Stye or Hordeolum
A stye is a painful, red lump that forms on the edge of the eyelid. It is an acute infection of a small gland in the eyelid, most commonly caused by the bacterium Staphylococcus aureus. The medical term is Hordeolum.
A stye is a localized infection of the hair follicles or sebaceous glands of the eyelids.
A stye is a staphylococcal abscess that may occur on either the external or internal margin of the eyelids.
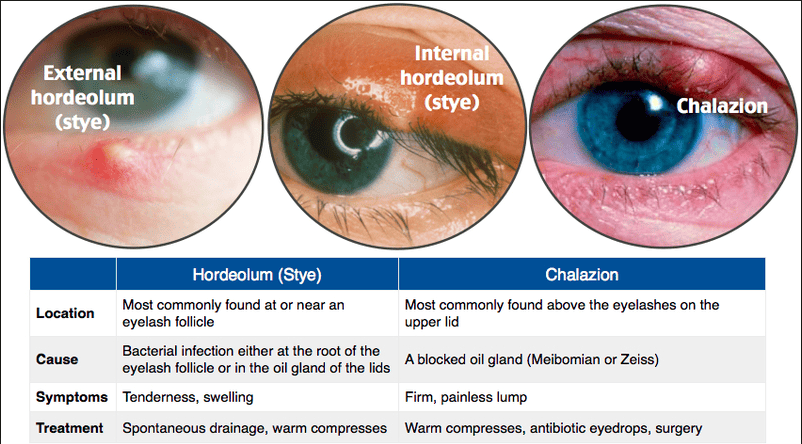
Types of Stye
External Stye (Hordeolum Externum)
This is the most common type, appearing on the outer edge of the eyelid. It is an infection of an eyelash follicle or a gland of Zeis or Moll. External styes are generally more painful than internal styes because they form on the surface of the eyelid, often along the lash line, involving many nerve endings, making them tender and noticeable.
- Location: Outer edge of the eyelid, at the lash line.
- Cause: Acute bacterial infection of an eyelash follicle or a sebaceous gland (Gland of Zeis or Moll).
- Pain Level: Typically more acutely painful, sharp, and localized tenderness.
- Appearance: Often resembles a small, red, tender pimple or boil, sometimes with a visible head.
Internal Stye (Hordeolum Internum)
This forms on the inner surface of the eyelid and is an infection of a Meibomian gland (an oil-producing gland within the eyelid). Unlike external styes, the pain from an internal stye is often described as a more generalized ache or pressure rather than sharp, localized pain, and they tend to be less acutely painful. However, they can cause more significant and diffuse swelling of the entire eyelid. Internal styes may sometimes require medical intervention for drainage as they are less likely to rupture on their own and tend to recur.
- Location: Inner surface of the eyelid, often causing swelling across the entire eyelid.
- Cause: Acute bacterial infection of a Meibomian gland.
- Pain Level: Less acutely painful than external styes, often a generalized ache or pressure.
- Appearance: Can cause significant, diffuse swelling of the eyelid; the lump may be felt or seen when the eyelid is everted.
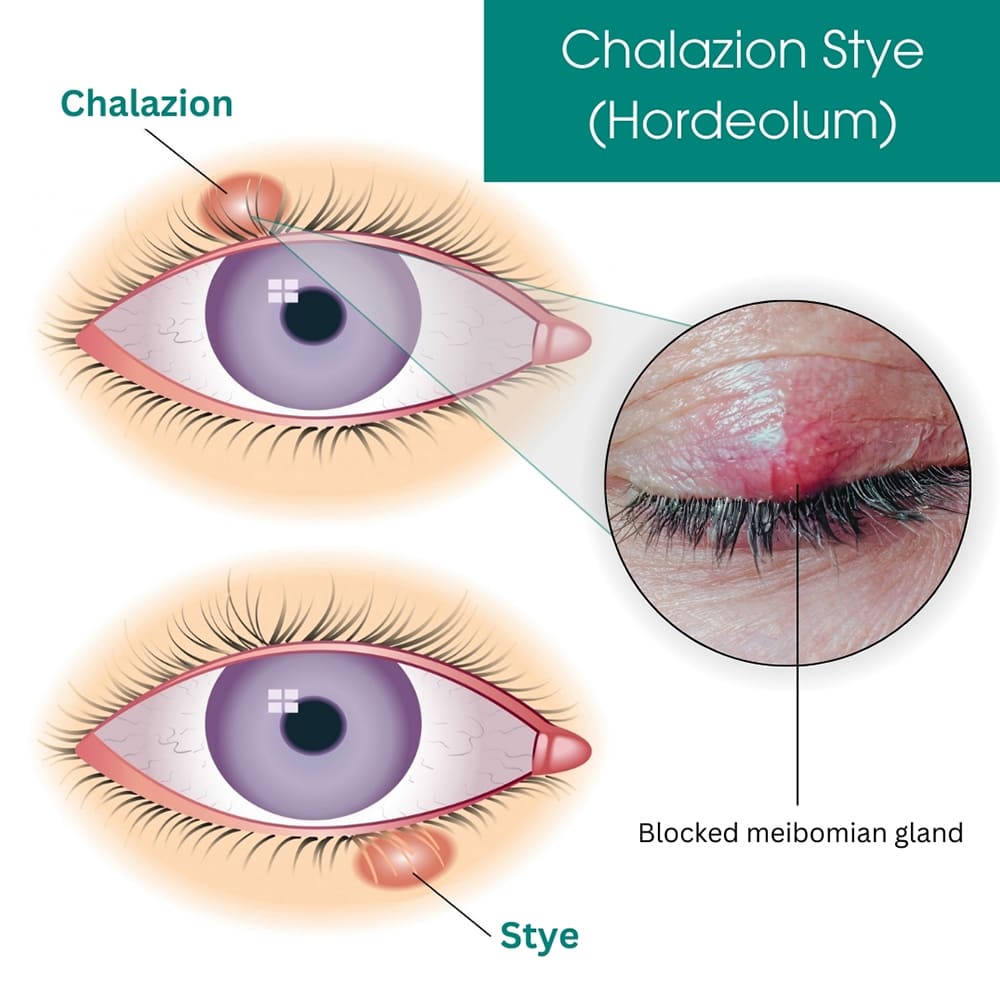
Chalazion
A chalazion is not a type of stye, but rather a chronic, non-infectious lump in the eyelid. It often develops when an internal stye doesn't fully resolve, or when a Meibomian gland becomes blocked and its contents (oil) are released into the surrounding tissue, causing sterile inflammation. Unlike styes, chalazia are typically painless once the initial inflammation subsides, although they can cause cosmetic concerns or, if large enough, temporary blurred vision by pressing on the cornea.
- Location: Usually forms deeper in the eyelid, away from the lid margin.
- Cause: Blocked Meibomian gland, leading to sterile inflammation; often a sequela of an untreated internal stye.
- Pain Level: Generally painless and non-tender after the initial inflammatory phase subsides.
- Appearance: A firm, round, non-tender lump in the eyelid; typically no acute redness unless secondarily infected.
Clinical Features (Signs and Symptoms)
The signs and symptoms of a stye are very distinct. You will see and hear the following from your patient:
- A visible lump: A noticeable red lump appears on the top or bottom eyelid.
- Swelling and Redness: The area is red and swollen. Sometimes a small area is affected, but sometimes the entire eyelid swells up.
- Pain and Tenderness: The lump is painful, and it is tender when touched.
- Itching and Burning: Patients often complain of itching in the early stages, as well as a burning sensation in the eye.
- Pus Formation: A tiny, yellowish spot (pus point) develops at the center of the swollen area after 2-3 days, right before it may burst spontaneously.
- Eye Discomfort: Patients feel a gritty sensation, as if a foreign body is in the eye. There is also discomfort during blinking.
- Watering and Discharge: The eye may water excessively (tearing) and can have mucous discharge. This can lead to crusting of the eyelid margins, especially upon waking.
- Sensitivity to Light (Photophobia): The eye becomes very sensitive to bright light.
- Blurred Vision: In some cases, vision may be temporarily blurred due to the swelling or discharge.
In summary,
Management of a Stye
The goals are to
- Usually the stye will heal spontaneously
- Avoid rubbing the eye as this might spread the infection
- Apply a warm/ hot compress to the eye for 10 minutes
- Apply tetracycline eye ointment 1% 2-4 times daily until 2 days after symptoms have disappeared
- Remove the eye lash when it’s loose
- When the forms in one of the deeper glands of the eyelid a condition is called internal hordeolum
- The pain and other symptoms are usually more severe.
- Because this type of the stye rarely ruptures by it self, a doctor may have to open it to drain the pus
Immediate and Home Care (Conservative Management)
- Warm Compresses: This is the most important treatment. Apply a clean cloth soaked in warm water to the closed eye for 10-15 minutes, 3-4 times a day. This helps drainage.
- Lid Hygiene: Gently clean the eyelid margins to remove crusts and bacteria.
- Important Advice: Tell the patient to NEVER squeeze or rub the stye, as this can spread the infection deeper.
- Eyelash Removal: You can gently remove an eyelash if it is loose and coming directly from the center of the stye, as this can help it drain.
Medical Management
- Topical Antibiotics: A clinician may prescribe Tetracycline 1% eye ointment or Chloramphenicol eye ointment, applied 2-4 times daily until 2 days after symptoms have disappeared.
- Pain Relief: Simple analgesics like Paracetamol can be used for pain.
- Oral Antibiotics: These are reserved for severe infections or if the infection spreads to the surrounding skin (preseptal cellulitis).
Surgical Management
- Incision and Drainage (I&D): This procedure is performed if resolution does not begin in the next 48 hours after warm compresses are started, especially for a painful internal hordeolum.
- Procedure: The procedure consists of the doctor numbing the area, making a very small incision on the inner or outer surface of the eyelid, and draining the pus. Very small sutures may be used to close the lesion.
Nursing Interventions
Your role as a nurse is central to effective management and prevention.
Nursing Care Plan
| Assessment | Nursing Diagnosis | Planning (Goals) | Implementation: Interventions | Implementation: Rationale | Evaluation |
|---|---|---|---|---|---|
| Subjective: Patient states, "My eyelid is very sore." Objective: Localised, red, swollen, tender lump on the upper eyelid margin. |
Acute Pain related to the inflammatory process and pressure from abscess as evidenced by patient's verbal report and tenderness on palpation. | Patient will report a reduction in pain within 24 hours. Patient will demonstrate correct application of warm compress. | 1. Teach and demonstrate application of warm compresses for 10-15 mins, 4x daily. 2. Administer prescribed analgesics. 3. Advise patient to avoid touching the stye. |
1. Heat promotes drainage, which relieves pressure and pain. 2. Analgesics provide systemic pain relief. 3. Pressure worsens pain and risks spreading infection. |
Goal Met. Patient reports pain has decreased and correctly shows how to apply a warm compress. |
| Objective: Patient wears contact lenses and heavy eye makeup. Asks, "Why do I keep getting these?" | Deficient Knowledge related to disease process, self-care, and prevention strategies as evidenced by patient's question and identified risk factors. | By end of session, patient will verbalize 3 key preventive measures. | 1. Educate on strict hand hygiene. 2. Instruct on not sharing cosmetics/towels. 3. Advise to remove makeup nightly and discard old products. 4. Instruct to avoid wearing contact lenses until healed. |
1. Reduces bacterial transfer to the eye. 2. Prevents cross-contamination. 3. Empowers patient to modify risk factors and prevent recurrence. 4. Prevents trapping bacteria and irritating the eye. |
Goal Met. Patient correctly lists hand washing, not sharing makeup, and removing makeup as preventive measures. |
| Objective: Pus point is visible on the stye. Patient lives in close quarters with siblings. | Risk for Infection related to the presence of an active bacterial lesion and potential for poor hygiene. | Patient and family will remain free from signs of spreading infection throughout the illness. | 1. Emphasize that personal items (towels) must not be shared. 2. Instruct to wash hands after touching the eye or applying medication. 3. Teach correct application of antibiotic ointment if prescribed. |
1. Staph bacteria are easily transmitted via contaminated items. 2. Prevents auto-inoculation and spreading to others. 3. Topical antibiotics treat the local infection and reduce bacterial load. |
Goal Met. The stye resolved without spreading. No other family members developed styes. |
Complications
- Chalazion: An internal stye may heal and leave a painless lump.
- Preseptal Cellulitis: The infection spreads to the whole eyelid. This needs urgent antibiotic treatment.
- Orbital Cellulitis: A medical emergency where the infection goes behind the eye. Refer immediately.
- Recurrence: Styes can come back, especially with poor hygiene.
Prevention
- Good Personal Hygiene: Proper and regular hand washing is the most important preventive measure.
- Face Washing: Keep the face, especially the eye area, clean.
- Makeup Hygiene: Never share cosmetics or eye makeup tools. Remove all makeup every night. Discard old or contaminated eye makeup (every 3-6 months).
- Do Not Share Personal Items: Avoid sharing towels, flannels, or pillowcases.
- Good personal hygiene,Proper hand washing
- Regular washing of the face
- Remove any loose eyelashes
- it is recommended to never share cosmetics or cosmetic eye tools with other people
- It is also recommended to remove makeup every night before going to sleep and discard old or contaminated eye makeup.


Very interestingnly nice,I enjoyed the I fo.
very nice topic
Very nice and precise work
Thanks for giving us such essential information bro
Have learned a lot from the topic
Easy and summarised work
Nice work good job done
thanks a lot for the knowledge