Table of Contents
ToggleASTHMA
Asthma is a chronic reversible inflammatory disease of the airways characterized by an obstruction of airflow.
- Inflammation causes recurrent typical characteristics of recurrent episodes of wheezing(occurs during expiration), breathlessness, chest tightness, and coughing, which respond to treatment with bronchodilators.
- Many inflammatory mediators play a role; mast cells, eosinophils, T-lymphocytes, macrophages, neutrophils, and epithelial cells.
- No precise cause but genetic and triggers are associations
Classification of Asthma
Asthma can be divided into;
(a)Intrinsic asthma– when no causative agent can be identified.
(b)Extrinsic or cryptogenic asthma– implying a definite external cause.
Levels of Asthma
These guidelines were established by the National Institutes of Health so that physicians and pediatricians can determine the extent of your child’s asthma.
1. Intermittent asthma
Asthma is considered intermittent if without treatment any of the following are true:
- Symptoms (difficulty breathing, wheezing, chest tightness, and coughing):
- Occur on fewer than 2 days a week.
- Do not interfere with normal activities.
- Nighttime symptoms occur on fewer than 2 days a month.
2. Mild persistent asthma
Asthma is considered mild persistent if without treatment any of the following are true:
- Symptoms occur on more than 2 days a week but do not occur every day.
- Attacks interfere with daily activities.
- Nighttime symptoms occur more than twice a month.
3. Moderate persistent asthma
Asthma is considered moderate persistent if without treatment any of the following are true:
- Symptoms occur daily. Inhaled short-acting asthma medication is used every day.
- Symptoms interfere with daily activities.
- Nighttime symptoms occur more than 1 time a week, but do not happen every day
4. Severe persistent asthma
Asthma is considered severe persistent if without treatment any of the following are true:
Symptoms:
- Occur throughout each day.
- Severely limit daily physical activities.
- Nighttime symptoms occur often, sometimes every night
Etiology/Risk Factors.
Multiple environmental factors and genetic determinants are implicated in the development of asthma.
These include;
- Endogenous factors
(a) Genetic predisposition; There is familial association of asthma and a high degree of occurrence of asthma in identical twins
(b) Atopy: A form of allergy in which there is a hereditary tendency to develop hypersensitivity reactions like; Hay fever/allergic rhinitis & atopic eczema /dermatitis & asthma. Atopy is due to the genetically determined production of specific IgE antibody, with many patients showing a family history of allergic diseases
2. Infection and Diseases
(a) Upper Respiratory Tract viral infections
- Rhinitis and Sinusitis
- Postnasal drip
- Respiratory syncytial virus infection in infancy
- Drugs like;
- Beta 2 blockers cause bronchoconstriction
- ACEI like Captopril
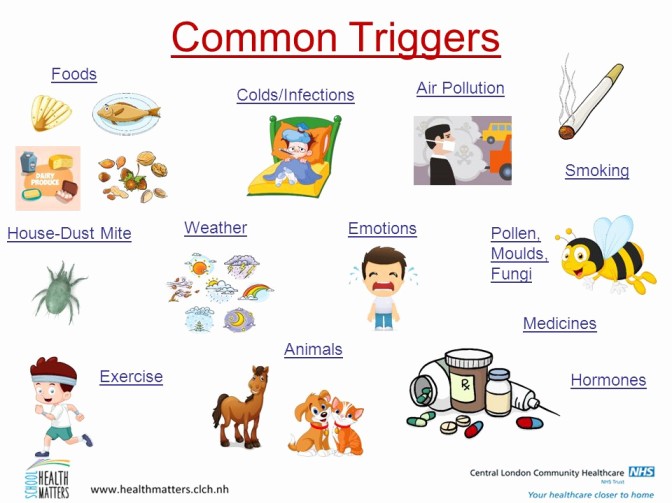
4. Environmental Factors.
(a) Air Pollution
- Air pollutants, such as sulfur dioxide, nitrogen dioxide, diesel particulates
- Indoor air pollution; Leads to exposure to nitrogen oxides from cooking stoves and exposure to passive cigarette smoke
(b) Allergens;
- Indoor allergens like cats ,cockroaches house, dust mites often found in pillows, mattresses, furniture, carpets and drapes
- Outdoor allergens like pollen grains , animal fur
- All these inhaled allergens are common triggers of asthma
Food: e.g. Nuts, chocolate, milk.
(c) Occupational Exposure;
- Occupational asthma is relatively common
- Over 200 sensitizing agents have been identified
- Some chemicals, fungal amylase in wheat flour bakers
(d) Changes in the weather
(e) Irritants like household sprays, paint fumes
(i) Others may include;
- Strong emotions: e.g. fear, laughing.
- Exercise or hyperventilation,
- Temperature and weather changes.

Pathophysiology of Asthma
Summary
The pathophysiology in asthma is reversible and airway inflammation leads to airway narrowing.
- Trigger Factor. When a person is exposed to a trigger, it causes airway inflammation and mast cells are activated.
- Activation. When the mast cells are activated, it releases several chemicals called mediators. These chemicals perpetuate the inflammatory response, causing increased blood flow, vasoconstriction, hypersecretion of mucus, the attraction of white blood cells to the area, airway muscle constriction and bronchoconstriction.
- Narrow Breathing Passages. Acute bronchoconstriction due to allergens results from a release of mediators from mast cells that directly contract the airway.
- Asthma features: As asthma becomes more persistent, the inflammation progresses and other factors may be involved in the airflow limitation, Signs include wheezing, cough, dyspnea, chest tightness. etc.
- Exposure to a stimulus –Release of substances from immune cells: mast cells, eosinophils, basophils, neutrophils, and macrophages.
- The initial step: T-cell activation. Lymphokines are produced which amplify the immune response, notably by the production of IgE antibodies and their induction of allergic reactions.
- Early-phase reaction: Release of IgE and the activation of cells bearing allergen specific IgE receptors, particularly airway mast cells.
- The activated cells produce proinflammatory mediators such as histamine, eicosanoids, and reactive oxygen species (ROS).
- Some of these substances, such as histamine, adenosine, bradykinin, and major basic protein, are stored in cells as granules.
- Other substances are formed and immediately released in response to asthmatic stimuli, including lipid mediators derived from arachidonic acid, such as leukotrienes and prostaglandins.
- Proinflammatory mediators induce contraction of airway smooth muscle, mucus secretion, and vasodilation.
- Airflow obstruction is caused by inflammatory mediators that induce microvascular leakage and exudation of plasma into the airways.
- Plasma protein leakage induces a thickened, engorged, and edematous airway wall and a narrowing of the airway lumen.
- The late-phase reaction occurs 6 to 9 hours after the early-phase reaction and is characterized by recruitment and activation of eosinophils, CD4+ cells, basophils, neutrophils, and macrophages. Adhesive interactions occur among the various cell types.
- T cells are recruited 24 hours after the early-phase reaction and are thought to play a role in the chronic phase of the response and the enhancement of non-specific bronchial hyper-responsiveness.
- All of these substances contribute to inflammation of the airway,
edema and desquamation of the bronchial epithelium, and
hypertrophy of smooth muscles in the respiratory tract.
• These chemical mediators also increase the responsiveness of
smooth muscles and the permeability of bronchioles to
allergens, infectious agents, mediators of inflammation, and
other irritants.
• As a result of these effects, mucus production increases and leads to mucus plugging of the airways, thereby decreasing the ability of the airways to remove noxious substances.
• As a result, patients develop airway obstruction and must use
accessory muscles to breathe. - Airway obstruction in asthma results from a combination of
bronchial inflammation, smooth muscle constriction, and obstruction of the lumen with mucus, inflammatory cells, and epithelial debris. - Symptoms of obstruction include dyspnea (difficult breathing), coughing, wheezing, headache, tachycardia, syncope, diaphoresis, pallor, and cyanosis
Clinical Manifestations
Principal symptoms
- Wheezing attacks
- Episodic shortness of breath
Typical symptoms
- Wheezing
- Chest tightness
- Breathlessness
- Non-productive cough
Signs
- Diaphoresis
- Tachycardia
- Widened pulse pressure
- Hypoxemia
- Central cyanosis
- Tachypnoea (RR> 25BPM)
- Cyanosis
- Feeble respiratory effort
- Bradycardia or arrhythmias
- Hypotension
- Exhaustion
- Confusion
- Coma
Acute severe asthma
- Respiratory rate ≥ 25/min
- Heart rate ≥ 110/min
- Inability to complete sentences in 1 breath
Diagnosis and Investigations
To determine the diagnosis of asthma, the clinician must determine that episodic symptoms of airway obstruction are present.
- Positive family history. Asthma is a hereditary disease, and can be possibly acquired by any member of the family who has asthma within their clan.
Physical Examination: Auscultation, Wheezing allover the lung, Breathlessness, Cyanosis
Diagnostic techniques Chest x-ray ,Blood and sputum tests, Skin tests, CBC

Management of Asthma
Aims
- Achieve and maintain control of symptoms
- Prevent asthma exacerbations
- Maintain pulmonary function as close to the normal as possible (Homeostasis)
- Avoid adverse effects from asthma medications
- Prevent development of irreversible airflow limitation
- Prevent asthma mortality
- Restore normal or best possible lung function
- Reduce the risk of severe attacks
- Enable normal growth to occur in children
- Minimize absence from school
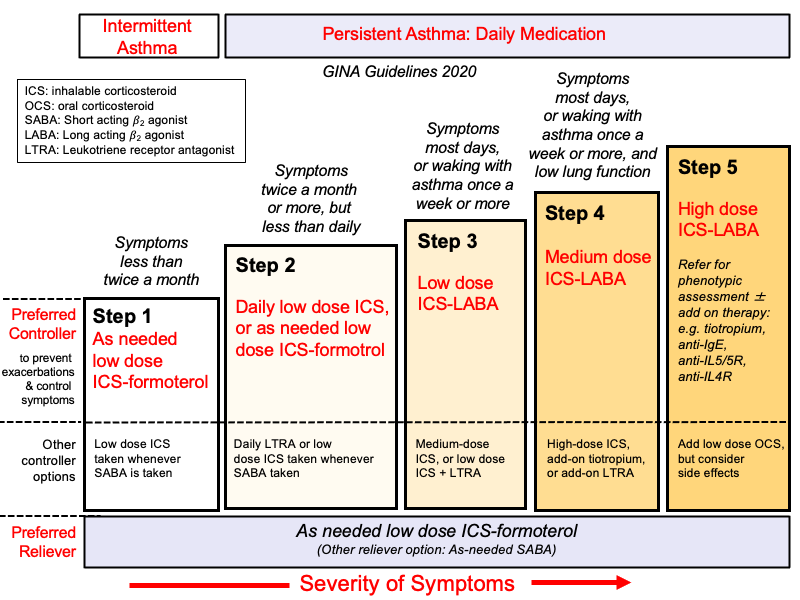
Step Ladder Management.
- Step 1: Occasional use of inhaled short-acting β2-adrenoreceptor agonist bronchodilators
- Step 2: Introduction of regular preventer therapy preferably inhaled corticosteroids-ICS
- Step 3: Add-on therapy Long-acting β2-agonists (LABAs), such as salmeterol and formoterol.
- Step 4: Poor control with step 3: addition of a fourth drug eg leukotriene receptor antagonists, theophyllines
- Step 5: Continuous or frequent use of oral steroids
- Reassure the patient
- Keep patient in upright position
- Oxygen 50-60%
Peak Flow Monitoring
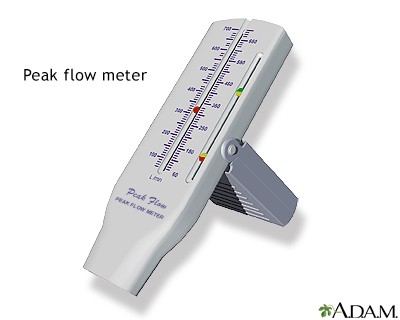
- Peak flow meters. Peak flow meters measure the highest airflow during a forced expiration.
- Daily peak flow monitoring. This is recommended for patients who meet one or more of the following criteria: have moderate or severe persistent asthma, have poor perception of changes in airflow or worsening symptoms, have unexplained response to environmental or occupational exposures, or at the discretion of the clinician or patient.
- Function. If peak flow monitoring is used, it helps measure asthma severity and, when added to symptom monitoring, indicates the current degree of asthma control.
Pharmacological management
Quick response medicines
- Bronchodilators
- Short acting inhaled beta 2 agonists
- Salbutamol (albuterol), Terbutaline, Levalbuterol, Pirbuterol
- Anticholinergics (Ipratropium 500mcg)
- Corticosteroids (Hydrocortisone)
Long term medicines
- Anti-inflammatory drugs
- Montelclust/levocetirizine
- Corticosteroids
- Bronchodilators
- Long acting beta 2 agonists
- Salmeterol, Formoterol
- Theophylline 5-7mg/kg
Nursing Care after an Acute Attack
- Give high flow oxygen to patient to relieve hypoxemia.
- Prepare and give the patient a bed in a propped up position to help improve breathing patterns
- Start up an IV access for IV drugs
- Give IV fluids if the patient is dehydrated and encourage oral fluid intake by patient.
- Prepare a fluid balance chart if patient is on IV fluids
- Take all patient vitals to monitor response to treatment
- Give emergency treatment like nebulized salbutamol or IV aminophylline /hydrocortisone to relieve Difficult in Breathing
- Administer all prescribed drugs for the patient and monitor for any Side and effects of drugs
NURSING DIAGNOSIS
- Impaired breathing patterns related to severe inflammatory process in the lungs evidenced by wheezing
- Impaired tissue oxygenation related to inflammatory process in airway passages evidenced by cyanosis
- Extreme anxiety related to the frequent life threatening asthmatic attacks evidenced by patient asking many questions
- Ineffective airway clearance related to increased production of mucus and bronchospasm evidenced by wheezing and dyspnea
- Impaired gas exchange related to altered delivery of inspired Oxygen.
Complications of Asthma.
- Airway infection like bronchiolitis
- Cor pulmonale; Rheumatic Heart Failure secondary to chronic chest disease
- Pneumonia
- Hypoxic respiratory failure in severe disease
- Atelectasis
- Pneumonia
- Status asthmaticus
- Pneumothorax /Air-leak syndromes (rare)
- Death


Am exhausted, thnx
How so dear 🤣😂😂
Thanks
Excellent notes