Table of Contents
TogglePERICARDITIS
Pericarditis is an inflammation of the pericardium.
Pericarditis is usually acute – it develops suddenly and may last up to several months.
Sometimes excess fluid develops in the space between the pericardial layers and causes a pericardial effusion
The Pericardium
The pericardium is a thin, two-layered, fluid-filled sac that covers the outer surface of the heart.(normal volume of the fluid is around 50ml)
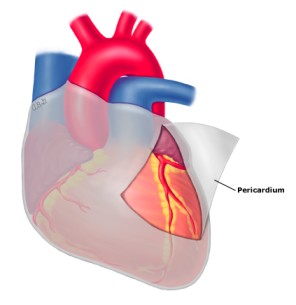
- It also prevents the heart from over-expanding when blood volume increases, which keeps the heart functioning efficiently.
- It shields the heart from infection or malignancy and contains the heart in the chest wall.
Causes of Pericarditis
- Infection
A) Viral infection: this is the most important cause in infection, coxsackie A virus and B commonest one, B3 , B5 are the most common, influenza Virus. hepatitis Virus.
B) Bacterial infection – :
- Tubercle bacilli
- Staphylococcus
- Streptococcus
- Pneumococcus
C)Fungal infection:
- Histoplasma
- Candida Species
- Infections such as toxoplasmosis
D) Metabolic disorders:
- Uraemia. (most important). Presents with pericadial effusion and especially after introduction of renal dialysis. The pericardial effusion enhanced after renal dialysis .
E) Connective tissue disorders e.g. systemic lupus erythematosus
- Chest trauma / injury
- Lung disease (Tuberculosis),
- HIV (Human Immunodeficiency Virus).
- Side effects some medication such as Isoniazid,Tetracycline
- Malignancy,
- Scleroderma
- Radiation Induced,
- Chest trauma / injury
- HIV (Human Immunodeficiency Virus).
- Side effects some medication such as Isoniazid,Tetracycline
- Malignancy,
- Scleroderma
- Radiation Induced,
- Lung disease (Tuberculosis),
- Myxedema,
- Acute MI,
- Dissection of Aortic Aneurysm,
- Ankylosing spondylitis,
- Inflammatory bowel disease,
- Rheumatic fever,
- Cancer (including leukemia).
Pathophysiology of Pericarditis
- The acute inflammatory response in pericardium can produce either serous or purulent fluid, or a dense fibrinous material. In viral pericarditis, the pericardial fluid is most commonly serous, is of low volume, and resolves spontaneously.
- Neoplastic, tuberculous, and purulent pericarditis may be associated with large effusions that are exudative, hemorrhagic, and leukocyte filled.
- Gradual accumulation of large fluid volumes in the pericardium, even up to 250 mL, may not result in significant clinical signs.
Signs and Symptoms of Pericarditis
- Beck’s triad is a collection of three medical signs associated with acute cardiac tamponade.
The signs are:-
- Low arterial blood pressure
- Distended neck veins
- Distant, muffled heart sounds.
Chest pain symptoms associated with pericarditis can be described as:
- Sharp and stabbing chest pain (caused by the heart rubbing against the pericardium). May increase with coughing, deep breathing or lying flat.
- Can be relieved by sitting up and leaning forward .
- You may also feel the need to bend over or hold your chest to breathe more comfortably.
Other clinical features include;
- Pain in the back, neck or left shoulder
- A dry cough
- Anxiety or fatigue
- Difficulty breathing when lying down
- Swelling of the feet, legs or ankles.
- This swelling may be a symptom of constrictive pericarditis, a serious type of pericarditis.
- In constrictive pericarditis, the patient’s pericardium hardens and/or thickens, preventing the heart muscle from expanding and affecting the function of the heart.
- Fever
- Tachycardia
- The heart may be compressed by the constrictive process, which may cause blood to back up into the lungs, abdomen and legs, as well as cause the swelling.
- Palpitations
- Weakness
- Irritability
- Fatigue
- Loss of appetite
- Irregular heart beat
- Anxiety and fatigue,
- Cyanosis,
- Cough,
- Hoarseness, voice weakness or complete aphonia,
- Dysphagia,
- Distended neck veins,
- Abdominal or leg swelling for long term pericarditis.
Diagnosis of Pericarditis
- Medical history and physical examination – history and physical assessment will identify presence of risk factors and signs and symptoms. On assessment, the physician may listen to heart sound and may hear pericardial rub which is the sound made by the pericardial layers from rubbing each other.
- Laboratory tests – lab tests including a series of blood and urine tests may help identify the possible cause of pericarditis.
- Electrocardiogram (ECG) – The tracing of the heart is often done to identify any effect on the heart functions.
- Chest X – ray – this imaging can easily give the physician the information related to the size and shape of the heart and clues to the presence of fluid build-up.
- Echocardiogram – this procedure involves viewing the pumping ability of the heart through ultrasound.
- CT scan of the chest – this imaging can give more details on the shape and size of the heart. It can identify the presence of restrictive pericarditis and can help rule out other heart conditions.
- MRI scan of the chest – another form of imaging can be performed if the other forms of imaging are inconclusive.
Management and Treatment of Pericarditis
Treatment options for pericarditis rely on the cause of the disease. However, some cases may not need any treatment and may resolve on its own.
- Medication Therapy. Some drugs are used to help manage the symptoms of pericarditis.
- Analgesics – pain killers are often given to cope with the pain associated with pericarditis.
- Anti-gout medication – a certain anti-gout medication can also be used for pain management.
- Corticosteroids – steroids combat inflammation. Corticosteroids are often given in pericarditis to settle the inflammation of the pericardium.
- Pericardiocentesis. This procedure involves the insertion of a needle into the pericardial sac to aspirate the fluid build-up. It is completed with the use of an ultrasound machine.
- Pericardiectomy. Pericardiectomy is a surgical procedure that involves the removal of the pericardium. It is typically done in cases of constrictive pericarditis.
Nursing Interventions
- Monitor patient pain level and evaluate pain within 30 minutes.
- Administer prescribed pain medication such as morphine to relieve pain.
- Monitor the patient pain level and effectiveness of analgesics.
- Provide a comfortable position (sit up and lean forward).
- Check vital sign and record it continuously.
- Discuss disease process and signs and symptoms expanding aneurysm or impending aneurysm.
- If surgical intervention needed, provide psychological support and prepare for surgery.
- For post surgical patients, discuss about warning sign of postoperative complication such as fever, inflammation in surgical site, bleeding and swelling.
- Daily check of weight.
- Closely monitor and notify to physician about persistent cough, vomiting or systolic blood pressure above 180mmhg because of the increased risk for hemorrhage.
- Ensure bed rest until fever, chest pain and friction rub disappear
- Administer O2 and keep SPO2 ˃90%.
- Administer medication as order-such as NSAIDs and steroids with food.
- Ensure administer of antibiotic timely.
- Continue I.V antihypertensive medication if persistent blood pressure high.
- Carefully maintain fluid intake and output.
- Reassure patient that chest pain is not a Myocardial Infarction.
- Check sign and symptoms for cardiac tamponade at least 8 hourly and PRN.
- Assist the patient with bathing if necessary.
- Tell the patient to resume his daily activities slowly.
- Build a rapport relationship with patient to reduce anxiety.
- Surgery: open surgical drainage is usually the treatment of choice for cardiac tamponade.
Nursing Diagnosis
- Hyperthermia related to the disease process of bacterial pericarditis evidenced by temperature of 38.0 degrees Celsius, rapid breathing, profuse sweating, and chills
- Alteration in comfort related to chest pain due to pericardial inflammation as evidenced by facial grimacing.
- Decreased cardiac output related to pericarditis as evidenced by fatigue and inability to do Activities of Daily Living as normal.
- Alteration in comfort related to chest pain due to pericardial inflammation as evidenced by clutching of hands or chest.
- Acute Pain related to inflammatory process of bacterial pericarditis evidenced by chest pain score of 10 out of 10, guarding sign, and shortness of breath
- Altered tissue perfusion related to tissue ischemia as evidenced by abnormal hemodynamic readings.
- Activity intolerance related to acute chest pain as evidenced by fatigue, disinterest in activities of daily living due to pain, verbalization of tiredness and generalized weakness
- Anxiety related to threat to body image as evidenced decreased energy, irritability, crying, feelings of helplessness
Complications of Pericarditis
- Constrictive Pericarditis: Constrictive pericarditis is a severe form of chronic pericarditis in which the inflamed layers of the pericardium stiffen, develop scar tissue, thicken and stick together.
- Pericardial Effusion: Rapid fluid accumulation in the pericardium can cause cardiac tamponade, a severe compression of the heart that impairs its ability to function.
- Cardiac tamponade: Compression of the heart caused by fluid collecting in the sac surrounding the heart.
- Pericardial effusion: Pericardial effusion is a buildup of fluid in the space around the heart.
- Myocardial ischemia: Myocardial ischemia occurs when blood flow to your heart is reduced, preventing the heart muscle from receiving enough oxygen.
- Stroke: A stroke, sometimes called a brain attack, occurs when something blocks blood supply to part of the brain, in this case, something blocking the heart also blocks blood supply to the brain.


Is it reduced cardiac output related to pericarditis as evidenced by fatigue and in ability to do activities of daily living as normal.
Or it should have been reduced body activity related to pericarditis evidenced by fatigue and inability to do daily living activities as normal??
In that’ part of nursing diagnosis 🙏
Is reduced body activity an allowed Nursing Diagnosis?, No, Check Nanda for more clarity
Altered bod temperature in relation to pericarditis evidence by high thermometer reading of 39
Thanks, however, instead of “In relation”, opt for “Related to” and also, relate it to the CAUSE, not the condition, such as “Related to disturbance of the thermoregulatory centers on the brain” and also add Degrees on 39.
Good notes, well summarized
𝐓𝐡𝐚𝐧𝐤𝐬
I need more clarity on pathophysiology
Weldone please
Nursing diagnosis needs more clearance, I guess. But overall note is good.