Table of Contents
ToggleINTEGRATED MANAGEMENT OF CHILDHOOD ILLNESSES (IMCI)
Integrated Management of Childhood Illnesses is a child management process where care/treatment of a sick child is done in totality.
IMCI stands for Integrated Management of Childhood Illness is an approach developed by the United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO) to improve the health and well-being of children under the age of five.
IMCI is an integrated approach to child health that focuses on the well-being of the whole child.
IMCI aims to reduce death, illness, disability, and to promote improved growth and development among children under five years of age.
IMCI aims to reduce preventable mortality, minimize illness and disability, and promote healthy growth and development in young children.
IMCI guidelines help to interview caretakers accurately and recognize clinical signs, choose appropriate treatments, provide counseling and preventive care of children aged unto 5 years.
Goals of IMCI
- Identify key causes of childhood mortality.
- Explain the meaning and purpose of integrated case management.
- Describe the major steps in the IMCI strategy.
- Introduce use of IMCI tools including chart booklet, wall posters and case management sheets.
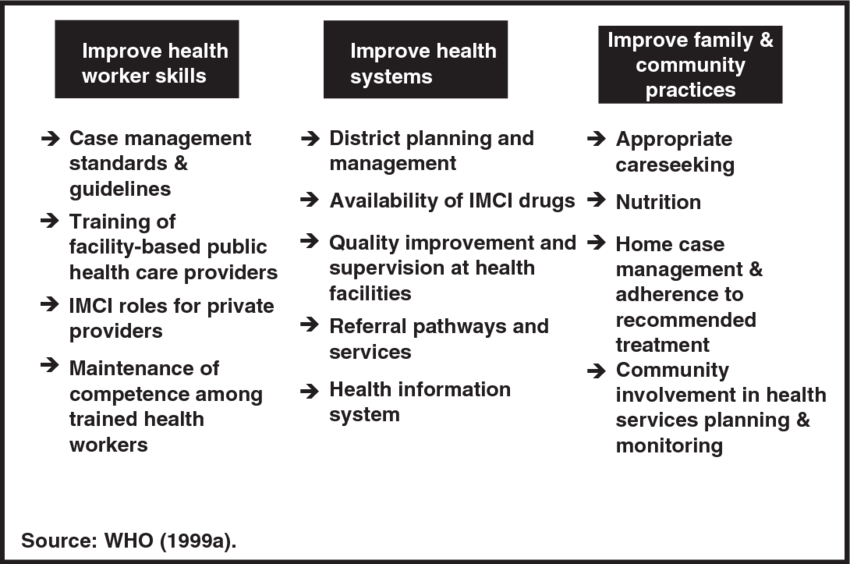
Key Components of IMCI
IMCI aims at three (3) main components of health care.
- Improving case management skills of healthcare providers.
- Improving health systems to provide quality care.
- Improving family and community health practices for health, growth, and development.
CHILD HEALTH AND MORTALITY
In 2015, approximately 5.9 million children under the age of five died worldwide, which translates to nearly 16,000 deaths every day. The leading causes of death in this age group are infections, neonatal conditions, and nutritional issues. Alarmingly, the majority of these deaths are preventable.
Uganda has been reported to have a high child mortality rate. According to the World Health Organization (WHO), Uganda ranks 168th out of 188 countries in terms of infant mortality rates.
The under-five mortality rate in Uganda was reported at 53 deaths per 1,000 live births in 2016, according to the World Bank.

Seventy five percent (75%) of the common causes of child mortality in developing countries include:
- Infectious Diseases: Acute respiratory infections, diarrhea diseases, malaria, and measles are leading causes of death among children under five years old. These diseases can be severe and life-threatening, especially in resource-constrained settings where access to healthcare and preventive measures may be limited.
- Malnutrition: Malnutrition is a significant contributor to child mortality in developing countries. Children who are malnourished have weakened immune systems, making them more susceptible to infectious diseases and less able to recover from illness.
It is important to note that these causes often overlap, and children may suffer from a combination of these conditions. The clinical presentations of these diseases can be similar, which may lead to challenges in diagnosing and treating children effectively.
WHY IMNCI? (Need for IMCI)
Multiple Conditions:
- Children often present with multiple potentially deadly conditions at the same time. IMCI takes a holistic approach, considering all the conditions that may affect a child and put them at risk of preventable mortality or impaired growth and development. By facilitating an integrated assessment and combined treatment of these conditions, IMCI focuses on effective case management and prevention of diseases, contributing to healthy growth and development.
Lack of Diagnostic Tools:
- In many healthcare settings, there is a lack of diagnostic tools such as laboratory tests or radiology. IMCI recognizes this challenge and provides clinical algorithms that rely on patient history, signs, and symptoms for diagnosis. By training healthcare providers in IMCI, they can effectively assess and manage childhood illnesses even in resource-limited settings.
Reliance on Patient History:
- IMCI acknowledges the importance of patient history in diagnosing and managing childhood illnesses. Healthcare providers are trained to gather comprehensive information about the child’s symptoms, medical history, and other relevant factors. This information, combined with the IMCI clinical algorithms, helps providers make accurate diagnoses and provide appropriate treatment.
Need for Referrals:
- In cases where a child has a serious illness that requires specialized care, IMCI emphasizes the need for timely referrals to a higher level of care . By identifying severe illnesses and facilitating prompt referrals, IMCI ensures that children receive the necessary treatment and support from specialized healthcare providers.
IMCI PROCESS
The IMCI (Integrated Management of Childhood Illness) process is a comprehensive approach to the identification and management of childhood illnesses in outpatient settings.
It aims to improve the quality of care for children under the age of five by providing standardized guidelines and interventions.
Here is an overview of the IMCI process and the interventions included in the IMCI guidelines:
IMCI Process:
- List of Conditions: The IMCI process involves checking for a list of conditions in children and infants to ensure comprehensive assessment and treatment.
- Assessment and Treatment: Children are assessed and treated for all conditions that are present, following standardized algorithms that guide management decisions.
- Decision to Transfer: If necessary, the IMCI guidelines provide guidance on when to transfer a child to higher levels of care for further management.
Interventions Included in the IMCI Guidelines:
The IMCI guidelines include both curative and preventive interventions for various childhood conditions.
Curative Interventions:
- Acute Respiratory Infections (ARI) including pneumonia
- Anaemia
- Diarrhoea (dehydration, persistent, dysentery)
- Ear infections
- HIV/AIDS
- Local bacterial infections
- Meningitis and sepsis
- Malnutrition
- Wheeze
- Malaria
- Measles
- Neonatal jaundice
Preventive Interventions:
- Breastfeeding support
- Immunization
- Nutrition counseling
- Periodic deworming
- Vitamin A supplementation
- Zinc supplementation
Who Can Use IMCI:
The IMCI process can be used by all doctors, nurses, and other health professionals who provide care for young infants and children under the age of five. It is primarily designed for first-level facilities such as clinics, health centers, or outpatient departments of hospitals.
The Case Management Process
IMCI classifies children into two categories:
- Sick young infants who range from 1 week to 2 months. Less than 1 week infants are not managed under IMCI, mainly because their illnesses are usually related to antenatal, labour and delivery.
- Sick child who range from 2 months to 5 years.
IMCI is designed for health workers (doctors, nurses etc) who treat sick children and infants in a first level health facility e.g. clinic, health center or OPD in a hospital.
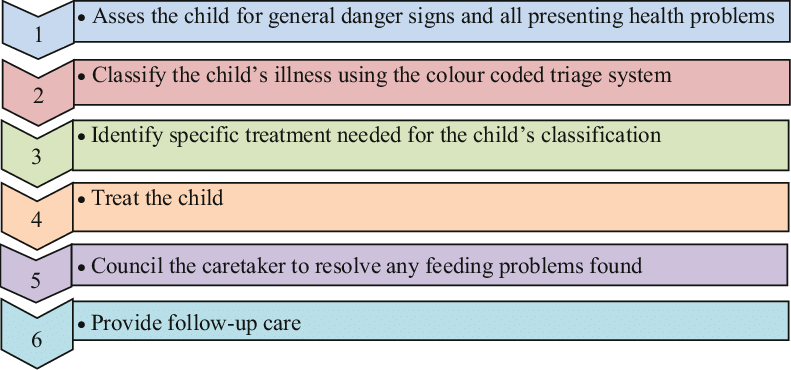
In the management process the following steps are taken:
- Assessing the child/young infant.
- Classify the illness.
- Identify treatment.
- Treating the child/ young infant.
- Give counseling to the mother.
- Give follow up care.
- Assessing the child means taking the history and performing a physical examination.
- Classifying the illness implies making a decision on the severity of illness i.e. you select a category of classification which corresponds with the severity of the disease.
Note that, classifications are not specific diagnoses but can be used to determine treatment e.g. severe febrile disease is a classification for a child who could be having cerebral malaria, meningitis, septicemia etc, but treatment for this classification covers for all the possible causes of the problem.
Steps in Integrated Case Management according to IMCI guidelines:
STEP 1: ASSESS
The assess column in the chart booklet describes how to take history and do a physical exam.
- Establish good communication with the mother of the child.
- Screen for general danger signs, which would indicate any life-threatening condition.
- Specific questions about the most common conditions affecting a child’s health (diarrhea, pneumonia, fever, etc).
- If the answers are positive, focus on a physical exam to identify life-threatening illness.
- Evaluation of the child’s nutrition and immunization status.
- The assessment includes checking the child for other health problems.
STEP 2: CLASSIFY
The classify (signs and classify) column of the chart lists clinical signs of illnesses and their classification. “Classify” in the chart means the health worker has to make a decision on the severity of the illness.
- Classify the child’s illnesses based on the assessment using a specially developed color-coded triage system.
- Because many children have more than one condition, each condition is classified according to whether it requires:
|
COLOUR |
CLASSIFICATION |
|
PINK |
Severe classification needing admission or pre-referral treatment and referral. |
|
YELLOW |
Classification needing specific medical treatment and advice. |
|
GREEN |
Not serious, and in most cases, no drugs are needed. Simple advice on home management given. |
STEP 3: IDENTIFY TREATMENT
The identify treatment column helps the healthcare workers to quickly and accurately identify treatments for the classifications selected. If a child or young infant has more than one classification, the healthcare worker must look at more than one table to find the appropriate treatments.
|
COLOUR |
CLASSIFICATION |
|
PINK |
If a child requires urgent referral, determine essential treatment to be given before referral. |
|
YELLOW |
If a child needs specific treatment, develop a treatment plan and identify the drugs to be administered at the clinic. Also, decide on the content of the advice to be given to the mother. |
|
GREEN |
If no serious conditions have been found, provide appropriate advice to the mother on the actions to be taken for the child’s care at home. |
STEP 4: TREAT
The treat column shows how to administer the treatment identified for the classifications. Treat means giving the treatment in the facility, prescribing drugs or other treatments to be given at home and also teaching the mother/caregiver how to administer treatment at home.
The following rules should be adhered to.
|
COLOUR |
CLASSIFICATION |
|
PINK |
If a child or young infant requires admission or referral, it is important the essential treatment is offered to the child or young infant before admission or referral. |
|
YELLOW |
If the child or young infant requires specific treatment, develop a treatment plan, administer drugs to be given at the facility and advise on treatment at home and counsel the mother/caregiver accordingly. |
|
GREEN |
If no serious conditions have been found (green classification), advise the mother/caregiver on care of the child at home. |
STEP 5: COUNSEL
- If follow up care is indicated, teach the mother/caregiver when to return to the clinic. Also teach the mother/ caregiver how to recognize signs indicating that the child or young infant should be brought back to the facility immediately.
- Assess feeding, including breastfeeding practice, and provide counseling to solve any feeding problems found. This also includes counseling the mother about her own health.
STEP 6: FOLLOW-UP
Some children or young infants need to be seen more than once for a current episode of illness. Identify such children or young infants and when they are brought back, offer appropriate follow up care as indicated in the IMNCI guidelines and also reassess the child or young infant for any new problems.
The guidelines also aim to empower healthcare workers to:
- Identify children who require additional follow-up visits.
- Provide appropriate follow-up care as indicated in IMCI guidelines.
- Correctly counsel the mother about her own health.
- Provide counseling for appropriate preventative and treatment measures.
- If necessary, reassess the child for any new problems.


This is good
It is very good.
Wonderful 👍