapped around the testicle, called the tunica vaginalis and this allows fluid present in the abdominal cavity to surround the testicle.
- This sac usually closes before birth, preventing additional fluid from going from the abdomen into the scrotum, and the fluid is gradually absorbed within the first year of life.
- When the sac remains open tunica vaginalis is patent and connects with the general peritoneal cavity leading to development of a communicating Hydrocele.
- The communication is usually too small to allow herniation of intra-abdominal contents. Digital pressure on the Hydrocele does not usually empty it, but the Hydrocele fluid may drain into the peritoneal cavity when the child is lying down.
Types of hydrocele
Non-communicating Hydrocele
- Here there is no connection between the abdominal cavity and the sac around the testicle in the scrotum.
- This type of Hydrocele is often found in newborns and these often resolve or go away over time.
- It may take up to one year for this to happen, but as long as the swelling is decreasing, it can be safely observed.
Communicating Hydrocele
- Here the sac does not close and this means that the fluid around the testicle can flow back up into the abdomen.
- It is noticeable that the Hydrocele looks smaller early in the day and larger in the evening; the pressure changes cause the fluid to flow back into the abdomen.
CLASSIFICATIONS OF HYDROCELES
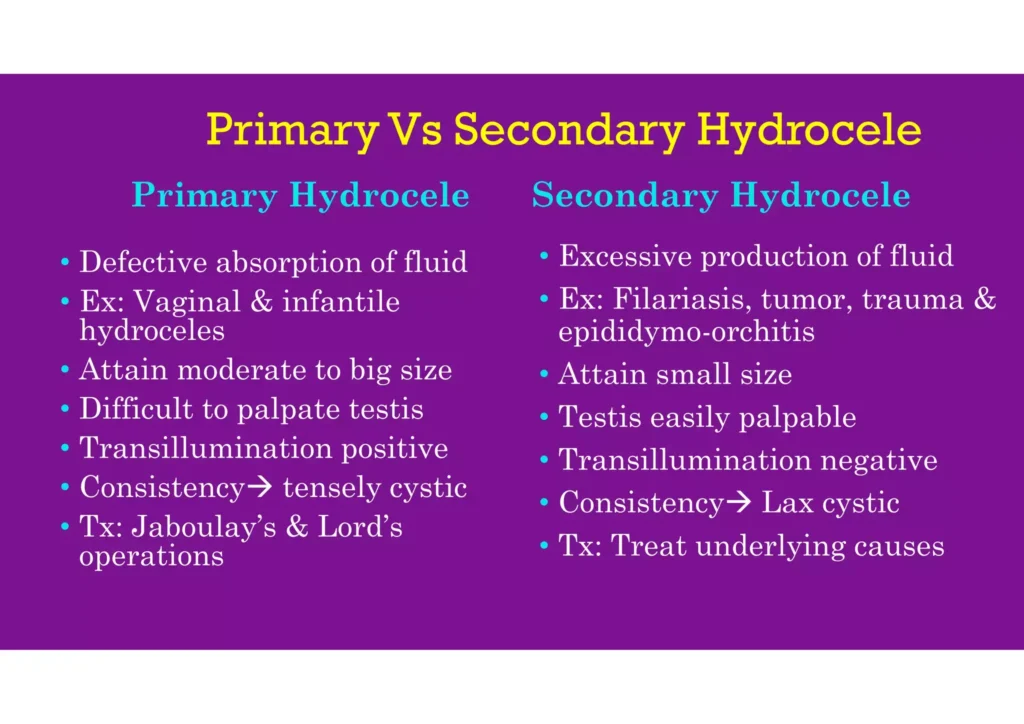
Primary hydrocele: A primary hydrocele is characterized by a soft, painless swelling that is usually large in size and makes it difficult to feel the testis. Transillumination can demonstrate the presence of fluid. Although these hydroceles are often asymptomatic, their large size can cause inconvenience and, if left untreated, may lead to atrophy of the testis due to compression or obstruction of blood supply. Early diagnosis during a complete physical examination may reveal small hydroceles in which the testis can be easily palpated within a lax hydrocele. However, in cases where the hydrocele sac is dense, ultrasound imaging is necessary to visualize the testis and reveal any underlying abnormalities. Primary hydroceles are usually painless, similar to testicular tumors.
A common method of diagnosing a primary hydrocele is through transillumination, where shining a strong light through the enlarged scrotum will pass light in the case of a primary hydrocele, while a tumor will not, except in the case of a malignancy with reactive hydrocele.
Its subdivided into four types.
Congenital Hydrocele:
- Occurs when the processus vaginalis, a tube-like structure connecting the abdomen to the scrotum, remains open and communicates with the peritoneal cavity.
- This allows peritoneal fluid to move, but the opening is usually too small to allow intra-abdominal contents to herniate through.
- When pressure is applied to the hydrocele, it usually does not empty, but the fluid may drain into the peritoneal cavity when the individual is lying down.
- The swelling cannot be felt above the inguinal ring, resembling a hernia.
Infantile Hydrocele:
- Occurs when the processus vaginalis becomes closed at the level of the deep inguinal ring, but the portion beyond it remains open, allowing fluid to accumulate.
- This condition is not exclusive to infants and can also occur in adults.
- The swelling cannot be felt above the inguinal ring.
Encysted Hydrocele of the Cord:
- In this type, both the proximal and distal portions of the processus vaginalis become closed off, while the central portion remains open, leading to the accumulation of fluid within it.
- This results in a smooth oval swelling near the spermatic cord, which can be mistaken for an inguinal hernia.
- When the testis is gently pulled downwards, the swelling moves downwards and becomes less mobile.
Vaginal Hydrocele (in females):
- In females, a related condition known as a “hydrocele of the canal of Nuck” can occur.
- This occurs when the canal of Nuck, the equivalent structure to the processus vaginalis in males, fails to close properly, leading to the development of a hydrocele.
- This condition may present as a swelling in the groin or labia majora.
Secondary hydrocele: A secondary hydrocele arises from an underlying condition, such as infections (e.g., filariasis, tuberculosis of the epididymis, syphilis), trauma or injury (e.g., post herniorrhaphy hydrocele or malignancy).
- Secondary hydroceles are generally smaller, with the exception of those caused by filariasis, which can lead to very large hydroceles.
- Testicular infarction, microlithiasis of the testicle, and lithiasis of tunica vaginalis can also contribute to the development of secondary hydroceles.
- Testicular diseases, including cancer, trauma (e.g., hernia), and orchitis (inflammation of the testis), can result in secondary hydroceles. They may also occur in infants undergoing peritoneal dialysis. It is important to note that a hydrocele is not a cancerous condition, but clinical evaluation is needed if a testicular tumor is suspected, as there are no documented cases associating hydroceles with testicular cancer in the world literature.
Secondary hydroceles are most commonly linked with acute or chronic epididymo-orchitis and are also observed with testicular torsion and certain testicular tumors. Commonly, a secondary hydrocele is soft and moderately sized, and the underlying testis can be felt. The secondary hydrocele usually resolves when the primary condition is treated.
Other predisposing factors for secondary hydroceles include acute/chronic epididymo-orchitis, testicular torsion, testicular tumors, hematocele, filarial hydrocele, post herniorrhaphy, and hydrocele of a herniated sac.

Diagnosis and Investigations
Through Clinical Presentation: A primary hydrocele is described as having the following characteristics/presentations.
Clinical Presentation.
- Fluctuating Size: The swollen area may vary in size, being smaller in the morning and larger later in the day. This fluctuation is known as a positive fluctuation test.
- Discomfort: Patients may experience discomfort due to the heaviness of the swollen scrotum.
- Scrotal Swelling: Hydroceles can present as painless unilateral or bilateral scrotal swelling.
- Transillumination: When examined with a focused beam of light, the scrotum transilluminates, displaying a uniform glow without any internal shadows. Transillumination positive.
- Impulse on Coughing: In most cases, the impulse on coughing is negative, although it may be positive in congenital hydroceles.
- Reducibility: Hydroceles are usually non-reducible, meaning they cannot be easily pushed back into the abdomen. Reducibility absent.
- Palpable Fullness: Upon examination, hydroceles present as a soft, non-tender fullness within the scrotum, which can be felt. Testis cannot be palpated separately. (exception – funicular hydrocele, encysted hydrocele)
Investigations and Diagnostic Findings
- Laboratory studies. laboratory studies may be indicated to exclude other surgical or medical conditions that may be in the differential diagnosis.
- Ultrasonography. Ultrasonography provides excellent detail of the testicular parenchyma; spermatoceles can be clearly distinguished from hydroceles on sonograms, a testicular tumor can also be identified.
- Duplex ultrasonography. Duplex studies provide information regarding testicular blood flow when a hydrocele may be associated with chronic torsion.
- Plain abdominal radiography. Plain radiography may be useful for distinguishing an acute hydrocele from a hernia.
Management and Treatment of Hydroceles
- Observation for Infants: Most hydroceles appearing in the first year of life often resolve without treatment and therefore require only observation.
- Surgical Removal: Hydroceles that persist after the first year or occur later in life may require surgical removal through a procedure known as hydrocelectomy, as they have little tendency towards regression. The method of choice for surgical removal is an open operation under general or spinal anesthesia for adults, and general anesthesia for children. Local infiltration anesthesia is not recommended due to its inability to relieve abdominal pain caused by traction on the spermatic cord.
- Aspiration Precautions: If a testicular tumor is suspected, a hydrocele should not be aspirated, as this can lead to the dissemination of malignant cells. Ultrasonography should be used to clinically exclude the presence of a tumor. If no tumor is present, the hydrocele fluid can be aspirated with a needle and syringe.
- Post-operative Care: After surgery, the scrotum should be supported, and ice bags can be used to alleviate pain. Regular changes of surgical dressings, observation of drainage, and monitoring for complications are necessary to prevent re-operation.
- Complications Management: In cases with the presence of complications, open operation with or without orchiectomy may be preferred, depending on the severity of the complications.
- Jaboulay’s Procedure: After aspiration of a primary hydrocele, fluid reaccumulates over the following months, necessitating periodic aspiration or operation. For younger patients, operation is usually preferred, while the elderly or unfit can have aspirations repeated whenever the hydrocele becomes uncomfortably large. Sclerotherapy is an alternative method, involving the injection of 6% aqueous phenol with 1% lidocaine for analgesia, which can inhibit reaccumulation. Multiple treatments may be necessary.
- Aspiration and Sclerosing Agents: Aspiration of the hydrocele contents and injection with sclerosing agents, sometimes with tetracyclines, can be effective but is often very painful. However, these alternative treatments are generally regarded as unsatisfactory due to the high incidence of recurrences and the frequent necessity for repetition of the procedure.
Surgical Management.
The surgical management of hydroceles can be approached in several ways, including inguinal, scrotal, and sclerotherapy methods.
- Inguinal Approach: This method involves ligation of the processus vaginalis high within the internal inguinal ring and is mostly the preferred procedure for pediatric hydroceles. In cases where a testicular tumor is detected on testicular ultrasonography, an inguinal approach with high control/ligation of the cord structures is necessary.
- Scrotal Approach: The scrotal approach includes excision or eversion and suturing of the tunica vaginalis and is recommended for chronic noncommunicating hydroceles. However, this approach should be avoided if there is any suspicion of underlying malignancy.
- Sclerotherapy: An additional adjunctive, if not definitive procedure is scrotal aspiration and sclerotherapy of the scrotum using tetracycline or doxycycline solutions. It’s important to note that recurrence after sclerotherapy is common, as is significant pain and epididymal obstruction, making this treatment a last resort in poor surgical candidates with symptomatic hydroceles and in men in whom fertility is no longer an issue.
- Hydrocelectomy: This surgical procedure aims to excise the hydrocele sac or reconfigure the remnant of the tunica vaginalis to allow lymphatic drainage via scrotal lymphatics. This method may be considered in cases where other surgical approaches have not been successful.
Nursing Interventions
The nursing interventions appropriate for the child are:
- Health education. Provide preoperative education, including a visit with OR personnel before surgery when possible. Discuss anticipated things that may concern the patient, such as masks, lights, IVs, BP cuff, electrodes, the feel of oxygen cannula or mask on nose or face, autoclave and suction noises, and the possibility of the child crying. Additionally, involve the child in age-appropriate discussions about the surgical procedure and encourage the expression of feelings and concerns.
- Pre, Intra and Post operative care:
Pre-Operative Care:
- Patient Assessment: Conduct a thorough assessment of the patient’s medical history, current health status, and any allergies. This includes obtaining baseline vital signs, laboratory tests, and diagnostic imaging as required.
- Education: Provide the patient with information about the upcoming surgery, including preoperative instructions, potential risks, and what to expect during the recovery period.
- Medication Management: Review the patient’s current medications and ensure appropriate management, including any required adjustments or discontinuations prior to surgery.
- Psychological Support: Offer emotional support and address any anxiety or concerns the patient may have about the surgery.
- Preparing the Surgical Site: Ensure the surgical site is properly prepared and sterile, including hair removal if necessary.
Intra-Operative Care:
- Patient Positioning: Assist with positioning the patient on the operating table to ensure optimal access for the surgical team.
- Monitoring: Continuously monitor the patient’s vital signs, including heart rate, blood pressure, oxygen saturation, and ECG, and respond to any changes promptly.
- Sterile Technique: Assist the surgical team in maintaining a sterile environment and provide the necessary equipment and supplies as required.
- Anesthesia Management: Collaborate with the anesthesiologist to ensure the patient’s comfort and safety during the administration of anesthesia.
- Communication: Facilitate effective communication between the surgical team and other healthcare professionals, and provide support and reassurance to the patient throughout the procedure.
Post-Operative Care:
- Recovery Monitoring: Monitor the patient’s vital signs, pain levels, and consciousness as they recover from anesthesia.
- Pain Management: Administer prescribed pain medications and assess the patient’s pain levels regularly, providing comfort measures as needed.
- Wound Care: Monitor the surgical site for any signs of infection or complications, and provide appropriate wound care as directed by the surgical team.
- Mobilization: Encourage early mobilization and assist the patient with repositioning to prevent complications such as deep vein thrombosis and pressure ulcers.
- Patient Education: Provide the patient and their family with postoperative instructions, including information on medication management, activity restrictions, and signs of potential complications.
- Emotional Support: Offer emotional support to the patient and their family, addressing any concerns and providing reassurance during the recovery process.
3. Reduce risk for infection. Verify that preoperative skin, scrotal, and bowel cleansing procedures have been completed as needed depending on the specific surgical procedure. Apply a sterile dressing to prevent environmental contamination of the fresh wound. Administer antibiotics as indicated and ensure proper hand hygiene and aseptic techniques during care.
4. Monitor fluid volume. Measure and record intake and output, including tubes and drains. Monitor vital signs, noting changes in blood pressure, heart rate and rhythm, and respirations. Gradually resume oral intake as indicated, ensuring the child remains well-hydrated.
5. Relief from pain. Regularly evaluate the child’s pain, noting its characteristics, location, and intensity on a 0–10 scale. Assess and address any anxiety or fear related to the procedure. Identify and address any causes of discomfort other than the operative procedure. Provide additional comfort measures, such as backrubs, heat or cold applications, and age-appropriate distraction techniques. Administer pain medication as prescribed and assess the effectiveness of pain relief measures. Encourage the child to communicate their pain and comfort needs.
6. Promote mobility. Encourage early mobilization and ambulation as tolerated postoperatively to prevent complications such as deep vein thrombosis and promote circulation and respiratory function.
7. Monitor for complications. Assess for signs of postoperative complications such as infection, bleeding, or adverse reactions to anesthesia or medications. Monitor surgical incision sites for signs of inflammation, drainage, or other abnormalities.
8. Encourage adequate nutrition. Provide the child with a balanced and nutritious diet to support the healing process. Offer small, frequent meals if the child’s appetite is reduced and encourage fluid intake to prevent dehydration.
9. Collaborate with the interdisciplinary team. Work closely with the surgical team, child life specialists, and other healthcare professionals to ensure comprehensive care for the child. Communicate any concerns or changes in the child’s condition promptly.
10. Provide age-appropriate activities. Offer age-appropriate activities and play opportunities to promote the child’s emotional well-being and assist with their recovery. Arrange for appropriate entertainment and distraction to alleviate anxiety and boredom during hospitalization.

Complications of Hydroceles
- Hematocele Formation: Hematocele, a collection of blood within the sac, can occur due to spontaneous bleeding into the sac or as a result of trauma. If not drained, it may lead to the formation of a clotted hematocele.
- Calcification of the Sac: The sac may calcify, leading to the formation of a clotted hydrocele, often resulting from a slow, painless ooze of blood into the tunica vaginalis. This can make it difficult to differentiate from a testicular tumor.
- Postherniorrhaphy Hydrocele: A relatively rare complication of inguinal hernia repair, possibly due to disruption of the lymphatics draining the scrotal contents.
- Infection and Pyocele: Infection may lead to the formation of pyocele, a collection of pus within the sac.
- Testicular Atrophy: Long-standing cases of hydrocele may lead to atrophy of the testis.
- Rupture: Rupture of the sac may occur due to trauma or spontaneously. In some cases, absorption of the fluid may lead to a cure.
- Herniation: In long-standing cases, the hydrocele sac may herniate through the dartos muscle.
Test Questions
1. Which of the following applies to the defect emerging from residual peritoneal fluid confined within the lower segment of the processus vaginalis?
A. Inguinal hernia
B. Incarcerated hernia
C. Communicating hydrocele
D. Noncommunicating hydrocele
1. Answer: D. Noncommunicating hydrocele
- Option D: With a noncommunicating hydrocele, most commonly seen at birth, residual peritoneal fluid is trapped within lower segment of the processus vaginalis (the tunica vaginalis). There is no communication with the peritoneal cavity and the fluid usually is absorbed during the first months after birth.
- Option A: An inguinal hernia arises from the incomplete closure of the processus vaginalis leading to the descent of an intestinal portion.
- Option B: Incarceration occurs when the hernia becomes tightly caught in the hernia sac.
- Option C: A communicating hydrocele usually is associated with an inguinal hernia because the processus vaginalis remains open from the scrotum to the abdominal cavity.
2. An infant with hydrocele is seen in the clinic for a follow-up visit at 1 month of age. The scrotum is smaller than it was at birth, but fluid is still visible on illumination. Which of the following actions is the physician likely to recommend?
A. Massaging the groin area twice a day until the fluid is gone.
B. Referral to a surgeon for repair.
C. No treatment is necessary; the fluid is reabsorbing normally.
D. Keeping the infant in a flat, supine position until the fluid is gone.
2. Answer: C. No treatment is necessary; the fluid is reabsorbing normally.
- Option C: A hydrocele is a collection of fluid in the scrotum that results from a patent tunica vaginalis; illumination of the scrotum with a pocket light demonstrates the clear fluid; in most cases, the fluid reabsorbs within the first few months of life and no treatment is necessary.
- Options A and D: Massaging the area or placing the infant in a supine position would have no effect.
- Option B: Surgery is not indicated.
3. Nurse Jeremy is evaluating a client’s fluid intake and output record. Fluid intake and urine output should relate in which way?
A. Fluid intake should be double the urine output.
B. Fluid intake should be approximately equal to the urine output.
C. Fluid intake should be half the urine output.
D. Fluid intake should be inversely proportional to the urine output.
3. Answer: B. Fluid intake should be approximately equal to the urine output.
- Option B: Normally, fluid intake is approximately equal to the urine output. Any other relationship signals an abnormality.
- Option A: Fluid intake that is double the urine output indicates fluid retention
- Option C: Fluid intake that is half the urine output indicates dehydration.
- Option D: Normally, fluid intake isn’t inversely proportional to the urine output.
4. When explaining to the parents of a child with hydrocele about the possible cause of the condition, the nurse bases this explanation on the interpretation that hydrocele is most likely the result of which of the following:
A. Blockage in the inguinal canal.
B. Failure of the upper part of the processus vaginalis to atrophy.
C. A patent processus vaginalis that results in the collection of fluid along the spermatic cord.
D. An obliterated processus vaginalis that allows fluid to accumulate in the scrotal sac.
4. Answer: C. A patent processus vaginalis that results in the collection of fluid along the spermatic cord.
- Option C: A hydrocele is a fluid collection within the tunica vaginalis of the scrotum or along the spermatic cord.
- Options A, B, C: These processes does not occur in hydrocele.
5. Shortly after an infant is returned to his room following hydrocele repair, the infant’s mother tells the nurse that the child’s scrotum looks swollen and bruised. Which of the following responses by type nurse is the most appropriate?
A. “Let me see if the doctor has ordered aspirin for him. If he did, I’ll get it right away.”
B. “Why don’t you wait in his room? Then you can ask me any questions when I get there.”
C. “What you are describing is unusual after this type of surgery. I’ll let the doctor know.”
D. “This is normal after this type of surgery. Let’s look at it together just to be sure.”
5. Answer: D. “This is normal after this type of surgery. Let’s look at it together just to be sure.”
- Option D: Swelling and bruising of the surgical site is a usual occurrence right after the surgery. Elevation of the scrotal area and anti-inflammatory agents can be administered as ordered by the physician.
- Option A: Aspirin is not the drug of choice given for pediatric patients.
- Option B: Answering questions could relieve the anxiety felt by the family and the patient.
- Option C: Swelling and bruising are normal occurrences for the patient after the surgery.

Thank you so much for this great help of questions, notes and everything.
Understandable
Am greatful
Thank you very much this topic is very enjoyable
thanks bro
for the great work done