Table of Contents
ToggleTopic 3.10 / 3.11: Natural Body Defence Mechanism
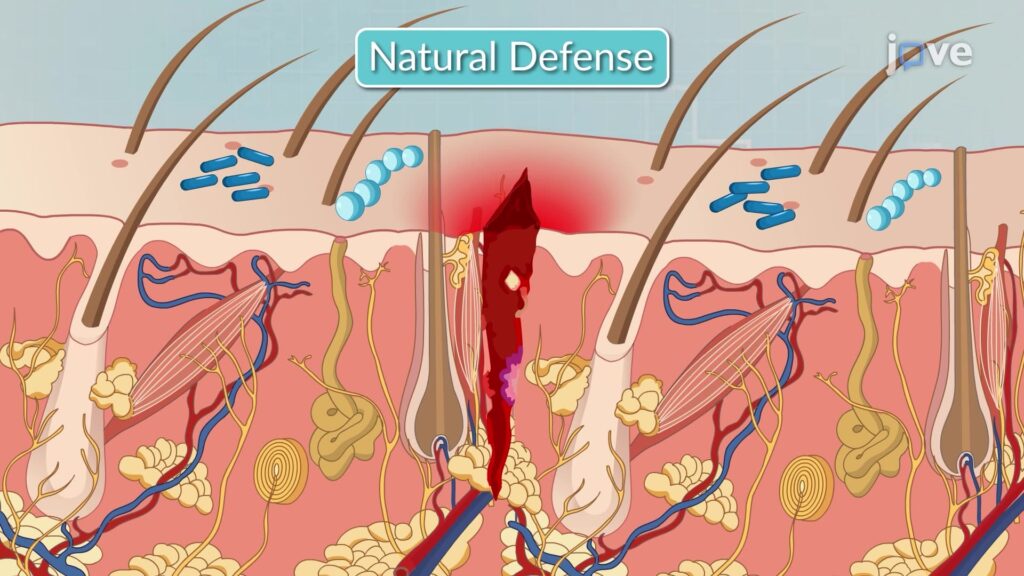
The human body possesses a sophisticated array of natural defense mechanisms designed to protect against pathogens (e.g., bacteria, viruses, fungi) and foreign substances, as well as to repair damaged tissues. These defenses can be broadly categorized into non-specific (innate) defenses and specific (adaptive) defenses.
I. Non-Specific (Innate) Defenses:
These are the body's first line of defense, providing immediate, general protection against a wide range of threats without prior exposure. They do not differentiate between types of pathogens.
- Skin: Intact skin acts as a formidable physical barrier, preventing pathogen entry. It also produces antimicrobial peptides and has a slightly acidic pH (acid mantle) which inhibits bacterial growth.
- Mucous Membranes: Line all body cavities open to the exterior (respiratory, gastrointestinal, genitourinary tracts). They trap pathogens with sticky mucus and often contain antimicrobial substances.
- Cilia: Hair-like projections in the respiratory tract that sweep mucus and trapped pathogens upwards for expulsion (e.g., coughing, sneezing).
- Normal Flora (Microbiota): Non-pathogenic microorganisms colonizing various body surfaces (skin, gut, vagina) that compete with pathogens for nutrients and space, often producing inhibitory substances.
- Body Secretions:
- Tears & Saliva: Contain lysozyme, an enzyme that breaks down bacterial cell walls.
- Gastric Acid: Highly acidic environment in the stomach destroys most ingested pathogens.
- Urine: The acidic pH and flushing action help prevent bacterial colonization of the urinary tract.
- Vaginal Secretions: Acidic pH inhibits the growth of many pathogens.
- Cerumen (Earwax): Traps particles and contains antimicrobial properties.
If pathogens breach the first line, the second line of defense activates, involving cellular and chemical responses.
- Phagocytes: Specialized white blood cells that engulf and digest foreign particles and pathogens.
- Neutrophils: Abundant, early responders to infection, highly phagocytic.
- Macrophages: Develop from monocytes, larger and longer-lived, act as "clean-up crews" and antigen-presenting cells.
- Natural Killer (NK) Cells: Lymphocytes that non-specifically kill virus-infected cells and cancer cells by inducing apoptosis (programmed cell death).
- Inflammatory Response: A localized tissue response to injury or infection, characterized by redness (rubor), heat (calor), swelling (tumor), and pain (dolor). Its purpose is to:
- Prevent spread of damaging agents.
- Dispose of cell debris and pathogens.
- Set the stage for repair.
Key chemical mediators like histamine and prostaglandins cause vasodilation and increased capillary permeability.
- Antimicrobial Proteins:
- Interferons (IFNs): Proteins released by virus-infected cells that protect neighboring uninfected cells from viral replication.
- Complement System: A group of plasma proteins that, when activated, enhances inflammation, promotes phagocytosis (opsonization), and directly lyses (bursts) bacterial cells.
- Fever: Systemic response to infection, raising body temperature. Moderate fever can:
- Inhibit the growth of some microorganisms.
- Increase metabolic rate, speeding up repair processes.
- Enhance phagocytic activity.
II. Specific (Adaptive) Defenses:
This is the body's third line of defense, which is highly specific, systemic, and has memory. It targets specific pathogens and improves with each subsequent exposure.
- Specificity: Recognizes and targets specific antigens.
- Memory: Remembers previous encounters with pathogens, allowing for a faster and stronger response upon re-exposure.
- Systemic: Not restricted to the initial infection site.
- Lymphocytes:
- B Lymphocytes (B cells): Responsible for humoral immunity. They produce antibodies that circulate in bodily fluids and target extracellular pathogens (e.g., bacteria, toxins).
- T Lymphocytes (T cells): Responsible for cellular immunity. They directly attack infected cells, cancer cells, or foreign cells. Types include:
- Helper T cells (CD4+): Coordinate both humoral and cellular immunity.
- Cytotoxic T cells (CD8+): Directly kill target cells.
- Regulatory T cells: Suppress immune responses to prevent autoimmunity.
- Antigen-Presenting Cells (APCs): Cells (e.g., macrophages, dendritic cells) that present antigens to T cells, initiating an adaptive immune response.
- Antibodies (Immunoglobulins): Proteins produced by plasma cells (differentiated B cells) that bind specifically to antigens, marking them for destruction.
- Active Immunity: Develops when the body produces its own antibodies or activated T cells in response to an antigen.
- Naturally acquired active immunity: Infection (e.g., getting sick with measles).
- Artificially acquired active immunity: Vaccination (e.g., MMR vaccine).
- Passive Immunity: Occurs when antibodies are transferred from one individual to another. Provides immediate but temporary protection as the body does not produce its own memory cells.
- Naturally acquired passive immunity: Antibodies passed from mother to fetus via placenta or to infant via breast milk.
- Artificially acquired passive immunity: Injection of pre-formed antibodies (e.g., antivenom, rabies immunoglobulin).
Interrelationship of Defenses:
It's crucial to understand that these defense mechanisms do not operate in isolation. Innate defenses provide immediate protection and also activate and guide the more specific adaptive immune responses. For example, inflammation helps to bring immune cells to the site of infection, and macrophages (innate) can act as APCs, linking to adaptive immunity. A healthy immune system relies on the coordinated action of all these components.
INFLAMMATION
Inflammation is part of the body's immune response to irritation, injury, or infection. Inflammation is a defensive mechanism in the body. Inflammation is a defensive reaction intended to neutralize, control or eliminate the offending agent and to prepare the site for repair.
It can be beneficial when, for example, your knee sustains a blow and tissues need care and protection. However, sometimes, inflammation can persist longer than necessary, causing more harm than benefit.
Cells or tissues of the body may be injured or killed by any of the agent (physical, chemical, infections) when this happens, an inflammatory response (inflammation) naturally occurs in healthy tissues adjacent to the site of injury.
Note: inflammation is not the same as infection, an infectious agent is only one of several agents that may trigger an inflammatory response. An infection exist when the infectious agent is living, growing and multiplying in the tissues and is able to overcome the body’s normal defense.
Inflammation differs from antibody mediated immunity and cell mediated immunity (AMI and CMI) in two important ways:
- Inflammatory protection is immediate but short term. It does not provide true immunity on repeated exposure to the same organisms.
- Inflammation is a non-specific body defense to invasion or injury and can be started quickly by almost any event, regardless of where it occurs or what causes it.
Functions of inflammation
- When something harmful or irritating affects a part of our body, there is a biological response to try to remove it. The signs and symptoms of inflammation can be uncomfortable but are a show that the body is trying to heal itself.
- Cells of inflammation or tissues of the body may be injured or killed by any of the agents (physically chemical, infectious) when this happens an inflammatory response (inflammation) naturally occurs in the healthy tissues adjacent to the site of injury.
- It provides immediate protection against the effects of tissue injury and invading foreign proteins.
- Inflammation also helps start both antibodies mediated and cell mediated actions to activate full immunity.
- It can be a barrier to prevent organisms from entering the body or can be an attacking force that eliminates organisms that have already entered the body.
- This type of immunity cannot be transferred from one person to another and is not an adaptive response to exposure or invasion by foreign proteins.
- The inflammatory response are part of innate immunity and other parts of innate immunity include;- This is the body’s ability to resist invading organisms and It is achieved through natural barriers, biologically functionally and chemically using:
- The skin as a barrier,
- Mucus to trap organisms,
- mucus membranes as a barrier
- Biological agents like normal flora
- Functional like taking a lot of fluids to flash
- Chemical secretions like tears to clear away
- Cell mediated like lymphocytes or antibodies
CELL TYPES INVOLVED IN INFLAMMATION
The leukocytes (white blood cells) involved in inflammation are neutrophils, macrophages, eosinophil’s and basophils. An additional cell type important in inflammation is the tissue mast cell. Neutrophils and macrophages destroy and eliminate foreign invaders. Basophils, Eosinophil’s and mast cells release chemicals that act on blood vessels to cause tissue level responses that help neutrophil and microphage actions.
NEUTROPHILS
- Mature neutrophils make up between 55% and 70% of the normal total white blood cell count.
- Neutrophils come from the stem cells and complete the maturation process in the bone marrow.
- They are also called granulocytes because of the large number of granules present inside each cell; other names of neutrophils are based on their appearance and maturity.
- Mature neutrophils are also called segmented neutrophils because of their nuclear shape.
- Usually, growth of a stem cell into a mature neutrophil requires 12 to 14 days.
- In a healthy person with full immunity, more than 100 billion fresh, mature neutrophils are released from the bone marrow into the circulation daily.
- This huge production is needed because the life span of each neutrophil is short about 12 to 18 days.
- Neutrophil function provides protection after invaders especially bacteria enter the body. This powerful army of small cells destroys invaders by phagocytosis and enzymatic digestion, although each cell is small and can take part in only one episode of phagocytosis.
MACROPHAGE
- Macrophage come from the committed myeloid stem cells in the marrow: and form the mono nuclear phagocyte system.
- The stem cells first form monocytes which are released into the blood stream at this stage until they mature. Monocytes have limited activity.
- Most monocytes move from the blood into the body tissues where they mature into macrophage.
- Some macrophages become fixed in position within the tissues whereas others can move within and between tissues.
- The liver, spleen and intestinal tract within large numbers of these cells.
FUNCTIONS
- Macrophage protects the body in several ways;-
- These cells are important in immediate inflammatory responses and also stimulate the longer-lasting immune responses of antibody mediated immunity and cell mediated immunity.
- Macrophage functions include phagocytosis, repair antigen presenting and secretion of cytokines for the immune system control.
BASOPHILS
- Basophils come from myeloid stem cells and make up only about 1% of the total circulating white blood cell count.
- These cells cause the manifestation of inflammation.
Functions
- Basophils act on blood vessels and release chemicals which include;- heparin, histamine, serotonin, kinins and leukotriene’s.
- Basophils have sites that bind the portion of immune-globulin E (IgE) molecules which binds to and is activated by allergens.
- When allergens bind to the IgE on the basophils, the basophils membrane opens and releases the vaso-active amines into the blood, where most of them act on smooth muscle and blood vessel walls.
- Heparin inhibits blood and proteins clotting.
- Histamine constricts small veins inhibiting blood flow and decreasing venous return.
- This effect causes blood to collect in capillaries and arterioles.
- Kinins dilate arterioles and increase capillary permeability.
- These actions cause blood plasma to leak into the interstial space.
EOSINOPHILS
- These come from the myeloid line and contain many vaso-active chemical.
Functions
- Eosinophil’s are very active against infestations on rurastic larvae and also limits inflammatory reaction.
- The eosinophil granules contain many different substances; some are enzymes that degrade the vaso-active chemicals released by other leukocytes.
TISSUE MAST CELLS
- These cells have functions very similar to basophils and eosinophils. Although mast cells do originate in the bone marrow, they come from different parent cells than leukocytes and do not circulate as mature cells.
- Instead they differentiate and mature in tissues especially those near blood vessels, nerves, lung tissues skin and mucous membranes.
- Some mast cells also respond to the inflammatory products made and released by T. lymphocytes.
The tissue mast cells have important roles in maintaining and prolonging inflammatory and hypersensitivity reactions.
STAGES/ PHASES OF INFLAMMATION
Injury
- Any type of injury of exogenous (outside the body) or endogenous (inside the body) injury can initiate the inflammatory y response; heat cold, radiations, chemicals, trauma infections, immunological injuries, neoplasms etc.
- Whatever the stimulus the response itself is the same but the degree of response varies with the type and severity of the injury.
Vascular response
- The vascular response consists of transitory vasoconstriction followed by immediate vasodilation. This reaction is due to chemical mediators such as histamine, serotonin or kinins being released at the site of infection or injury.
- The mediator cause increase in blood flow to the area causing redness and heat.
- They also cause increased permeability of the capillaries which increase blood flow to the interstitial space. The extra fluid dilutes toxins and microorganism the area and serves as a vehicle by which phagocytes and nutrients needed for healing to reach the injured site.
Fluid exudation
- Fluid exudation from the capillaries into the interstitial spaces begins immediately and is most active during the first 24hours after.
- The exudate is serous fluid but the capillary walls become more permeable and proteins are lost into the interstitial spaces causing increased pressure in this space which encourages tissue swelling and oedema.
Cellular exudation
- It occurs when WBCS are summoned to the vessels in the affected area as a result of the release of chemostastic substance from injured cells and activation of complement.
- WBCS adhere to the capillary walls and migrate through the walls. Neutrophils are the first to respond usually within first few hours.
- Neutrophils ingest dead tissue cells and then die, releasing proteolytic enzyme that liquefy the dead neutrophils, dead bacteria and other dead cells forming pus.
Healing
The inflammatory response contains the spread of bacteria and prepares tissue for healing by two overlapping process: reconstruction and maturation. For repair to proceed, acute inflammation must subside and pus and dead tissue must be removed. Repair of wound involves three processes:
- Filling in the wound
- Sealing the wound
- Shrinking the wound
Reconstruction
- Once the inflamed area is clean or debrided, reconstruction begins and new cells are produced to fill in the space left by the injury.
- Fibroblast is attracted to the area which secret fibrin – a thread like structure that encircles the space.
Maturation
- Maturation follows reconstruction phase, during maturation which can last for months to years, scar is remodeled. Capillaries contract leaving a vascular scar and structure and function of damaged tissue are restored.
Types of inflammation
There are three main types of inflammation and its categorized by its duration and the type of exudate produced.
- Acute inflammation
- Chronic inflammation
- Sub-acute inflammation
ACUTE INFLAMMATION
An acute inflammation is one that starts rapidly and becomes severe in a short space of time. Signs and symptoms are normally only present for a few days but may persist for a few weeks in some cases.
The 5 Cardinal Signs (PRISH):
- Pain: The inflamed area is likely to be painful, especially during and after touching.
- Redness: This occurs because the capillaries in the area are filled with more blood than usual.
- Immobility: There may be some loss of function in the region of the inflammation.
- Swelling: This is caused by a buildup of fluid.
- Heat: More blood flows to the affected area, and this makes it feel warm to the touch.
Causes of Acute Inflammation
- Burns
- Chemical irritants
- Frostbite
- Toxins
- Infection by pathogens
- Physical injury, blunt or penetrating
- Immune reactions due to hypersensitivity
- Radiation
- Foreign bodies, including splinters, dirt and debris
- Trauma
Examples of diseases, conditions, and situations that can result in acute inflammation include:
- acute bronchitis
- infected ingrown toenail
- a sore throat from a cold or flu
- a scratch or cut on the skin
- high-intensity exercise
- acute appendicitis
- dermatitis
- tonsillitis
- infective meningitis
- sinusitis
- a physical trauma
CHRONIC INFLAMMATION
This refers to long-term inflammation and can last for several months and even years. It can result from:
- Failure to eliminate whatever was causing an acute inflammation.
- An autoimmune disorder that attacks normal healthy tissue.
- Exposure to a low level of a particular irritant, such as an industrial chemical, over a long period.
Examples of diseases and conditions that include chronic inflammation:
- Rheumatoid arthritis
- Asthma
- Chronic peptic ulcer
- Tuberculosis
- Periodontitis
- Ulcerative colitis and Crohn's disease
- Sinusitis
- Active hepatitis
| Acute | Chronic | |
|---|---|---|
| Caused by | Harmful bacteria or tissue injury | Pathogens that the body cannot break down, including some types of virus, foreign bodies that remain in the system, or overactive immune responses |
| Onset | Rapid | Slow |
| Duration | A few days | From months to years |
| Outcomes | Inflammation improves, turns into an abscess, or becomes chronic | Tissue death and the thickening and scarring of connective tissue |
Management of Inflammation
Investigation
- White blood cell count
- Bacteriological examination of specimen got from the site of infection.
- Serum tests for the presence of antibodies.
Common treatments
- Simple measures like fluid intake and rest can be considered to aid resolution.
- Antibiotics may be given to combat infection.
- Rest of the affected part.
- Surgical interventions may be necessary if all fails, excision and removal of necrotic tissue can be done.
- Incision and drainage may be done to drain pus.
- Rehabilitation is done to restore the functions.
Anti-inflammatory medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) can be taken to alleviate the pain caused by inflammation. Examples of NSAIDs include naproxen, ibuprofen, and aspirin.
- Acetaminophen, such as paracetamol or Tylenol, can reduce pain without affecting the inflammation.
- Corticosteroids, such as cortisol, are a class of steroid hormones that prevent a number of mechanisms involved in inflammation.
Inflammation diet
There are several foods that can have been shown to help reduce the risk of inflammation, including:
- olive oil, tomatoes, nuts, leafy greens, fatty fish, fruit.
Avoid eating foods that aggravate inflammation, including:
- fried foods, white bread, soda and sugary drinks, red meat, Margarine.