Immunological Agents
Immunological agents are a broad class of drugs that modify the immune system’s activity, either by enhancing or suppressing its function.
They are like tools that help your immune system work better or differently. For example, vaccines help your body fight off specific diseases(enhancing) or autoimmune drugs treat autoimmune diseases, where the immune system attacks the body’s own tissues (suppressing).
Types of Immunological Agents:
- Immunostimulants: These are drugs that boost the immune system’s function, often used when the immune system is weakened or underperforming.
- Immunosuppressants: These drugs reduce or suppress the immune system’s activity, essential in preventing transplant rejection and treating autoimmune diseases.
IMMUNE STIMULANTS
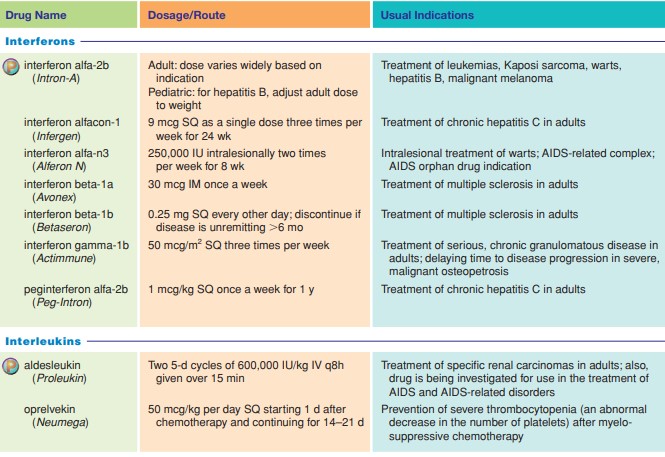
Interferons
interferon alfa-2b
interferon alfacon-1
interferon alfa-n3
interferon beta-1a
interferon beta-1b
interferon gamma-1b
peginterferon alfa-2a
peginterferon alfa-2b
Interleukins
aldesleukin
oprelvekin
IMMUNE SUPPRESSANTS
T- and B-Cell Suppressors
abatacept
alefacept
azathioprine
Interleukin-Receptor Antagonist
anakinra
Monoclonal Antibodies
adalimumab
alemtuzumab
basiliximab
bevacizumab
certolizumab
Immunostimulants
1. Interferons
Interferons are proteins produced naturally by cells in response to viral infections and other stimuli. They work by interfering with virus replication within host cells, activating immune cells like natural killer cells and macrophages, and increasing the antigen presentation to lymphocytes.
Drug | Indications | Therapeutic Action | Adverse Effects |
Interferon alfa-2b | Chronic hepatitis C, Kaposi’s sarcoma, malignant melanoma | Inhibits viral replication, enhances immune response, and increases macrophage activity | Flu-like symptoms, myelosuppression, depression, suicidal ideation |
Interferon alfacon-1 | Hepatitis C | Inhibits viral replication and boosts immune system | Headache, dizziness, bone marrow suppression, photosensitivity |
Interferon alfa-n3 | Genital warts, basal cell carcinoma | Inhibits viral replication and tumor growth | Fatigue, anorexia, nausea, vomiting |
Interferon beta-1a | Multiple sclerosis | Reduces the frequency of clinical exacerbations and slows the progression of disability in multiple sclerosis | Injection site reactions, flu-like symptoms, liver dysfunction |
Interferon beta-1b | Multiple sclerosis | Similar to Interferon beta-1a; modulates the immune system to reduce inflammation | Fatigue, depression, flu-like symptoms, liver impairment |
Interferon gamma-1b | Chronic granulomatous disease, severe osteopetrosis | Enhances the respiratory burst of macrophages, stimulating greater antimicrobial activity | Fever, rash, diarrhea, myalgia |
Peginterferon alfa-2a | Chronic hepatitis C and B | Increases immune response against hepatitis viruses | Neutropenia, thrombocytopenia, liver enzyme abnormalities, flu-like symptoms |
Peginterferon alfa-2b | Chronic hepatitis C | Longer-lasting effects due to its pegylated form, allowing less frequent dosing | Similar to Peginterferon alfa-2a, including hematologic toxicity and depression |
Therapeutic Action:
- Interferons prevent viral particles from replicating inside host cells.
- They stimulate cells to produce antiviral proteins and enhance the cytotoxicity of T-cells and natural killer cells.
- They inhibit tumor growth by enhancing the host’s immune response.
Pharmacokinetics:
- Interferons are well absorbed via subcutaneous or intramuscular injection, reaching peak plasma levels within 3-8 hours.
- They are metabolized in the liver and kidneys and excreted primarily through the kidneys.
Contraindications:
- Allergies to interferons or their components.
- Pregnancy and lactation (due to teratogenic effects).
- Cardiac diseases, particularly arrhythmias and hypertension.
- Myelosuppression.
2. Interleukins
Interleukins are cytokines that play an essential role in the immune response by promoting the proliferation of lymphocytes and other immune cells.
- Cytokines: The general term for any small protein that helps cells communicate with each other.
Imagine your immune system as a big army. Interleukins are like the signals that tell different parts of the army what to do.
- Activate immune cells: Tell certain cells to start fighting off invaders.
- Control inflammation: Help regulate how much inflammation happens in response to an infection or injury.
- Promote cell growth: Help immune cells multiply and become stronger.
Drug | Indications | Therapeutic Action | Adverse Effects |
Aldesleukin | Metastatic renal cell carcinoma, metastatic melanoma | Stimulates the proliferation of T-cells and natural killer cells, enhances the immune response against cancer | Capillary leak syndrome, hypotension, anemia |
Oprelvekin | Prevention of severe thrombocytopenia in chemotherapy | Increases platelet production by stimulating megakaryocyte production | Fluid retention, edema, dyspnea, arrhythmias |
Therapeutic Action:
- Interleukins boost immune cell activity, enhancing the body’s ability to fight tumors and increase platelet production.
Pharmacokinetics:
- Interleukins are absorbed via subcutaneous injection, with peak levels occurring within hours.
- They are metabolized in the kidneys and excreted in urine.
Contraindications:
- Allergies to interleukins or E. coli-produced products.
- Pregnancy and lactation due to potential teratogenic effects.
- Patients with renal, liver, or cardiovascular impairments.

Immunosuppressants
Immunosuppressants are used primarily to prevent transplant rejection and treat autoimmune diseases by inhibiting the immune system.
These are like the “peacekeepers” of the immune system. They dampen down the immune response, preventing it from overreacting.
Used to treat autoimmune diseases where the immune system attacks the body’s own tissues. Cyclosporine is the most commonly used immunosuppressant.
1. T- and B-Cell Suppressors
T- and B-cell suppressors inhibit the activity of these lymphocytes, reducing the immune system’s ability to mount an attack against transplanted organs or self-tissues in autoimmune diseases.
Drug | Indications | Therapeutic Action | Adverse Effects |
Abatacept | Rheumatoid arthritis, juvenile idiopathic arthritis | Inhibits T-cell activation by binding to CD80 and CD86 on antigen-presenting cells | Headache, infections, hypertension, nausea |
Alefacept | Plaque psoriasis | Inhibits T-cell activation and reduces T-cell numbers | Lymphopenia, hepatotoxicity, infections |
Azathioprine | Prevention of kidney transplant rejection, rheumatoid arthritis | Inhibits purine synthesis, reducing T and B-cell proliferation | Bone marrow suppression, hepatotoxicity, nausea |
Therapeutic Action:
- These drugs inhibit the proliferation and activity of T-cells and B-cells, essential for preventing transplant rejection and treating autoimmune conditions.
Pharmacokinetics:
- T- and B-cell suppressors are generally well absorbed when administered orally or intravenously.
- They are metabolized in the liver and excreted primarily via the kidneys.
Contraindications:
- Allergies to the drugs or their components.
- Pregnancy and lactation (due to potential teratogenic effects).
- Renal or hepatic impairment.
- Active infections or known neoplasms.
2. Interleukin-Receptor Antagonist
This class of drugs blocks interleukin activity, which is critical in the inflammatory and immune response.
Drug | Indications | Therapeutic Action | Adverse Effects |
Anakinra | Rheumatoid arthritis | Blocks the interleukin-1 receptor, reducing inflammation and halting joint damage | Headache, sinusitis, nausea, infections, injection-site reactions |
Therapeutic Action:
- Interleukin-receptor antagonists prevent the binding of interleukins to their receptors, reducing inflammation and tissue damage.
Pharmacokinetics:
- Anakinra is administered subcutaneously and reaches peak plasma levels within hours.
- It is metabolized by the liver and excreted primarily in urine.
Contraindications:
- Allergies to E. coli–produced products or anakinra itself.
- Pregnancy and lactation due to the potential transfer of the drug to the fetus or infant.
- Renal impairment, immunosuppression, or active infections.
3. Monoclonal Antibodies
Monoclonal antibodies are laboratory-produced molecules that can mimic the immune system’s ability to fight off harmful pathogens such as viruses.
These are like highly specific “guided missiles” of the immune system.
They’re designed to target and attack specific cells or molecules. They can be used to treat cancer, autoimmune diseases, and even infections. Think of them as a sniper team that only targets the enemy, leaving the rest of the army alone.
Drug | Indications | Therapeutic Action | Adverse Effects |
Adalimumab | Rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis | Binds to tumor necrosis factor (TNF) alpha, inhibiting its inflammatory effects | Infections, malignancies, injection site reactions |
Alemtuzumab | Chronic lymphocytic leukemia | Targets CD52 on lymphocytes, leading to cell lysis | Infusion reactions, infections, cytopenias |
Basiliximab | Prevention of kidney transplant rejection | Blocks interleukin-2 receptor on T-cells, preventing their activation | GI disturbances, infections, hypersensitivity |
Monoclonal antibodies include adalimumab (Humira), alemtuzumab (Campath), basiliximab (Simulect), bevacizumab (Avastin), cetuximab (Erbitux), certolizumab (Cimzia), daclizumab (Zenapax)
Indications
- Prevention of renal transplant rejection
- Treatment of B-cell chronic lymphocytic leukemia
- Reduction of the signs and symptoms of Crohn disease
- Treatment of paroxysmal nocturnal hemoglobinuria, to reduce haemolysis.
- Treatment of B-cell non-Hodgkin lymphoma in conjunction with rituximab.
- Treatment of asthma with a very strong allergic component and seasonal allergic rhinitis not occasionally controlled by common medicine.
- Prevention of serious RSV(Respiratory syncytial virus) infection in high-risk children.
- Treatment of metastatic breast cancer.
- Treatment of psoriasis
Therapeutic Action:
- Monoclonal antibodies specifically target and neutralize pathogens or inflammatory molecules, providing targeted immune suppression.
Pharmacokinetics:
- These drugs are administered via intravenous injection and have variable half-lives depending on the specific antibody.
- They are metabolized and excreted through the reticuloendothelial system.
Contraindications
- Monoclonal antibodies are contraindicated in the presence of any known allergy to the drug or to murine products and in the presence of fluid overload.
- They should be used cautiously with fever (treat the fever before beginning therapy)
- They should not be used during pregnancy or lactation unless the benefit clearly outweighs the potential risk to the fetus or neonate.
Adverse Effects
- The most serious adverse effects associated with the use of
monoclonal antibodies are acute pulmonary edema (dyspnea, chest pain, wheezing), which is associated with severe fluid retention. - Fever
- Chills
- Malaise
- Myalgia
- Nausea
- Diarrhea
- Vomiting
- Increased susceptibility to infection
- Intravascular hemolysis with resultant fatigue, pain, dark urine, shortness of breath, and blood clots.


Fantastic website
Very interesting short and precise for starters mazima.
Thanks for everything
its so amazing,and understandable