Table of Contents
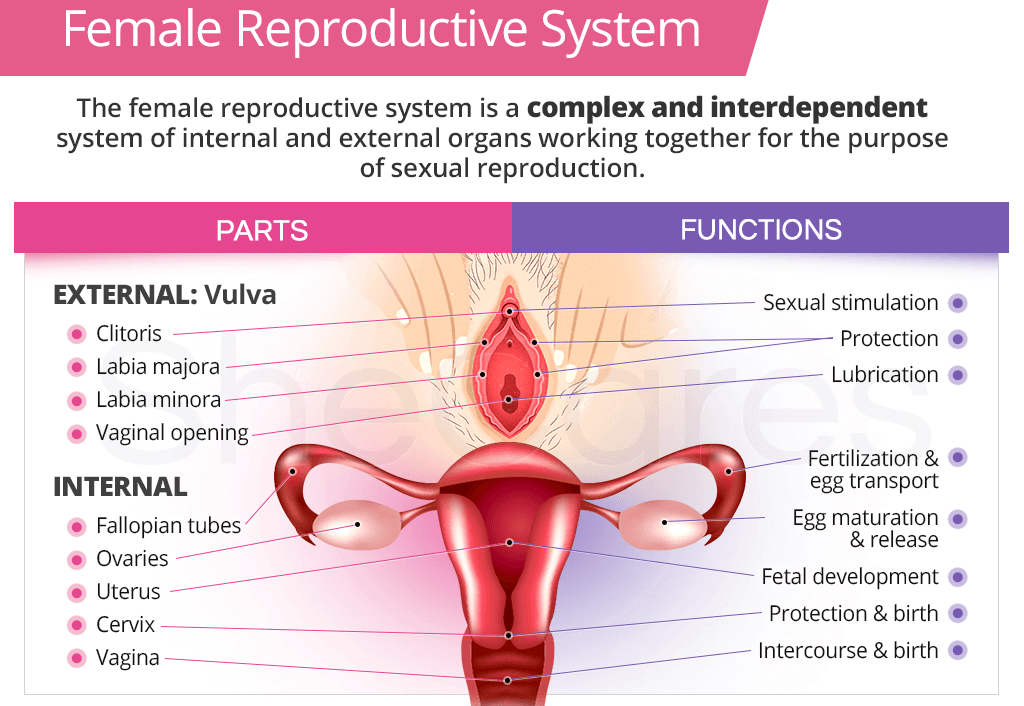
ToggleFemale Reproductive System
The functions of the female reproductive system are:
- Formation of ova
- Reception of spermatozoa
- Provision of suitable environments for fertilisation and fetal development
- Parturition (childbirth)
- Lactation, the production of breast milk, which provides complete nourishment for the baby in its early life.
The female reproductive organs, or genitalia, include both external and internal organs
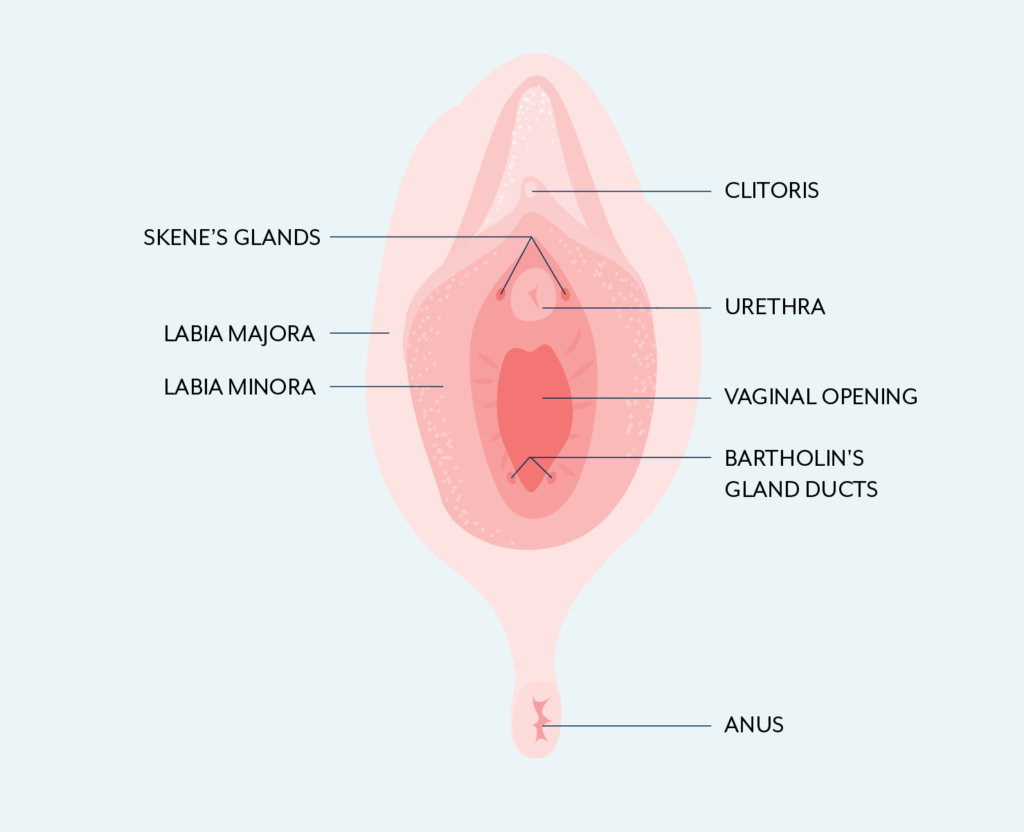
External Genitalia (Vulva)
The external genitalia are known collectively as the vulva, and consist of the labia majora and labia minora, the clitoris, the vaginal orifice, the vestibule, the hymen and the vestibular glands (Bartholin’s glands).

Labia majora
- These are the two large folds forming the boundary of the vulva.
- They are composed of skin, fibrous tissue and fat and contain large numbers of sebaceous and eccrine sweat glands.
- Anteriorly the folds join in front of the symphysis pubis, and posteriorly they merge with the skin of the perineum.
- At puberty, hair grows on the mons pubis and on the lateral surfaces of the labia majora.
Labia minora
- These are two smaller folds of skin between the labia majora, containing numerous sebaceous and eccrine sweat glands.
- The cleft between the labia minora is the vestibule.
- The vagina, urethra and ducts of the greater vestibular glands open into the vestibule.
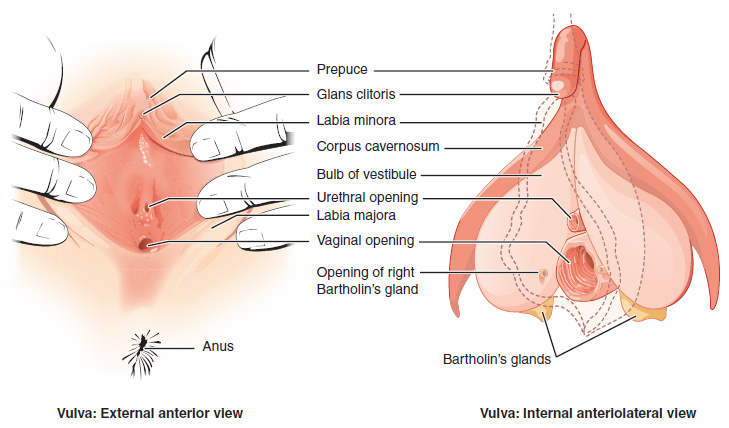
Clitoris
- The clitoris corresponds to the penis in the male and contains sensory nerve endings and erectile tissue.
- It is a small cylindrical mass composed of two small erectile bodies, the corpora cavernosa, and numerous nerves and blood vessels.
- The clitoris is located at the anterior junction of the labia minora.
- A layer of skin called the prepuce of the clitoris is formed at the point where the labia minora unite and covers the body of the clitoris.
- The exposed portion of the clitoris is the glans clitoris.
Vestibule
- The region between the labia minora is the vestibule.
- Within the vestibule are the hymen (if still present), the vaginal orifice, the external urethral orifice, and the openings of the ducts of several glands.
- Anterior to the vaginal orifice and posterior to the clitoris is the external urethral orifice, the opening of the urethra to the exterior.
- On either side of the external urethral orifice are the openings of the ducts of the paraurethral (Skene’s) glands. These mucus-secreting glands are embedded in the wall of the urethra.
- On either side of the vaginal orifice itself are the greater vestibular (Bartholin’s) glands, which open by ducts into a groove between the hymen and labia minora. They produce a small quantity of mucus during sexual arousal and intercourse that adds to cervical mucus and provides lubrication.
Hymen
- The hymen is a thin layer of mucous membrane that partially occludes the opening of the vagina.
- It is normally incomplete to allow for passage of menstrual flow.
- It is partially torn by coitus and completely torn by child birth.

Vestibular glands(Bartholin’s glands)
- The vestibular glands (Bartholin’s glands) are situated one on each side near the vaginal opening.
- They are about the size of a small pea and have ducts, opening into the vestibule immediately lateral to the attachment of the hymen.
- They secrete mucus that keeps the vulva moist.
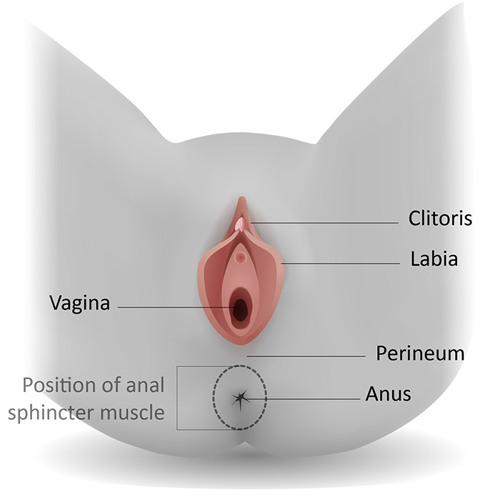
Perineum
- The perineum is a roughly triangular area extending from the base of the labia minora to the anal canal.
- It consists of connective tissue, muscle and fat. It gives attachment to the muscles of the pelvic floor.
Internal Genitalia
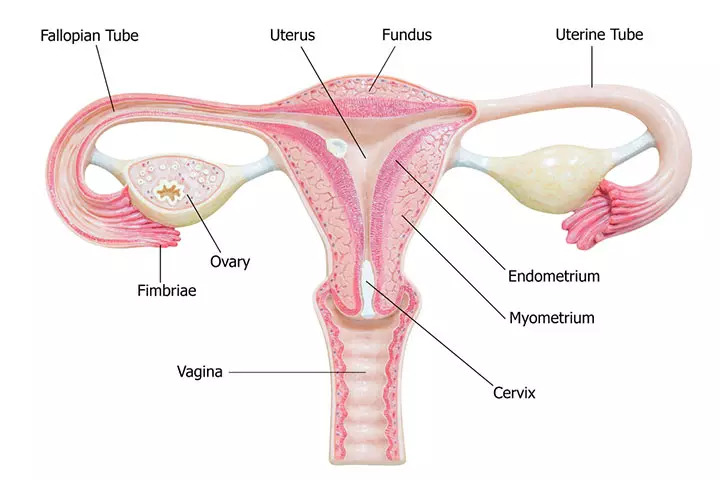
The internal organs of the female reproductive system lie in the pelvic cavity and consist of the vagina, uterus, two uterine tubes and two ovaries
Vagina
- The vagina is a fibromuscular tube lined with a non keratinized stratified squamous epithelium that extends from the exterior of the body to the uterine cervix, connecting the external and internal organs of reproduction.
- It runs obliquely upwards and backwards at an angle of about 45° between the bladder in front and rectum and anus behind.
- It is situated between the urinary bladder and the rectum.
- In the adult, the anterior wall is about 7.5 cm long and the posterior wall about 9 cm long. The difference is due to the angle of insertion of the cervix through the anterior wall.
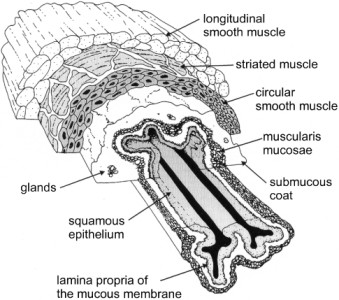
Structure
The vagina has three layers:
- An outer covering of areolar tissue
- A middle layer of smooth muscle
- An inner lining of stratified squamous epithelium that forms ridges or rugae.
It has no secretory glands but the surface is kept moist by cervical secretions.
- Between puberty and the menopause, Lactobacillus acidophilus bacteria are normally present, which secrete lactic acid, maintaining the pH between 4.9 and 3.5. The acidity inhibits the growth of most other microorganisms that may enter the vagina from the perineum.
Arterial supply: An arterial plexus is formed round the vagina, derived from the uterine and vaginal arteries, which are branches of the internal iliac arteries.
Venous drainage: A venous plexus, situated in the muscular wall, drains into the internal iliac veins.
Functions
- The vagina acts as the receptacle for the penis during sexual intercourse (coitus).
- Provides an elastic passageway through which the baby passes during childbirth.
- It acts as the outlet for menstrual flow.
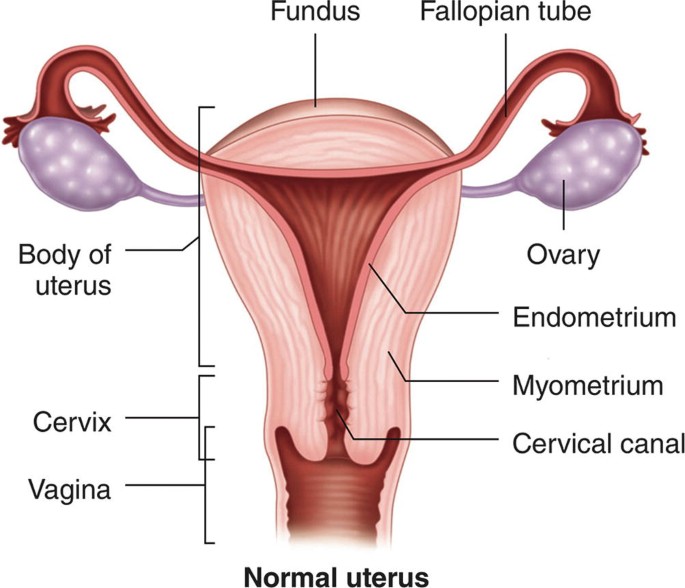
Uterus
The uterus, a hollow, pear-shaped organ with a flattened anteroposterior orientation, is situated in the pelvic cavity between the urinary bladder and the rectum.
Weighing between 30 to 40 grams, the uterus assumes an almost horizontal position, measuring approximately 7.5 cm in length, 5 cm in width, and possessing walls around 2.5 cm thick.
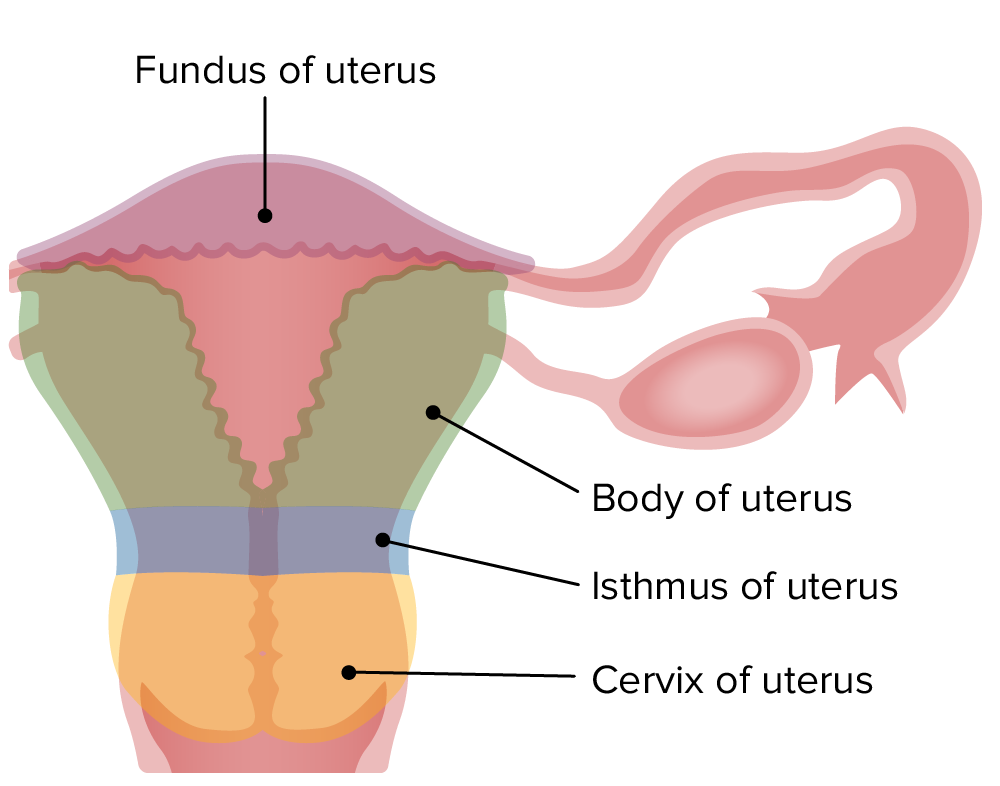
Uterine Parts
- Fundus: The dome-shaped upper part of the uterus above the openings of the uterine tubes.
- Body: The main and widest part, narrowing inferiorly at the internal as it connects with the cervix.
- Cervix: The neck of the uterus, protruding through the anterior wall of the vagina and opening into it at the external os.
- N.B: The isthmus, a constricted region about 1 cm long, lies between the body and the cervix.
Uterine Structure:
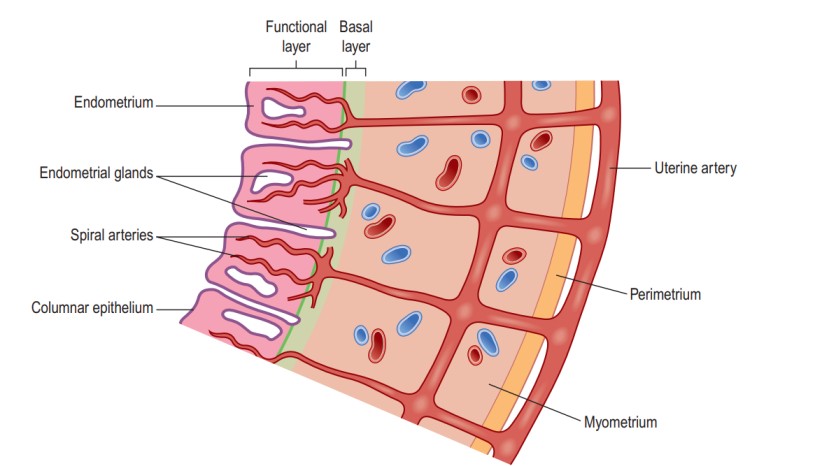
The uterus comprises three layers of tissue: perimetrium, myometrium, and endometrium.
- Perimetrium: Covers the fundus, body, and cervix, forming the vesicouterine pouch anteriorly and the rectouterine pouch (of Douglas) posteriorly. The broad ligament attaches the uterus to the sides of the pelvis at its lateral ends.
- Myometrium: The thickest layer, consisting of smooth muscle fibers interlaced with areolar tissue, blood vessels, and nerves.
- Endometrium: Composed of columnar epithelium with mucus-secreting tubular glands. Functionally divided into the upper functional layer, shed during menstruation if the ovum is not fertilized, and the basal layer, regenerating the functional layer during each cycle. The upper two-thirds of the cervical canal is lined with this mucous membrane.
Vascular Supply:
- Arterial supply is provided by uterine arteries, branches of the internal iliac arteries, passing up the lateral aspects of the uterus between the layers of the broad ligaments.
- Venous drainage follows a similar route, eventually draining into the internal iliac veins.
Functions of the Uterus:
- Menstrual Cycle: Prepares the uterus for receiving, nourishing, and protecting a fertilized ovum.
- Implantation Site: Serves as the site for the embedment of the fertilized ovum (zygote).
- Uterine Secretions: Nourish the ovum before and after implantation in the endometrium.
- Placental Attachment: Acts as a site of attachment for the placenta.
- Labour: During labour, the uterus expels the baby through powerful, rhythmic contractions.

Supporting Structures of the Uterus/The wall of the Uteus
The uterus is intricately supported within the pelvic cavity by surrounding organs, pelvic floor muscles, and an array of ligaments that suspend it from the pelvic walls. The key supporting structures include:
1. Broad Ligaments:
- Formed by a double fold of peritoneum on each side of the uterus.
- Extend down from the uterine tubes, appearing draped over them, with lateral ends attached to the sides of the pelvis.
- Uterine tubes are enclosed in the upper free border, penetrating the posterior wall of the broad ligament near lateral ends, opening into the peritoneal cavity.
- Ovaries are attached to the posterior wall, one on each side.
- Blood, lymph vessels, and nerves pass to the uterus and uterine tubes between the layers of the broad ligaments.
2. Round Ligaments:
- Bands of fibrous tissue situated between the two layers of the broad ligament on either side of the uterus.
- Extend to the sides of the pelvis and traverse the inguinal canal, concluding by merging with the labia majora.
3. Utero-sacral Ligaments:
- Originate from the posterior walls of the cervix and vagina.
- Extend backward, one on each side of the rectum, ultimately attaching to the sacrum.
4. Transverse Cervical (Cardinal) Ligaments:
- Extend from each side of the cervix and vagina to the side walls of the pelvis.
5. Pubo-cervical Fascia:
- Extends forward from the transverse cervical ligaments on each side of the bladder.
- Attaches to the posterior surface of the pubic bones.

Fallopian Tubes
- The uterine (Fallopian) tubes, measuring approximately 10 cm in length, extend laterally from the uterus, positioned between its body and fundus.
- Located in the upper free border of the broad ligament, the trumpet-shaped lateral ends of these tubes penetrate the posterior wall, opening into the peritoneal cavity in close proximity to the ovaries.
- Each tube terminates with fingerlike projections known as fimbriae, with the ovarian fimbria being the longest and closely associated with the ovary.
- These tubes lie within the folds of the broad ligaments of the uterus, providing a crucial pathway for sperm to reach an ovum and facilitating the transportation of secondary oocytes and fertilized ova from the ovaries to the uterus.

Fallopian Tube Parts:
- Fimbriae End: The extremity of each tube with fingerlike projections.
- Infundibulum: A funnel-shaped section close to the ovary, open to the pelvic cavity.
- Uterine Tube Extension: Extends medially and eventually inferiorly, attaching to the superior lateral angle of the uterus.
- Ampulla: The widest, longest portion, constituting approximately the lateral two-thirds of the tube’s length.
- Isthmus: A more medial, short, narrow, thick-walled portion connecting to the uterus.
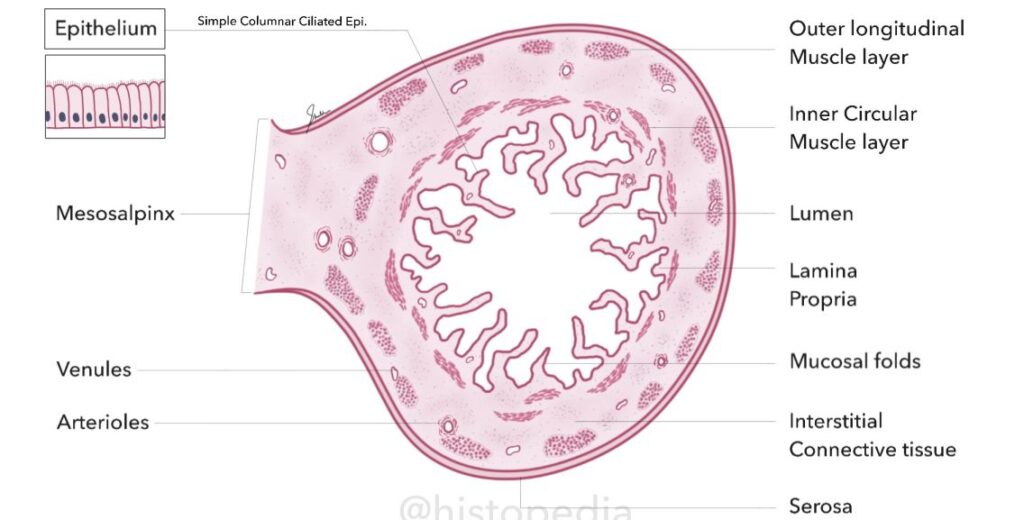
Fallopian Tube Structure:
- The uterine tubes exhibit an outer covering of peritoneum (broad ligament), a middle layer of smooth muscle (muscularis), and are lined with ciliated epithelium.
- The epithelium contains ciliated simple columnar cells, acting as a “ciliary conveyor belt” to facilitate the movement of a fertilized ovum (or secondary oocyte) within the uterine tube towards the uterus. Non-ciliated cells, peg cells, possess microvilli and secrete fluid providing nutrition for the ovum.
- The muscularis layer comprises an inner, thick, circular ring of smooth muscle and an outer, thin region of longitudinal smooth muscle. Peristaltic contractions and the ciliary action of the mucosa work collaboratively to propel the oocyte or fertilized ovum towards the uterus.
- The outer layer of the uterine tubes is a serous membrane, the serosa (peritoneum).
- Local currents generated by the movements of the fimbriae during ovulation sweep the ovulated secondary oocyte from the pelvic cavity into the uterine tube.
- Sperm encounter and fertilize a secondary oocyte in the ampulla of the uterine tube, although fertilization in the pelvic cavity is not uncommon.
Fallopian Tube Functions:
- Ovum Movement: Uterine tubes facilitate the movement of the ovum from the ovary to the uterus through peristalsis and ciliary movement.
- Mucus Secretion: The mucosa secretes mucus, creating ideal conditions for the movement of ova and spermatozoa.
- Fertilization Site: Fertilization of the ovum usually occurs in the uterine tube, with the zygote propelled into the uterus for implantation.
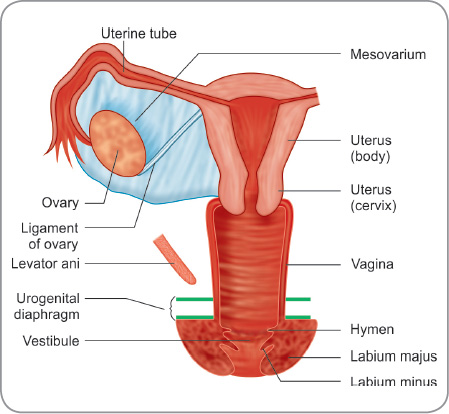
Ovaries
- The ovaries, functioning as the female gonads responsible for producing sex hormones and ova, are situated in a shallow fossa on the lateral walls of the pelvis.
- They measure between 2.5 to 3.5 cm in length, 2 cm in width, and 1 cm in thickness.
- Homologous to the testes, each ovary is attached to the upper part of the uterus by the ovarian ligament and to the back of the broad ligament by a broad band of tissue known as the mesovarium. Blood vessels and nerves access the ovary through the mesovarium.
Ovary Ligaments and Attachment:
- The broad ligament of the uterus, a part of the parietal peritoneum, connects to the ovaries through a double-layered peritoneal fold named the mesovarium.
- The ovarian ligament anchors the ovaries to the uterus, while the suspensory ligament attaches them to the pelvic wall.
- Each ovary contains a hilum, the point of entrance and exit for blood vessels and nerves, along which the mesovarium is attached.
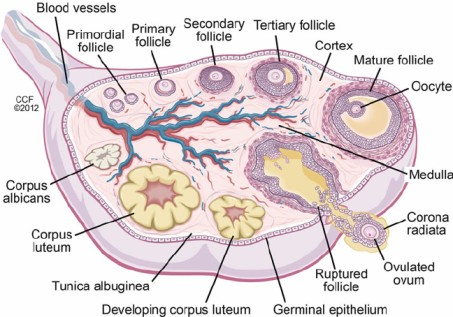
Ovary Structure:
The ovaries consist of two main parts:
Medulla:
- Located at the centre and comprises fibrous tissue, blood vessels, and nerves.
Cortex:
- Surrounds the medulla.
- Features a framework of connective tissue or stroma, covered by germinal epithelium.
- Contains ovarian follicles in various stages of maturity, each housing an ovum.
- Before puberty, the ovaries are inactive, but the stroma already contains immature (primordial) follicles, present from birth.
- Approximately every 28 days during the childbearing years, one ovarian follicle (Graafian follicle) matures, ruptures, and releases its ovum into the peritoneal cavity, a process known as ovulation.
- Following ovulation, the ruptured follicle transforms into the corpus luteum (meaning ‘yellow body’), leaving a small permanent scar of fibrous tissue called the corpus albicans (meaning ‘white body’) on the ovary’s surface.
Ovary Vascular Supply:
- Arterial supply is provided by the ovarian arteries branching from the abdominal aorta just below the renal arteries.
- Venous drainage occurs through a plexus of veins behind the uterus, giving rise to the ovarian veins. The right ovarian vein opens into the inferior vena cava, while the left opens into the left renal vein.
Ovary Hormone Production:
The ovaries play a pivotal role in hormone production, synthesizing oestrogen and progesterone.
Mammary Glands/Breasts.
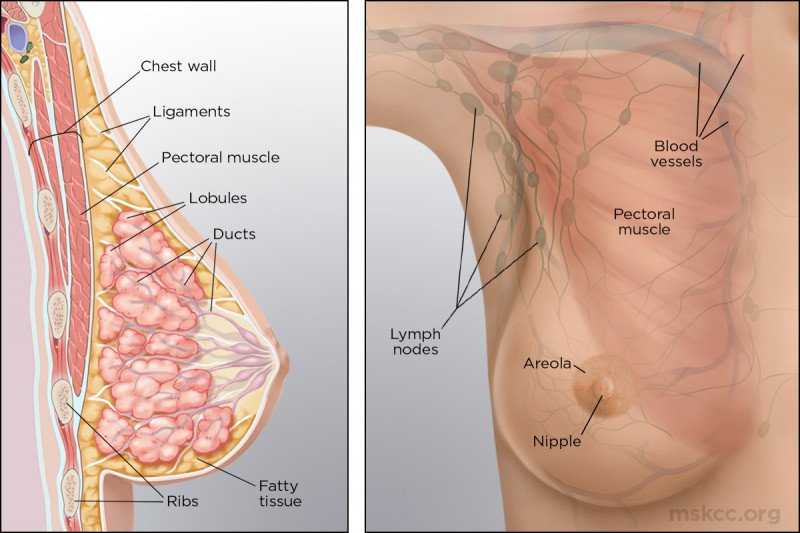
- The breasts, or mammary glands, serve as accessory glands in the female reproductive system and exist in a rudimentary form in males.
- Each breast is a variable-sized hemispheric projection located anterior to the pectoralis major and serratus anterior muscles, attached to them by a layer of fascia composed of dense irregular connective tissue.
Breast Anatomy:
- Nipple: Each breast features a pigmented projection known as the nipple, which contains closely spaced openings of ducts called lactiferous ducts, through which milk emerges.
- Areola: The circular pigmented area of skin surrounding the nipple is called the areola, appearing rough due to the presence of modified sebaceous (oil) glands.
- Suspensory Ligaments: Strands of connective tissue, known as the suspensory ligaments of the breast (Cooper’s ligaments), run between the skin and fascia, providing support to the breast. These ligaments may loosen with age or due to excessive strain, as seen in long-term jogging or high-impact aerobics. Wearing a supportive bra can slow this process and help maintain the strength of the suspensory ligaments.
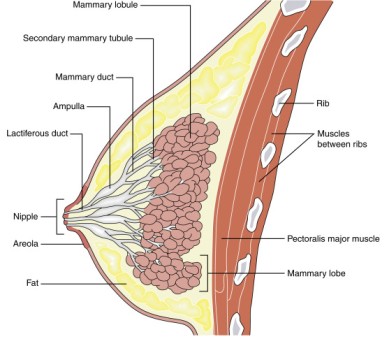
Mammary Gland Structure:
- Within each breast lies a mammary gland responsible for milk production.
- A mammary gland comprises 15 to 20 lobes, or compartments, separated by variable amounts of adipose tissue.
- Each lobe contains smaller compartments called lobules, consisting of grapelike clusters of milk-secreting glands known as alveoli, embedded in connective tissue.
- Contraction of myoepithelial cells surrounding the alveoli facilitates the propulsion of milk toward the nipples.
- During milk production, it moves from the alveoli into secondary tubules and then into mammary ducts.
- Near the nipple, mammary ducts expand to form sinuses called lactiferous sinuses, where some milk may be stored before draining into a lactiferous duct.
- Each lactiferous duct carries milk from one of the lobes to the exterior, allowing for breastfeeding and milk secretion.

Female Puberty
Puberty is the age at which the internal reproductive organs reach maturity, usually between the ages of 12 and 14.
This is called the menarche, and marks the beginning of the childbearing period.
The ovarian maturation is stimulated by gonadotropins from the anterior pituitary, namely follicle-stimulating hormone and luteinizing hormone.
Key Changes During Female Puberty:
- Reproductive Organs Maturity: The uterus, uterine tubes, and ovaries attain maturity, preparing for their crucial roles in the reproductive system.
- Menstrual Cycle and Ovulation Onset (Menarche): Menarche means the commencement of the menstrual cycle and ovulation.
- Breast Development and Enlargement: Significant changes occur in the breasts, characterized by development and enlargement.
- Growth of Pubic and Axillary Hair: Pubic and axillary hair growth signifies the onset of secondary sexual characteristics.
- Height Increase and Pelvic Widening: Puberty is accompanied by a noticeable increase in height and the widening of the pelvis, facilitating the accommodation of potential reproductive processes.
- Distribution of Subcutaneous Fat: There is an increase in subcutaneous fat deposition, particularly at the hips and breasts.
The Reproductive Cycle in Females
This is a series of events, occurring regularly in females every 26 to 30 days throughout the childbearing period between menarche and menopause.
The cycle consists of a series of changes taking place concurrently in the ovaries and uterine lining, stimulated by changes in blood concentrations of hormones
Hormonal Regulation:
The hypothalamus secretes luteinizing hormone-releasing hormone (LHRH), stimulating the anterior pituitary to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
FSH promotes the maturation of ovarian follicles and the secretion of oestrogen, while LH triggers ovulation and supports the development of the corpus luteum.

Menstrual Phase:
- In the absence of fertilization, the corpus luteum degenerates, causing a decline in oestrogen and progesterone levels.
- The functional layer of the endometrium, dependent on these hormones, is shed during menstruation.
- Menstrual flow consists of endometrial secretions, cells, blood, and the unfertilized ovum.
Proliferative Phase:
- FSH stimulates the growth of an ovarian follicle, leading to the production of oestrogen.
- Oestrogen triggers the proliferation of the endometrial functional layer in preparation for potential fertilization.
- Rising oestrogen levels prompt an LH surge, culminating in ovulation and marking the end of the proliferative phase.
Secretory Phase:
- After ovulation, LH stimulates the development of the corpus luteum, which produces progesterone, estrogen, and inhibin.
- Progesterone induces endometrial changes, enhancing the secretory glands and facilitating spermatozoa movement.
- Cervical mucus increases, aiding sperm passage, and observable changes indicate ovulation.
Fertilization and Pregnancy:
The ovum has a short fertilizable window(probably as little as 8 hours), while sperm can survive longer.
If fertilization occurs, the zygote travels to the uterus, where it embeds, produces hCG, and sustains the corpus luteum.
Hormones from the corpus luteum, placenta, and gonadotrophins support the early stages of pregnancy, inhibiting further follicle maturation.