Table of Contents
TogglePhysical Examination of the Patient (PEX 2.3.3: Perform physical examination of the patient)
Objectives:
- Identify the requirements for assessing the patient.
- Prepare the requirements for assessing the patient.
- Carry out assessment of the patient.
- Define the term nursing process (part of 3.0).
- State the characteristics of the nursing process (part of 3.0).
- Describe the components of the nursing process (part of 3.0).
- Apply nursing process when giving nursing care (part of 3.0).
Definition:
Physical examination of a patient is done from head to toe and assessment of the major systems.
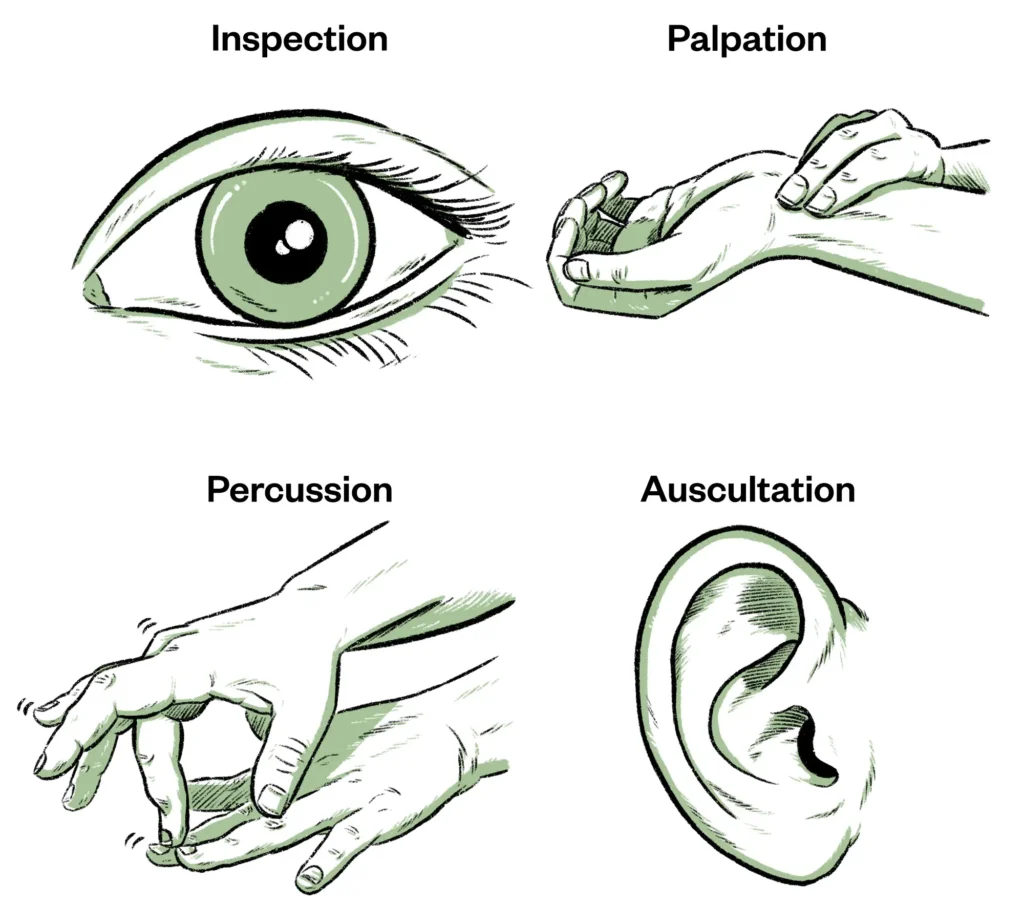
Physical Examination calls for 4 techniques :
- Inspection: Means looking at the client carefully to discover any signs of illness.
- Palpation: Means using hands to touch and feel. Different parts of hands are used for different sensations such as temperature, texture of skin, vibration, tenderness, etc. (e.g., fingertips for fine tactile surfaces, back of fingers for temperature, flat of palm and fingers for vibrations).
- Percussion: Determines the density of various parts of the body from the sound produced by them, when they are tapped with fingers. Helps find abnormal solid masses, fluid, and gas, and map out size and borders of organs. Methods include indirect percussion (tapping a finger placed on the body).
- Auscultation: Means listening to the sounds transmitted by a stethoscope, used to listen to the heart, lungs, and bowel sounds.

Functional health pattern approach (from 3.2):
Based on Gordon's functional health patterns, allows collection of data according to each pattern. Includes eleven health functional patterns (e.g., Health perception, Nutritional, Elimination, Activity/Exercise, Sleep/Rest, Cognitive/Perceptual, Self-perception, Role/Relationship, Sexuality/Reproductive, Coping/Stress, Value/Belief).
Requirements:
Same as for Taking History (from 3.1), particularly the Observation Tray contents and equipment for vital signs, measurements, and physical assessment tools.
Top Shelf (Observation Tray):
- Thermometer
- Watch (with seconds hand)
- Stethoscope
- Blood pressure machine (Sphygmomanometer)
- Neurological tray (Torch light/penlight, Spatula, Patella hammer, Otoscope, Tuning fork, Gallipot with cotton swabs/gauzes, Skin pencil, Snellens chart, Ophthalmoscope, Atropine 1% eye drops)
- Auroscope set (Jobson Horne ring probe, Wool and applicator, Dissecting aural forceps)
- Sterile throat swab
- Dental mirror laryngoscope
- Nasal speculum
- Alcohol swabs
- Lubricant
- Drape
- Vaginal speculum
- Disposal pads
Bottom Shelf:
- Record forms (History forms, assessment charts)
- Disposable gloves
- Specimen bottles
At the side:
- Weight scale (electronic or sling scale)
- Measuring tape
- Ruler
- Record chart
- Screen (for privacy)
- Examination table (if needed)
- Hand washing equipment
Special Senses Assessment tools (from 3.1.1/3.2):
- Bottle for cold and hot water (to test temperature sensation).
- Bottles with distinctive smelling liquids e.g. lavender (to test olfactory sense).
- Bottles with salt, sugar, bitter, and sour substances (to test taste sensation).
Procedure (General Physical Examination - Head to Toe Approach):
| Steps | Action | Rationale |
|---|---|---|
| 1. | Observe the general rules of nursing procedure. | Promotes adherence to standards. |
| 2. | Explain the purpose of the physical examination to the patient. Ensure privacy, provide adequate lighting, and assist the patient into a comfortable position. | To gain cooperation, reduce anxiety, and ensure a proper examination environment. |
| 3. | General Appearance: Observe overall appearance: posture, gait, movement, hygiene, state of nourishment, level of consciousness, and apparent age. Note any obvious changes or distress. | To identify obvious changes, assess mobility, hygiene, and overall health status. |
| 4. | Vital Signs: Measure temperature, pulse, respiration, and blood pressure. Obtain height and weight (as per procedure 3.1.2). | Provides baseline data on patient's physiological status. |
| 5. | Orientation & Cognitive Function: Observe patient's ability to respond to verbal commands, level of consciousness, orientation to person, place, and time. Note ability to think, remember, process information, and communicate. Note articulation on speech, style, and content. | Responses and cognitive processes indicate the patient's brain function and mental status. |
| 6. | Integumentary System (Skin, Hair, Nails): Inspect and palpate the skin: Note appearance, color, texture, sensation, moisture, temperature, turgor. Observe for any lesions, rashes, growths, trauma, edema. Check capillary refill by pressing the nail bed, noting the return of color. Assess hair for color, texture, growth, distribution. Inspect nails for color, shape, texture, and condition. | To assess the integrity and function of the skin, hair, and nails. Helps identify dehydration, anemia, circulation problems, or skin abnormalities. |
| 7. | Head: Inspect and palpate the head: Note size, shape, and symmetry. Palpate for any deformities, depressions, or tenderness. Inspect face for facial expression, asymmetry, involuntary movements, edema, and masses. | To detect abnormalities, assess for signs of paralysis, or masses. |
| 8. | Eyes: Inspect both eyes for position and alignment, symmetry, colour (sclera, conjunctiva). Observe pupils for size, shape, equality, and reaction to light (PERRLA). Test visual acuity (using Snellen chart if available). Observe ability to see. | To detect any abnormalities, assess visual function and neurological status related to the eyes. |
| 9. | Ears: Inspect and palpate ear shape, size, symmetry, and patency of the ear canal using an otoscope. Test hearing (e.g., whisper test or tuning fork tests). Observe ability to hear. | To detect abnormalities in ear structure and canal, and assess auditory function. |
| 10. | Nose: Inspect the anterior and inferior surface of the nose. Palpate the nose. Inspect the nasal vestibule with penlight; observe symmetry, size, flaring, and sensation. Observe ability to smell. | To detect any abnormalities or obstruction in the nasal passages. |
| 11. | Mouth: Observe lips, mucous membrane, gum, tongue, teeth, and palate for color, moisture, texture, and sensation. Inspect the throat (uvula, tonsils, pharynx) using a penlight and tongue depressor. Observe ability to taste. | To detect any abnormalities or signs of infection in the oral cavity and throat. |
| 12. | Neck: Inspect and palpate the neck: Note symmetry, range of motion. Inspect and palpate the lymph nodes (pre-auricular, post-auricular, occipital, tonsillar, submandibular, submental, superficial cervical, posterior cervical, deep cervical chain, supra clavicular) for location, size, shape, texture, and pain. Inspect and palpate jugular veins. Inspect and palpate thyroid gland for enlargement, contour, and symmetry. Ask patient to swallow while palpating the thyroid. | To detect enlargement of lymph nodes (infections/conditions), assess jugular venous distension (JVD - indicates increased venous pressure), and assess thyroid abnormalities. |
| 13. | Chest, Lungs, and Heart: Inspect chest movement and symmetry during breathing. Palpate chest. Auscultate lung sounds in all lobes (anterior, posterior, lateral) for normal breath sounds and adventitious sounds (crackles, wheezes). Percuss the chest. Auscultate heart sounds (rate, rhythm, murmurs) at the appropriate locations. | To assess respiratory and cardiovascular function and detect abnormalities such as congestion or abnormal heart rhythms. |
| 14. | Breasts and Axilla: Inspect breasts appearance, color, size, symmetry, shape, and texture. Palpate breasts for lumps or tenderness. Inspect nipples for symmetry, shape, dry scaling, fissure, ulceration, bleeding or other discharge. Inspect and palpate axilla for lymph nodes. | To detect any abnormalities, lumps, or signs of infection/inflammation. |
| 15. | Abdomen: Assist patient to lie in supine position with knees slightly flexed (if possible) to relax abdominal muscles. Inspect the abdomen: Note skin color, symmetry, shape, distension. Observe pulsations from the aorta (if visible). Auscultate bowel sounds in all four quadrants (presence, character, frequency). Percuss the abdomen for tone. Palpate the abdomen (light and deep palpation) for tenderness, masses, and size/consistency of organs (liver, spleen, kidneys). | To assess abdominal function, detect abnormalities such as distension, abnormal bowel sounds, tenderness, masses, or organ enlargement. |
| 16. | Musculoskeletal System: Inspect and palpate neck, shoulders, arms, hands, hips, knees, legs, ankles, and feet for symmetry, size, contour of joints, skin condition, tenderness, swelling, or deformities. Assess range of motion (active and passive) of all major joints, noting any pain or limitation. Assess muscle strength and tone. Observe gait. | To detect swelling, deformities, pain, and limitations in movement. Assesses functional mobility. |
| 17. | Neurological System: Assess level of consciousness (already done in step 5), orientation, cognitive function. Assess cranial nerves. Assess motor function (strength, coordination, balance). Assess sensory function (light touch, pain, temperature, vibration, position). Assess reflexes. | To assess the function of the nervous system and detect any deficits. |
| 18. | Thank the patient for their cooperation and assist them back to a comfortable position. Dispose of used materials and clean equipment. Wash hands. | To conclude the examination respectfully and maintain hygiene. |
| 19. | Document findings accurately and completely on the patient's chart. Report any significant or abnormal findings immediately to the doctor. | For continuity of care, monitoring, and legal record. |
Nurses Revision