Table of Contents
TogglePathological Effects Of Microorganisms
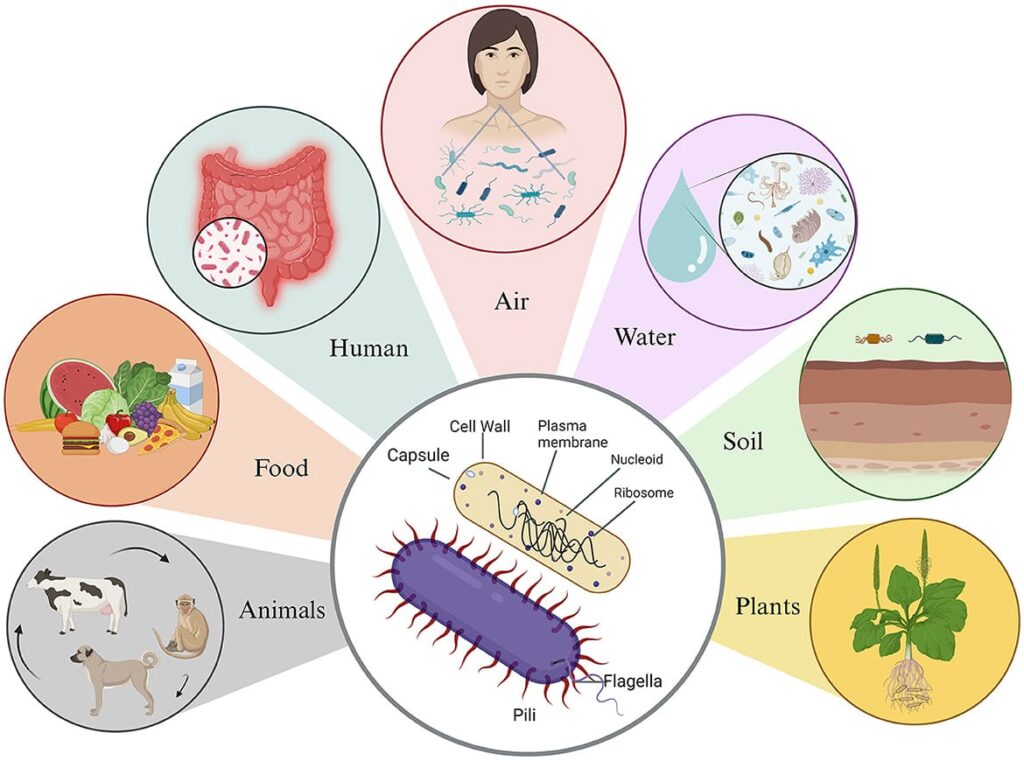
Microorganisms are a ubiquitous part of our world. While many are harmless or even beneficial (like our normal flora), a subset known as pathogens possess the ability to cause disease. The pathological effects of microorganisms refer to the full spectrum of harmful changes and damage they inflict on a host. This damage is a dynamic process involving direct cell injury, toxin-mediated damage, and often, collateral damage from the host's own immune response. The ultimate result is tissue injury, organ dysfunction, and systemic illness.
Mechanisms of Microbial Pathogenicity: How Microbes Cause Damage
Pathogenicity is an active process where pathogens use an arsenal of strategies, known as virulence factors, to successfully infect a host, evade its defenses, and cause disease.
A) Invasion and Colonization: Establishing a Foothold
- Respiratory Tract: Inhalation of airborne droplets (e.g., M. tuberculosis, Influenza virus, SARS-CoV-2).
- Gastrointestinal Tract: Ingestion of contaminated food or water (e.g., Salmonella, Vibrio cholerae, Giardia lamblia).
- Genitourinary Tract: Sexual contact or ascending infection from the urethra (e.g., Neisseria gonorrhoeae, Chlamydia trachomatis, E. coli).
- Skin and Parenteral Route: Through breaks in the skin (cuts, burns), insect bites, or direct injection via needles (e.g., Clostridium tetani from a wound, Plasmodium from a mosquito, HIV from a contaminated needle).
- Pili (Fimbriae): Hair-like appendages on bacteria like uropathogenic E. coli (UPEC) that bind specifically to cells lining the bladder, initiating a UTI.
- Glycocalyx (Capsule or Slime Layer): A sticky polysaccharide or polypeptide layer. Streptococcus mutans uses it to form tenacious biofilms on teeth (dental plaque), leading to caries.
- Hyaluronidase: The "spreading factor." Digests hyaluronic acid, the substance that holds cells together in connective tissue, allowing bacteria like Staphylococcus aureus to spread rapidly through tissue, causing cellulitis.
- Collagenase: Breaks down collagen, the primary protein of connective tissue. Produced by Clostridium perfringens to facilitate the devastatingly fast spread of gas gangrene through muscle.
- Kinases (e.g., Streptokinase): Digest fibrin clots. The body forms clots to wall off infections, but bacteria like Streptococcus pyogenes produce streptokinase to dissolve these clots and escape.
B) Toxin Production: Bacterial Chemical Warfare
Toxins are poisonous substances that are a primary cause of pathology in many diseases.
| Feature | Exotoxins | Endotoxins |
|---|---|---|
| Source | Secreted by living bacteria (mostly Gram-positive, some Gram-negative). | Part of the outer membrane of all Gram-negative bacteria. Released when the bacterium dies and lyses. |
| Composition | Proteins, often enzymes. | Lipid A portion of Lipopolysaccharide (LPS). |
| Potency & Specificity | Very high potency (fatal in tiny doses). Highly specific effects on target cells. | Lower potency (large amounts needed). Causes general, systemic effects. |
| Effect on Body | Causes specific signs and symptoms related to the toxin's function (e.g., paralysis, diarrhea, cell death). | Causes systemic inflammation: fever, chills, weakness, aches, and in high doses, septic shock and Disseminated Intravascular Coagulation (DIC). |
| Fever Production | Usually do not produce fever directly. | Potent pyrogens (fever-producers) by inducing cytokine release. |
| Example | Tetanus toxin, Botulinum toxin, Diphtheria toxin, Cholera toxin. | Lipid A from E. coli, Salmonella, Neisseria meningitidis. |
C) Evasion of the Host Immune System: The Art of Disguise and Defense
- Capsules: A slippery glycocalyx (e.g., on Streptococcus pneumoniae) physically prevents phagocytes from engulfing the bacterium. This is a major virulence factor.
- Leukocidins: Toxins produced by bacteria like Panton-Valentine leukocidin (PVL) from S. aureus that specifically target and kill white blood cells.
- All viruses are obligate intracellular parasites.
- Bacteria like Mycobacterium tuberculosis and Listeria monocytogenes are engulfed by macrophages but produce substances to prevent their digestion, turning the macrophage into a "safe house" for replication.
- Examples: Influenza virus (antigenic drift), Neisseria gonorrhoeae, and Trypanosoma brucei (causes sleeping sickness).
D) Immune-Mediated Damage
Often, the most severe and chronic damage is caused not directly by the microbe, but by the host's own over-zealous or misdirected immune response.
- Type II (Cytotoxic): Antibodies mistakenly bind to host cells, marking them for destruction. In Rheumatic Fever, antibodies against Streptococcus pyogenes cross-react with and damage heart valve tissue.
- Type III (Immune Complex): Clumps of antigen and antibody (immune complexes) get lodged in small blood vessels, triggering a destructive inflammatory cascade. In Post-streptococcal glomerulonephritis, these complexes damage the delicate filtering units (glomeruli) of the kidneys.
- Type IV (Delayed-Type): A T-cell mediated response. The classic example is the formation of a granuloma in tuberculosis. T-cells surround the infected macrophages, but the chronic inflammation slowly destroys healthy lung tissue, leading to cavitation.
Organ-System-Based Pathological Effects
A. Respiratory System
The pathogen invades the alveoli, is engulfed by macrophages, but survives inside. This triggers granuloma formation, leading to caseous necrosis and cavitary lesions. Pathological effects include chronic cough, hemoptysis, and weight loss.
- Streptococcus pneumoniae: Causes lobar pneumonia, filling alveolar spaces with fluid and pus (exudates), impairing gas exchange.
- Influenza Virus: Destroys ciliated respiratory epithelium, crippling the mucociliary escalator and increasing the risk of secondary bacterial infections.
Clinical Scenario: Acute Respiratory Distress Syndrome (ARDS)
A patient with severe influenza develops rapidly worsening shortness of breath and hypoxemia that doesn't improve with supplemental oxygen. A chest X-ray shows diffuse bilateral opacities ("white-out").
Pathological Process: This is an example of immune-mediated damage. The massive inflammatory response to the virus in the lungs (a "cytokine storm") causes the alveolar capillaries to become extremely leaky. The alveoli fill with protein-rich fluid, inactivating surfactant and collapsing the air sacs. This severe, non-cardiogenic pulmonary edema leads to catastrophic failure of gas exchange and high mortality.
B. Gastrointestinal System
Produces cholera toxin, which triggers excessive secretion of electrolytes and water, leading to profuse watery diarrhea and severe dehydration. The pathology is purely toxin-mediated with no tissue invasion.
- Salmonella typhi: Invades the intestinal lining, causing ulcers, then enters the bloodstream to cause systemic typhoid fever.
- Helicobacter pylori: Disrupts the gastric mucosa, causing gastritis and peptic ulcers.
- Clostridioides difficile: After antibiotics wipe out normal gut flora, this bacterium overgrows and produces toxins that cause severe inflammation and necrosis of the colon lining, forming a "pseudomembrane" (pseudomembranous colitis).
C. Nervous System
Produces tetanospasmin, a neurotoxin that inhibits inhibitory neurotransmitters, leading to spastic paralysis (muscle rigidity, lockjaw).
- Herpes simplex virus: Can cause encephalitis, leading to inflammation and necrosis of brain tissue.
- Poliovirus: Destroys motor neurons in the spinal cord, causing flaccid paralysis.
Clinical Scenario: Cryptococcal Meningitis
A patient with advanced HIV/AIDS presents with a persistent, worsening headache over several weeks, fever, and confusion. A lumbar puncture is performed.
Pathological Process: The fungus Cryptococcus neoformans is inhaled and spreads from the lungs to the brain. Its thick polysaccharide capsule helps it evade the weakened immune system. In the central nervous system, it causes a chronic inflammation of the meninges. Unlike acute bacterial meningitis, the onset is slow. The infection increases intracranial pressure, leading to the headache and neurological signs.
D. Cardiovascular System
Can cause infective endocarditis—an infection of the heart valves. This leads to the formation of vegetations (clumps of bacteria, platelets, and fibrin), causing valve destruction, embolism (when pieces break off and travel in the blood), and heart failure.
- Treponema pallidum (Syphilis): In its tertiary stage, can cause inflammation of the aorta (aortitis), weakening its wall and leading to aneurysm formation.
- Viral Myocarditis: A direct attack on the heart muscle (myocardium) by viruses like Coxsackie B, leading to inflammation, heart muscle weakness, and potentially life-threatening arrhythmias.
F. Genitourinary System
Adheres to mucosal cells in the urethra, causing inflammation and purulent discharge (urethritis). In females, it can ascend to the upper reproductive tract.
- Escherichia coli: The major cause of UTIs, leading to painful urination (dysuria) and potentially ascending to the kidneys to cause pyelonephritis.
- Schistosoma haematobium: A parasitic fluke whose eggs become lodged in the bladder wall, causing chronic inflammation that is linked to fibrosis, urinary problems, and a high risk of bladder cancer.