Death caused by self-directed injurious behavior with any intent to die as a result of the behavior.
Suicide refers to deliberate act of self harm that result into death.
NB: The critical component here is the intent to die. It's not merely self-harm, but self-harm carried out with the aim of ending one's life. Suicide refers to the act itself.
- Suicidal Ideation (SI): Thinking about, considering, or planning suicide. This can range from fleeting thoughts that life is not worth living to detailed planning of how to end one's life. Spectrum includes:
- Passive Suicidal Ideation: A desire to die, but without a specific plan or active intent to act (e.g., "I wish I wouldn't wake up," "I wish I could disappear").
- Active Suicidal Ideation: Thoughts of taking one's own life, often accompanied by specific plans, methods, and a timeline.
- Suicide Attempt: A non-fatal self-directed injurious behavior with any intent to die as a result of the behavior.
- Note: Similar to suicide, the intent to die is central. However, in this case, the attempt was unsuccessful, meaning the individual survived.
- Non-Suicidal Self-Injury (NSSI) (also known as Self-Harm or Self-Mutilation): Direct, deliberate destruction of body tissue without suicidal intent. This includes behaviors like cutting, burning, scratching, hitting oneself, or interfering with wound healing.
- Note: The absence of intent to die. The purpose of NSSI is to cope with intense emotional pain, to feel something when numb, to punish oneself, to escape a difficult situation, or to exert control.
- Suicide: Self-inflicted death with intent to die.
- Suicidal Ideation: Thoughts or plans about ending one's life.
- Suicide Attempt: Self-inflicted injury with intent to die, but not resulting in death.
- Non-Suicidal Self-Injury (NSSI): Self-inflicted injury without intent to die, usually to cope with distress.
Suicide is a major global public health concern. The World Health Organization (WHO) reports that it is one of the leading causes of death worldwide.
- Mortality Rate: Globally, close to 800,000 people die by suicide every year. This translates to one death every 40 seconds.
- Age Group Impact: Suicide is the fourth leading cause of death among 15-29-year-olds globally.
- Completed Suicides: Globally, suicide rates are generally higher among men than women in most countries (often 2-4 times higher). Men tend to use more lethal means. Suicide Attempts: Women are more likely to attempt suicide than men, though men are more likely to die by suicide.
- Underreporting: Due to stigma, legal issues, and difficulties in determining intent, suicide is often underreported or misclassified, meaning the true numbers may be even higher.
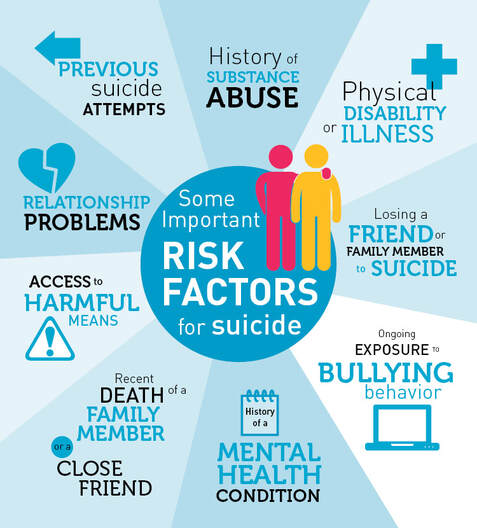
These factors rarely act in isolation; rather, they often interact and accumulate, increasing an individual's vulnerability. Risk factors can be broadly categorized as follows:
These are statistical associations that indicate certain groups may have higher rates of suicide.
- Age: Adolescents and young adults (15-29 years) are at elevated risk globally. Older adults (especially men over 75) also represent a high-risk group.
- Gender: Men die by suicide more often than women. Women attempt suicide more often than men.
- Sexual Orientation/Gender Identity: LGBTQ+ individuals, particularly youth, often face higher rates due to discrimination, stigma, and lack of support.
- Socioeconomic Status: Poverty, unemployment, financial strain, and homelessness are associated with increased risk.
- Marital Status: Single, divorced, or widowed individuals may be at higher risk than married individuals.
These are among the strongest and most consistently identified risk factors.
- Mood Disorders: Major Depressive Disorder (MDD), Bipolar Disorder (especially during depressive or mixed episodes).
- Substance Use Disorders: Alcohol and drug abuse significantly impair judgment, increase impulsivity, and exacerbate underlying mental health issues.
- Schizophrenia and Psychotic Disorders: Increased risk due to command hallucinations, paranoia, and social isolation.
- Anxiety Disorders: Severe anxiety, panic disorder, PTSD.
- Eating Disorders: Anorexia Nervosa and Bulimia Nervosa.
- Personality Disorders: Borderline Personality Disorder (BPD) is strongly associated with self-harm and suicide attempts due to emotional dysregulation, impulsivity, and relationship difficulties.
These factors relate to an individual's external circumstances and social connections.
- Loss of a loved one (bereavement), especially by suicide (suicide contagion/cluster).
- Relationship problems (divorce, breakup).
- Job loss, financial collapse.
- Legal problems, incarceration.
- Bullying, cyberbullying.
While less understood than psychological and social factors, biological predispositions play a role.
- Genetics: A family history of suicide or mental illness suggests a genetic predisposition, though the exact mechanisms are complex.
- Neurobiology: Imbalances in neurotransmitters (e.g., serotonin) and alterations in brain structure and function are implicated, particularly in mood disorders.
- Chronic Pain: As mentioned above, it can have biological impacts that contribute to depression and suicidal ideation.
This theory posits that people will not die by suicide unless they have both the desire to die and the acquired capability to inflict lethal self-injury.
- Thwarted Belongingness: Feeling alone, isolated, alienated.
- Perceived Burdensomeness: Feeling like a burden on others.
- Examples: History of self-harm, repeated exposure to violence, military combat, medical procedures.
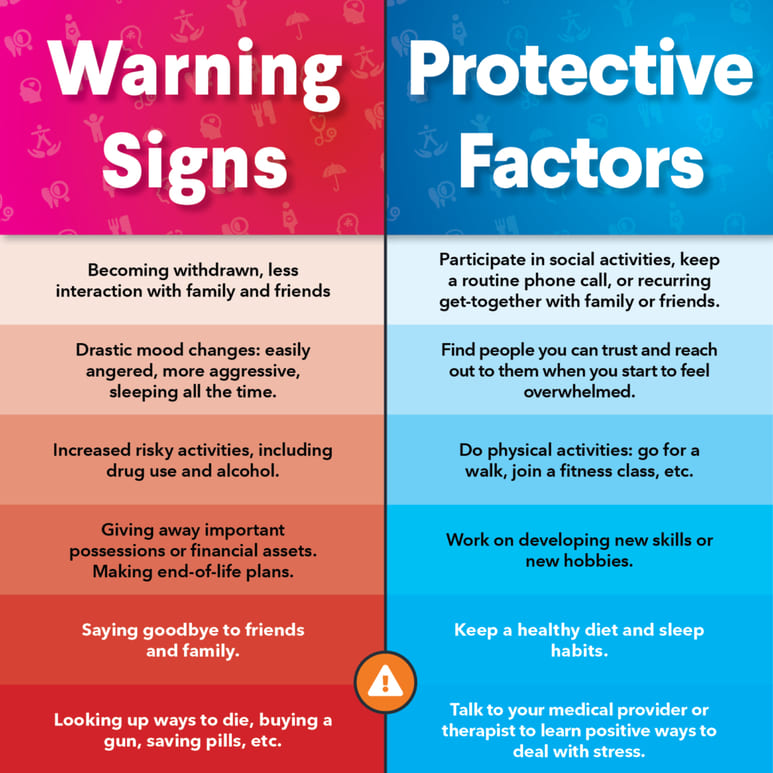
Protective factors are characteristics or conditions that reduce the likelihood of a person developing a mental health condition, or reduce the impact of existing mental health conditions, thereby buffering against the risk of suicide. While risk factors highlight vulnerabilities, protective factors emphasize strengths and resources.
These factors can exist at individual, relational, community, and societal levels.
These are personal strengths and coping resources.
- Problem-solving skills: Ability to identify and effectively resolve problems.
- Emotion regulation skills: Ability to manage intense emotions without resorting to destructive behaviours.
- Distress tolerance: Capacity to withstand and cope with painful or uncomfortable emotions.
These involve supportive relationships and social connections.
- Supportive Family Environment: Positive relationships with family members, open communication, a sense of belonging and being cared for.
- Supportive Friends/Peers: Close friendships, feeling understood and accepted by peers.
- Mentors/Trusted Adults: Presence of adults (teachers, coaches, community leaders) who provide guidance and support.
These relate to the broader environment and available resources.
- Access to Quality Mental Health Care: Availability and accessibility of mental health services, including crisis intervention, therapy, and psychiatric care.
- Access to Physical Healthcare: Good overall healthcare infrastructure.
- Reduced Access to Lethal Means: Policies and practices that make it harder for individuals in crisis to access methods for suicide (e.g., safe storage of firearms, medication safety, bridge barriers).
- Support for Seeking Help: A community culture that encourages help-seeking and reduces the stigma associated with mental health issues.
- Effective School and Community-Based Mental Health Programs: Programs that promote mental wellness, teach coping skills, and provide support to young people.
- Positive School Environment: Schools that are safe, inclusive, and promote a sense of belonging.
- Cultural and Religious Institutions: For some, these institutions provide strong social networks, values, and support systems.
- Stable Housing and Employment: Basic needs being met contribute to overall well-being.
- Policies that Reduce Economic Hardship: Social safety nets that provide support during times of financial difficulty.
- Responsible Media Reporting of Suicide: Guidelines for media to report on suicide in a way that minimizes contagion effects and promotes help-seeking.
Warning signs are observable behaviors or statements that indicate an immediate and acute risk of suicide. It is important to take these signs seriously and act promptly.
Warning signs can be remembered by the acronym "IS PATH WARM?" (developed by the American Association of Suicidology).
- I - Ideation:
- Talking about wanting to die, kill oneself, or end one's life.
- Expressing feelings of hopelessness or having no reason to live.
- Searching for ways to kill oneself (e.g., online searches for methods, acquiring weapons or pills).
- Making specific plans for suicide.
- S - Substance Abuse:
- Increased or excessive use of alcohol or drugs.
- Misuse of prescription medication.
- Substance abuse can lower inhibitions, impair judgment, and intensify suicidal thoughts.
- P - Purposelessness:
- Feeling that there is no reason to live, no purpose in life.
- Feeling trapped, like there's no way out of a difficult situation.
- Feeling like a burden to others.
- A - Anxiety:
- Experiencing extreme anxiety, agitation, or being unable to sleep.
- Feeling restless or on edge.
- T - Trapped:
- Feeling trapped or feeling like there's no way out of a situation.
- A sense of being caught in an unbearable circumstance.
- H - Hopelessness:
- Having no hope for the future, believing that things will never get better.
- A pessimistic outlook on life and circumstances.
- W - Withdrawal:
- Withdrawing from friends, family, and social activities.
- Becoming isolated or preferring to be alone.
- Loss of interest in activities previously enjoyed.
- A - Anger:
- Exhibiting rage, uncontrolled anger, seeking revenge.
- Irritability or extreme mood swings.
- R - Recklessness:
- Engaging in reckless or risky behaviors without thinking of consequences.
- Excessive thrill-seeking that is out of character.
- M - Mood Changes:
- Dramatic shifts in mood, sudden changes from deep sadness to calm or happiness (which can sometimes indicate a decision to commit suicide has been made).
- Severe depression, anhedonia (inability to feel pleasure).
- Giving away prized possessions.
- Saying goodbye to friends and family.
- Writing a will or suicide note.
- "Getting affairs in order."
Suicide risk assessment and screening are systematic processes used by mental health professionals, healthcare providers, and trained individuals to identify individuals at risk of suicide, evaluate the severity of that risk, and determine the appropriate level of intervention.
- Purpose: To quickly identify individuals who might be at risk for suicide and require further evaluation. It's a brief initial step.
- Method: Often involves short questionnaires or a few direct questions (e.g., "In the past few weeks, have you wished you were dead or thought you would be better off dead?").
- Who: Can be conducted by various healthcare providers (nurses, primary care physicians, social workers) in different settings (clinics, emergency departments, schools).
- Outcome: Identifies individuals who need a more comprehensive suicide risk assessment. A positive screen does not mean a person is suicidal, but indicates a need for deeper inquiry.
- Purpose: To conduct a comprehensive evaluation of an individual's suicidal ideation, intent, plan, and overall risk factors and protective factors to determine the imminence and severity of suicide risk. This informs clinical decision-making.
- Method: A detailed clinical interview, often structured or semi-structured, conducted by a trained mental health professional. It integrates information from various sources (patient interview, family reports, medical records, collateral information).
- Who: Primarily conducted by psychiatrists, psychologists, licensed clinical social workers, psychiatric nurse practitioners, or other mental health specialists.
- Outcome: Develops a risk formulation and a safety plan, and determines the appropriate level of care (e.g., outpatient therapy, intensive outpatient program, inpatient hospitalization).
A thorough assessment typically covers the following areas:
- Suicidal Ideation:
- Frequency, Intensity, Duration: How often do thoughts occur? How strong are they? How long do they last?
- Content: Specific phrases, images, or scenarios.
- Controllability: Can the person stop the thoughts?
- Passive vs. Active Ideation: Distinguishing between wishing to be dead and active thoughts of taking one's life.
- Suicide Plan:
- Specificity: How detailed is the plan?
- Lethality: How deadly is the chosen method (e.g., firearms vs. superficial cuts)?
- Accessibility: Does the individual have immediate access to the means specified in the plan?
- Preparatory Behaviors: Has the person taken steps to prepare (e.g., acquiring means, writing notes, giving away possessions)?
- Suicide Intent:
- Motivation: Why does the person want to die?
- Expectation of Outcome: Does the person expect to die from the plan?
- Ambivalence: Is there a part of them that wants to live? How strong are these conflicting feelings?
- Previous Suicide Attempts:
- Details of past attempts: number, methods, lethality, intent, circumstances, and whether they sought help afterward. (This is the strongest predictor of future attempts).
- Risk Factors:
- Mental health diagnoses (especially depression, bipolar disorder, substance use, psychosis, BPD).
- History of trauma or abuse.
- Family history of suicide.
- Significant recent losses or stressors.
- Chronic physical illness or pain.
- Social isolation.
- Impulsivity, hopelessness, agitation.
- Protective Factors:
- Reasons for living.
- Strong social support.
- Religious or spiritual beliefs.
- Effective coping skills.
- Sense of responsibility to family/pets.
- Access to mental health care.
- Current Mental State:
- Presence of psychosis, severe anxiety, agitation, intoxication.
- Ability to think clearly and make rational decisions.
- Support System:
- Availability and willingness of family/friends to provide support.
Read (SAD PERSONS SCALE) for Practicals
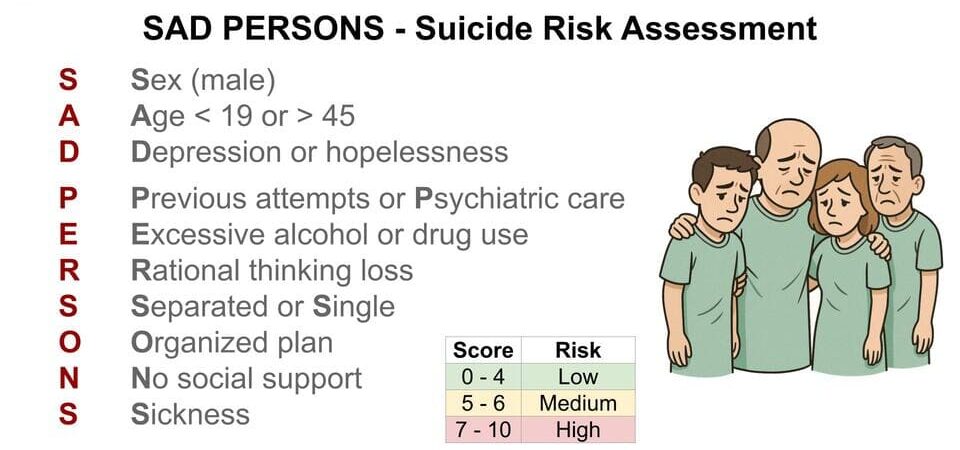
While a clinical interview is paramount, several tools can aid the process:
- PHQ-9 (Patient Health Questionnaire-9): Includes a question about suicidal thoughts (question 9).
- Columbia-Suicide Severity Rating Scale (C-SSRS) - Screener Version: A brief, structured tool used in many settings.
- ASQ (Ask Suicide-Screening Questions) Tool: Brief 4-question screen for medical settings.
- SAD PERSONS Scale: A mnemonic to remember risk factors, often used in emergency settings (though its predictive validity is limited).
- C-SSRS - Full Version: Comprehensive interview for assessing suicide ideation and behavior.
- Beck Scale for Suicide Ideation (BSSI): Self-report or clinician-rated scale.
- Structured Clinical Interview for DSM-5 (SCID): Covers suicidal ideation in detail within mental health diagnoses.
Crisis intervention focuses on providing immediate, short-term support during an acute suicidal crisis, while safety planning is a proactive, collaborative process to help individuals manage future suicidal urges. Both are vital components of suicide prevention.
Crisis intervention aims to stabilize the individual, reduce immediate danger, and connect them with ongoing support. Key principles include:
- Establish Rapport and Trust: Create a safe, non-judgmental space. Be empathetic, listen actively, and convey acceptance.
- Assess Imminent Risk:
- Directly ask about suicidal thoughts, intent, and plan.
- Determine if there's a specific plan, access to means, and a timeframe.
- Evaluate impulsivity, hopelessness, and substance use.
- Ensure Safety:
- Remove Lethal Means: If possible and safe, help remove access to firearms, excessive medication, ropes, etc. This is a critical immediate step.
- Do Not Leave Alone: If risk is high, ensure the person is not left unsupervised.
- Hospitalization: If the risk of harm is imminent and uncontrollable, psychiatric hospitalization may be necessary to ensure safety and provide intensive care. This is a last resort but essential when other options are insufficient.
- Listen and Validate: Allow the person to express their pain without judgment. Validate their feelings, even if you don't agree with their conclusions (e.g., "I hear how much pain you're in, and it makes sense that you feel trapped").
- Offer Hope: Gently remind them that feelings are temporary, and help is available. Focus on reasons for living or things they care about.
- Mobilize Support:
- Involve trusted family members or friends (with the individual's consent if possible, but safety is paramount).
- Connect them with crisis hotlines, emergency services, or mental health professionals.
- Problem-Solving (Short-Term): Focus on immediate steps to get through the crisis, rather than long-term solutions.
A safety plan is a personalized, written list of coping strategies and sources of support that individuals can use when they experience suicidal thoughts or urges. It is developed collaboratively with a clinician and the individual at risk. Unlike a "no-suicide contract" (which is largely ineffective and often discouraged), a safety plan focuses on actionable steps and personal resources.
- Warning Signs:
- What are the specific thoughts, images, feelings, or situations that indicate a crisis may be developing? (e.g., "When I start isolating myself, feel overwhelming guilt, or can't sleep.")
- Internal Coping Strategies:
- What can the individual do on their own to distract themselves or soothe themselves without contacting another person?
- Examples: Listening to music, reading, going for a walk, mindfulness exercises, journaling, watching a favorite movie, engaging in a hobby.
- Social Contacts Who Provide Distraction:
- Who can the individual contact to talk to or do something with to distract from suicidal thoughts, but without discussing the suicidal thoughts?
- Examples: A friend for coffee, a family member for a movie, a colleague for a chat about work.
- Family Members or Friends Who Can Provide Support:
- Who can the individual contact and talk to about their suicidal feelings and ask for help?
- Examples: A trusted family member, a close friend, a partner, a spiritual leader. Include their names and phone numbers.
- Mental Health Professionals and Agencies:
- Who are the professionals or agencies the individual can contact for help during a crisis?
- Examples: Therapist's name/number, psychiatrist's name/number, local mental health clinic, crisis hotline (e.g., 988 Suicide & Crisis Lifeline). Include specific phone numbers.
- Making the Environment Safe (Reducing Access to Lethal Means):
- What steps can be taken to reduce access to means that could be used for self-harm?
- Examples: Removing firearms from the home, giving medications to a trusted person to dispense, securing sharp objects, avoiding certain locations. This section is often reviewed and updated regularly.
Treatment approaches for suicidal individuals focus on addressing mental health disorders, enhancing coping skills, improving overall well-being, and directly targeting suicidal thoughts and behaviors. A comprehensive approach often involves a combination of psychotherapy, pharmacotherapy, and other supportive interventions.
Several evidence-based psychotherapies have demonstrated effectiveness in reducing suicidal ideation and behaviors.
- Cognitive Behavioral Therapy (CBT):
- Focus: Helps individuals identify and change distorted thinking patterns and maladaptive behaviors that contribute to distress and suicidal thoughts.
- Techniques: Cognitive restructuring (challenging negative thoughts), behavioral activation (increasing engagement in enjoyable activities), problem-solving skills training, and coping skills development.
- How it helps with suicide risk: Addresses hopelessness, improves problem-solving, and teaches skills to manage intense emotions.
- Dialectical Behavior Therapy (DBT):
- Focus: Originally developed for individuals with Borderline Personality Disorder, who often struggle with chronic suicidality and self-harm.
- Techniques: Emphasizes skill-building in four key areas:
- Mindfulness: Being present and aware.
- Distress Tolerance: Coping with painful emotions without acting on them.
- Emotion Regulation: Understanding and managing intense emotions.
- Interpersonal Effectiveness: Improving communication and relationships.
- How it helps with suicide risk: Directly targets suicidal urges and self-harm behaviors by teaching concrete skills to manage emotional crises.
- Collaborative Assessment and Management of Suicidality (CAMS):
- Focus: A therapeutic framework where the patient and clinician work together as a team to develop and implement a suicide-focused treatment plan.
- Techniques: Utilizes a "Suicide Status Form" (SSF) to track suicidal ideation, identify drivers of suicidality, and collaboratively create a treatment plan that addresses these drivers. The patient is seen as the expert on their own suicidal experience.
- How it helps with suicide risk: Directly and consistently engages with the patient's suicidality, fostering a strong therapeutic alliance and focusing on resolving the core reasons for wanting to die.
- Brief Cognitive Behavioral Therapy (BCBT) for Suicide Prevention:
- Focus: A time-limited, goal-oriented CBT intervention specifically adapted for acute suicidal crises.
- Techniques: Focuses on developing a safety plan, identifying triggers, enhancing coping skills, and preventing future crises.
Medications are often used in conjunction with psychotherapy, especially when underlying mental health disorders (like depression, bipolar disorder, or anxiety) are present.
- Antidepressants: Treat major depressive disorder, which is a significant risk factor for suicide. Requires careful monitoring, especially in children, adolescents, and young adults, due to a black box warning about a possible transient increase in suicidal thoughts/behaviors early in treatment for a small subset of individuals. This risk is generally outweighed by the long-term benefits of treating depression.
- Mood Stabilizers: For Bipolar Disorder, which has a very high suicide risk. Lithium is notably the only medication with consistent evidence of reducing suicide rates, specifically in individuals with mood disorders.
- Antipsychotics: For psychotic disorders (e.g., schizophrenia) that are associated with increased suicide risk. Clozapine is an atypical antipsychotic shown to reduce suicide risk in patients with schizophrenia.
- Anxiolytics: For severe anxiety, but generally used short-term due to dependence potential. Not a primary suicide prevention medication.
- Electroconvulsive Therapy (ECT): Highly effective for severe, treatment-resistant depression, especially when psychotic features are present, or when rapid reduction of suicidal ideation is needed in an acute crisis.
- Transcranial Magnetic Stimulation (TMS): A non-invasive brain stimulation technique approved for treatment-resistant depression.
- Hospitalization (Inpatient/Partial Hospitalization Programs): Provides a safe, structured environment for individuals at high risk of suicide. Partial hospitalization offers intensive day treatment while allowing patients to return home at night.
- Support Groups: Connects individuals with shared experiences, reducing isolation and fostering hope. Examples include groups for depression, addiction, or suicide attempt survivors.
- Case Management and Coordinated Care: Ensures that individuals receive comprehensive and integrated care across different providers and settings.
Suicide prevention refers to a range of efforts to reduce the risk of suicide, while postvention focuses on providing support to individuals and communities affected by suicide. Both are crucial for a comprehensive public health approach to mental wellness.
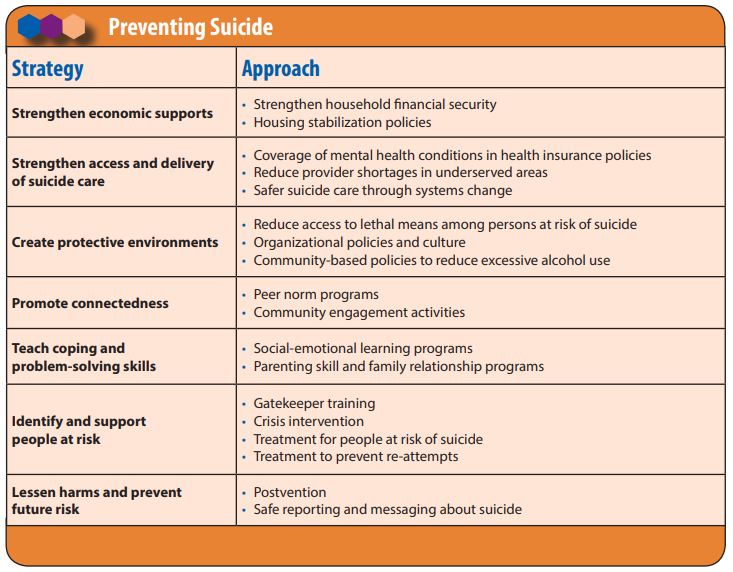
Prevention strategies operate at multiple levels – individual, relational, community, and societal – to address risk factors and enhance protective factors.
- Promoting Connectedness and Social Support:
- Community Programs: Fostering community engagement, social activities, and support networks.
- Mentorship Programs: Connecting vulnerable individuals with positive role models.
- Reducing Social Isolation: Outreach to elderly, disabled, or marginalized populations.
- Reducing Access to Lethal Means:
- Firearm Safety: Promoting safe storage (locked, unloaded, separate from ammunition), gun locks, and education on temporary removal during crises.
- Medication Safety: Safe storage of prescription and over-the-counter medications, proper disposal of unused medications.
- Bridge Barriers/Cliff Fences: Physical barriers at common suicide sites.
- Poison Control: Restricting access to highly toxic substances.
- Enhancing Help-Seeking and Mental Health Services:
- Early Identification & Screening: Implementing suicide risk screening in healthcare settings (primary care, emergency rooms).
- Improved Access to Care: Increasing availability, affordability, and quality of mental health services.
- Telehealth Services: Expanding access to mental health care, especially in rural or underserved areas.
- Crisis Services: Promoting awareness and accessibility of crisis hotlines, text lines, and mobile crisis teams.
- Training Gatekeepers: Training individuals in positions to recognize and refer people at risk (e.g., teachers, clergy, police, bartenders, beauticians).
- Responsible Media Reporting and Messaging:
- Guidelines for Reporting: Encouraging media outlets to follow guidelines that avoid sensationalizing suicide, describe methods, or glorify individuals, which can lead to "suicide contagion."
- Focus on Hope and Help: Promoting messages that offer hope, encourage help-seeking, and provide resources (e.g., crisis hotline numbers).
- Stories of Recovery: Highlighting stories of individuals who have overcome suicidal thoughts and found recovery.
- Strengthening Economic Supports:
- Poverty Reduction: Programs that address economic hardship, such as job training, housing assistance, and financial counseling.
- Unemployment Benefits: Providing safety nets during periods of job loss.
- Teaching Coping and Problem-Solving Skills:
- School-Based Programs: Integrating mental health education and coping skills training into school curricula.
- Life Skills Training: Offering programs that teach stress management, conflict resolution, and emotional regulation.
- Addressing Underlying Mental Health Conditions:
- Universal Prevention: Public health campaigns to reduce stigma around mental illness and promote mental wellness for all.
- Selective Prevention: Targeting groups at higher risk (e.g., veterans, LGBTQ+ youth, indigenous communities) with tailored programs.
- Indicated Prevention: Intervening early with individuals showing initial signs of mental health issues.
Postvention refers to interventions conducted after a suicide has occurred, aimed at alleviating distress and preventing further suicides. It is a critical, often overlooked, aspect of suicide prevention.
- Support for Survivors of Suicide Loss (Bereaved by Suicide):
- Grief Support Groups: Providing safe spaces for individuals who have lost someone to suicide to share experiences and receive emotional support.
- Individual Counseling: Offering therapy specifically tailored to the complex grief often associated with suicide loss (guilt, shame, anger, trauma).
- Resources and Information: Connecting survivors with appropriate resources, including mental health services.
- Peer Support: Connecting newly bereaved individuals with those who have navigated similar experiences.
- Community Healing and Resilience:
- Crisis Response Teams: Mobilizing mental health professionals and support staff to schools or workplaces affected by a suicide to provide immediate counseling and support.
- Commemorative Activities: Facilitating healthy ways for communities to mourn and remember those lost, while avoiding glorification.
- Addressing Contagion: Proactively managing media attention and communication within the community to prevent a cluster of suicides.
- Reducing Stigma:
- Open Dialogue: Fostering open and honest conversations about suicide and mental health to reduce shame and isolation among survivors and those struggling.
- Education: Educating the public about the facts of suicide, common reactions to grief, and how to support those affected.
- Learning from Suicides:
- Suicide Review Boards: Analyzing circumstances surrounding suicides to identify patterns, systemic gaps, and opportunities for prevention. This can include "psychological autopsies" to understand the deceased's state of mind.
Suicide attempt is a psychiatric emergency and therefore collaborative interventions should be implemented.
Aims of management:
- To prevent self harm.
- To restore the patient’s functional state.
- To restore the patient's self esteem.
- Build Trust: Healthcare providers will try to build a positive relationship with the person who attempted suicide. This helps them cooperate and feel comfortable enough to accept help.
- Caution Card: The person will be kept under very close observation. This might involve a "caution card" or specific handover procedures to ensure continuous monitoring.
- Immediate Isolation (for safety): Admitted to a private room initially to create a secure environment while medical staff gather information and wait for the doctor.
- Remove All Dangers: A critical first step is to remove anything that could be used for harm – sharp objects, belts, glass, certain medications. The goal is to make the environment completely safe.
- Observations: Immediately, check vital signs (like heart rate, breathing), look for any physical injuries (like cuts, broken bones, or signs of poisoning). Life-threatening injuries are treated first. This means stopping serious bleeding, giving oxygen if they're struggling to breathe, doing a stomach pump/gastric lavage for ingested poisons, or immobilizing fractures.
- Observe Behavior: carefully watch for signs that the person is still thinking about suicide. This includes talking about ending their life, handling dangerous items, refusing food, gathering medications, giving away possessions, or unusual sleep patterns.
- Assessing Mental State: Assess the patient’s mental status by interviewing the patient, attendants or family member to identify any underlying mental illnesses (like severe depression, psychosis, etc.) that contributed to the attempt.
- Medication (When Appropriate):
- If there was poisoning, specific medications like Hydrocortisone 100mg to 200mg 3 times to 4 times might be given to help.
- For attempts linked to psychosis, Chlorpromazine 100mg nocte might be prescribed.
- If depression was a factor, Amitriptyline 75mg nocte could be used.
- If there are wounds, antibiotics like Cloxacillin will be given to prevent infection.
- Chemotherapy/drug therapy:
- Since depression is very common in people with suicidal tendencies, antidepressants (like Laroxyl 25mg-75mg ddd, Imipramine 25mg-75mg ddd) are often prescribed.
- For mood swings or bipolar disorder, mood stabilizers (like Carbamazepine, Lithium carbonate, Sodium valproate) might be used.
- Therapy and Other Treatments:
- ECT (Electroconvulsive Therapy): For very severe depression, especially if other treatments haven't worked or if there's an immediate, life-threatening risk, ECT might be recommended.
- Cognitive Therapy: This helps people change unhelpful thoughts and behaviors.
- Psychotherapy: This includes various types of talk therapy – group therapy, individual sessions, family therapy – all aimed at helping the person process their feelings, develop coping skills, and understand their situation better.
- Occupational Therapy: Engaging in activities or hobbies can help distract the mind and provide a sense of purpose.
- Encourage Expression: It's important to allow the person to express all their feelings, even anger, in a safe way.
- Focus on Strengths: Help them see their good qualities and achievements, rather than dwelling on perceived failures.
- Rehabilitation: If needed, help them learn new skills or regain old ones to build a more stable life.
- Engage in Activities: Provide distractions like games or simple activities to shift their focus away from suicidal thoughts.
- Nutritional Support: Offer appealing foods to encourage eating, as self-starvation can be a concern.
- Continuous Monitoring: Again, 24/7 close watch is crucial.
- Consistent Care: Limiting the number of different nurses caring for them can help build trust and continuity.
- Relaxation Techniques: Teach them ways to calm themselves when stressed.
- Family Involvement is Key:
- Advise family members to remove any potential means of harm from the home.
- Encourage family to be supportive and non-judgmental, helping the person adapt to a "suicide-free" life.
- Follow Treatment Plan: Emphasize the importance of taking all prescribed medications and attending therapy sessions.
- Follow-Up Appointments: Regular check-ups are essential.
- Report Side Effects: They should know to contact a healthcare provider if they experience any adverse effects from medication.
- Manage Stressors: Advise them to try and avoid or manage stressful situations that could trigger a relapse.
- Avoid Substances: Strongly advise against abusing drugs or alcohol, as these can severely impair judgment and increase risk.
- Family Support Continues: Reiterate the vital role of family in providing ongoing support.
- Community Integration: Encourage family and friends not to isolate the person, but rather to include them and foster a sense of belonging.


Requesting questions about the topic
https://nursesrevisionuganda.com/self-study-question-for-nurses-and-midwives/#MENTAL_HEALTH
Am too grateful for the work and notes
For sure I need questions about this topic
I like the way points r simplified
Thnx a lot I hv understood it
Some nursing diagnosis
To love and serve. Thank you for the work though I wish the points had some simple explanation. Otherwise the work is wow
Thanks for the well simplified note