Addison’s Disease (Adrenal Insufficiency)
Addison’s disease, also known as primary adrenal insufficiency, is a rare disorder characterized by the insufficient production of hormones by the adrenal glands.
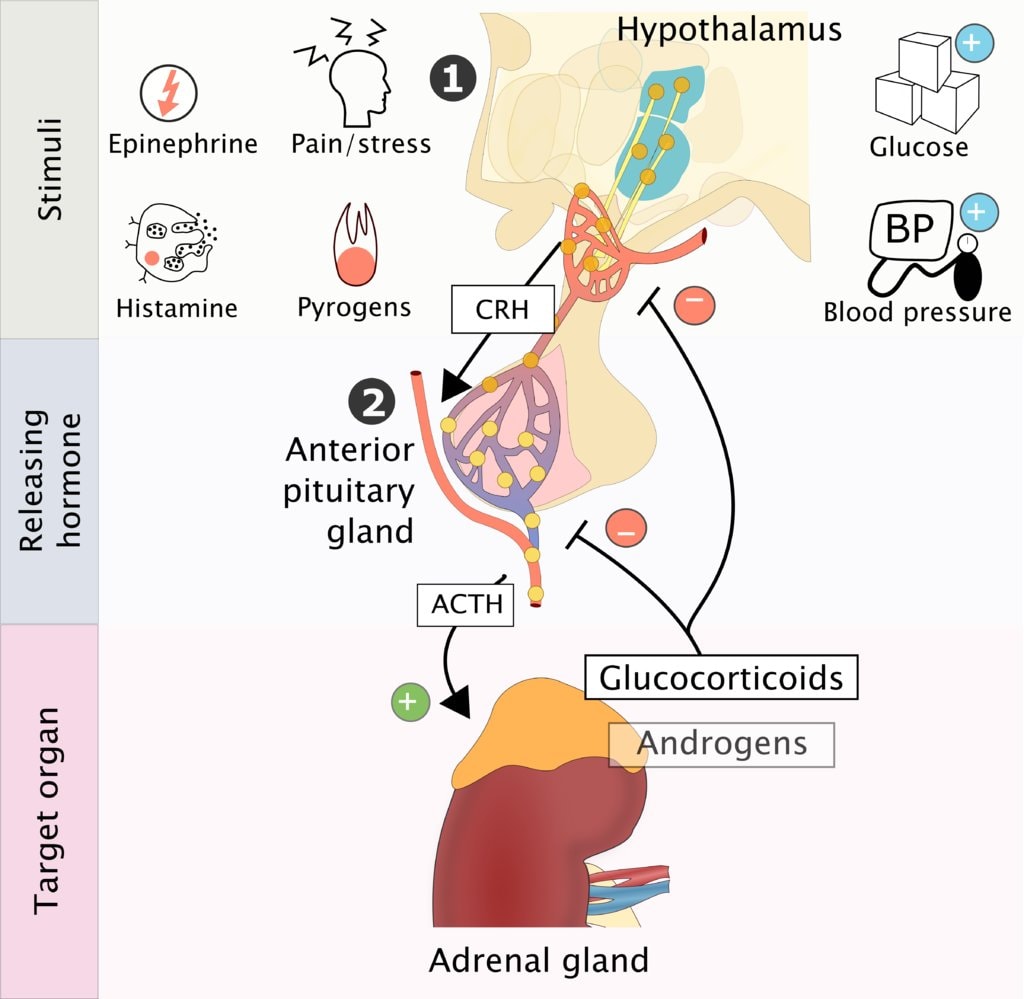
Addison’s disease is a clinical condition characterized by adrenocorticotrophic hormone hyposecretion due to primary disease of the adrenal glands or secondary to pituitary gland disorder.
The adrenal glands, located above the kidneys, produce hormones such as cortisol and aldosterone that are essential for maintaining normal bodily functions.
It’s mostly idiopathic or auto immune but can occur in tuberculosis infection of the gland or obstruction by the adrenal tumor, metastasis / hemorrhage
Hormones Produced by the Adrenal Cortex
|
Hormone |
Examples of the Hormone |
Effects of the Hormone |
|
Glucocorticoids |
Cortisol, Cortisone, Hydrocortisone |
– Protein Breakdown: Enhances the breakdown of proteins, especially in muscle cells, to release amino acids. – Glucose Formation: Promotes gluconeogenesis, converting non-carbohydrate sources into glucose, raising blood sugar levels. – Lipolysis: Stimulates the breakdown of stored fats into fatty acids and glycerol. – Resistance to Stress: Increases blood pressure and blood glucose, providing the body with energy to handle stress. – Anti-inflammatory Effects: Inhibits white blood cells that participate in inflammatory responses, reducing inflammation and allergic reactions. – Depression of Immune Responses: Lowers the activity of the immune system, which can decrease the body’s ability to fight infections. |
|
Mineralocorticoids |
Aldosterone |
– Electrolyte Balance: Regulates sodium (Na⁺) and potassium (K⁺) ions, maintaining blood pressure and fluid balance. – Blood Pressure Regulation: Adjusts blood pressure and blood volume by increasing sodium retention and water reabsorption in the kidneys. – Acid-Base Balance: Promotes the excretion of hydrogen ions (H⁺) in the urine, preventing acidosis and helping to maintain blood pH. |
|
Androgens |
Dehydroepiandrosterone (DHEA), Androstenedione |
– Secondary Sexual Characteristics: Influence the development of male secondary sexual characteristics, such as facial hair and deepening of the voice. – Sex Drive: Contribute to libido in both males and females. – Precursor for Estrogen: In postmenopausal women, androgens serve as precursors for estrogen synthesis. |
Hormone | Cells that Produce It | Action of the Hormone |
Adrenaline (Epinephrine) | Chromaffin Cells | – Fight or Flight Response: Increases heart rate, blood pressure, and blood glucose levels; dilates airways to prepare the body for stress. – Energy Mobilization: Stimulates the breakdown of glycogen to glucose in the liver, providing quick energy. – Increased Alertness: Enhances alertness and readiness by stimulating the central nervous system. |
Noradrenaline (Norepinephrine) | Chromaffin Cells | – Fight or Flight Response: Similar to adrenaline, it constricts blood vessels to increase blood pressure and redirects blood flow to vital organs. – Vasoconstriction: Causes blood vessels to constrict, which increases peripheral resistance and helps maintain blood pressure during stress. |
Pathophysiology of Adrenal Insufficiency
Adrenal glands are incapable of producing sufficient cortisol and other steroids . It is distinguished from acute primary adrenocortical insufficiency caused by Waterhouse-Friderichsen syndrome.
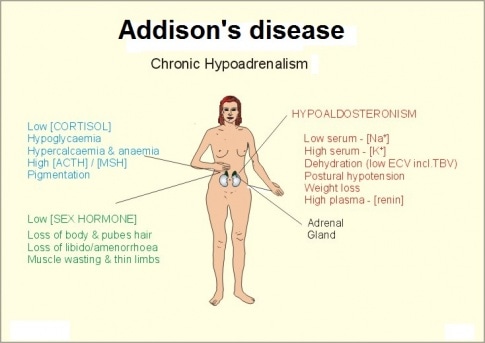
Mineralocorticoid deficiency: Because mineralocorticoids stimulate sodium reabsorption and potassium excretion, deficiency results in increased excretion of sodium and decreased excretion of potassium, chiefly in urine but also in sweat, saliva, and the gastrointestinal tract. A low serum concentration of sodium (hyponatremia) and a high concentration of potassium (hyperkalemia) result.
Urinary salt and water loss cause severe dehydration, plasma hypertonicity, acidosis, decreased circulatory volume, hypotension, and, eventually, circulatory collapse. However, when adrenal insufficiency is caused by inadequate adrenocorticotropic hormone (ACTH) production (secondary adrenal insufficiency), electrolyte levels are often normal or only mildly deranged, and the circulatory problems are less severe.
Glucocorticoid deficiency: Glucocorticoid deficiency contributes to hypotension and causes severe insulin sensitivity and disturbances in carbohydrate, fat, and protein metabolism. In the absence of cortisol, insufficient carbohydrate is formed from protein; hypoglycemia and decreased liver glycogen result. Weakness follows, due in part to deficient neuromuscular function. Resistance to infection, trauma, and other stress is decreased. Myocardial weakness and dehydration reduce cardiac output, and circulatory failure can occur.
Decreased blood cortisol results in increased pituitary ACTH production and increased blood beta-lipotropin, which has melanocyte-stimulating activity and, together with ACTH, causes the hyperpigmentation of skin and mucous membranes characteristic of Addison disease. Thus, adrenal insufficiency secondary to pituitary failure does not cause hyperpigmentation.

Causes of Addison’s Disease(Can be predisposing Factors too)
- Autoimmune Reaction: Addison’s Disease can occur when the body’s immune system mistakenly attacks and damages the adrenal glands. This is known as an autoimmune reaction. In this case, the immune system views the adrenal glands as foreign entities and targets them for destruction, leading to a deficiency in adrenal hormones.
- Idiopathic Atrophy of the Adrenal Glands: In some cases, the adrenal glands may undergo atrophy, which means they shrink and lose their function without a clear identifiable cause. This condition is referred to as idiopathic adrenal atrophy.
- Surgical Removal of Both Adrenal Glands: Addison’s Disease can result from the surgical removal of both adrenal glands. This usually occurs as a last resort when treating conditions such as Cushing’s syndrome or adrenal tumors. After removal, the individual will need hormone replacement therapy.
- Adrenal Carcinoma: Adrenal carcinoma is a rare type of cancer that originates in the adrenal glands. In some instances, the cancerous growth can disrupt the normal functioning of the adrenal glands, leading to adrenal insufficiency and Addison’s Disease.
- Infections such as TB: Certain infections, particularly tuberculosis (TB), can infiltrate and damage the adrenal glands. TB-induced damage to the adrenal glands can impair their ability to produce hormones, causing Addison’s Disease.
- Abnormal/Malfunction of the Pituitary Gland: The pituitary gland plays a crucial role in regulating adrenal function by secreting adrenocorticotropic hormone (ACTH). If the pituitary gland malfunctions and doesn’t produce an adequate amount of ACTH, the adrenal glands won’t receive the necessary signals to produce hormones, leading to Addison’s Disease.
- Prolonged Use of Steroid Medication: Long-term use of corticosteroid medications, which are often prescribed for conditions like autoimmune diseases or inflammation, can suppress the production of ACTH by the pituitary gland. This can lead to adrenal gland atrophy and result in Addison’s Disease.
Additional causes include:
- Genetic Factors: While most cases of Addison’s Disease are not inherited, there is a rare genetic form known as familial glucocorticoid deficiency (FGD). In FGD, specific genetic mutations can lead to the inadequate production of adrenal hormones.
- Hemorrhage into the Adrenal Glands: Severe bleeding into the adrenal glands, often due to injury or other medical conditions, can damage the glands and impair their hormone production.
- Amyloidosis: Amyloidosis is a rare condition in which abnormal proteins (amyloids) build up in various organs, including the adrenal glands. This accumulation can disrupt adrenal function and cause Addison’s Disease.

Clinical Presentation of Addison’s Disease:
Due to Cortisol Deficiency: Addison’s Disease primarily results in the deficiency of cortisol, which is a crucial hormone for various bodily functions.
Common symptoms due to cortisol deficiency include:
- Weakness: Individuals with Addison’s Disease often experience significant weakness, making even simple tasks challenging.
- Weight Loss: Unexplained weight loss can occur due to a disruption in metabolism.
- Fatigue: Profound fatigue and tiredness are typical, even after a full night’s sleep.
- Nausea and Vomiting: Persistent nausea and vomiting may be present.
- Diarrhea: Chronic diarrhea can develop as a result of gastrointestinal disturbances.
Due to Increased ACTH Production (If the Cause Is in the Adrenal Gland): When Addison’s Disease is caused by issues within the adrenal glands, it can lead to increased production of adrenocorticotropic hormone (ACTH).
Symptoms related to excess ACTH include:
- Hyperpigmentation of Skin and Mucous Membranes: A distinctive symptom is the darkening of the skin and mucous membranes, which may appear as tan or bronze patches. This is often referred to as hyperpigmentation.
Due to Mineralocorticoid Deficiency: Addison’s Disease can also lead to the deficiency of mineralocorticoids, particularly aldosterone, which plays a crucial role in regulating electrolyte balance.
Symptoms associated with mineralocorticoid deficiency include:
- Very Low Blood Pressure (Hypotension): The absence of aldosterone can result in extremely low blood pressure, leading to dizziness and fainting.
- Serum Potassium High, but Sodium and Chloride Are Low: Electrolyte imbalances can manifest as high levels of potassium and low levels of sodium and chloride.
Due to Androgen Deficiency: In some cases, Addison’s Disease may also cause androgen deficiency, which can lead to specific symptoms:
- Sparse Hair in Females: Women with Addison’s Disease may experience hair thinning or loss.
- General Weakness: Overexertion, exposure to cold, or acute infections can exacerbate the overall weakness and fatigue experienced by individuals with Addison’s Disease.
Other symptoms: Dizziness, headache, and menstrual irregularities in women may also occur.
In severe cases, adrenal crisis can occur, which is a life-threatening condition characterized by
- extremely low blood pressure, electrolyte imbalances, and shock.
CLASSIC TRIAD/CARDINAL SIGNS Hyperpigmentation: A darkening of the skin, MOSTLY in areas exposed to the sun and areas of friction or pressure. The hyperpigmentation is a result of increased production of melanin due to elevated levels of adrenocorticotropic hormone (ACTH). Weakness and Fatigue: Individuals with Addison’s disease often experience generalized weakness and fatigue. This is attributed to the deficiency of glucocorticoids, such as cortisol, which play a crucial role in maintaining energy balance. Low Blood Pressure (Hypotension): Addison’s disease can lead to decreased production of aldosterone, contributing to low blood volume and hypotension (low blood pressure). Electrolyte imbalances, particularly low sodium levels, also play a role in hypotension. |
DIAGNOSTIC EVALUATION
History collection
- History of recent infection, steroid use, or adrenal or pituitary surgery.
- History of poor tolerance for stress, weakness, fatigue, and activity intolerance.
- Anorexia, nausea, vomiting, or diarrhea as a result of altered metabolism.
- Dizziness due to orthostatic hypotension.
- History of craving for salt or intolerance to cold.
- Presence of altered menses in females and impotence in males.
Physical examination
- Signs of dehydration such as tachycardia, altered level of consciousness, dry skin with poor turgor, dry mucous membranes, weight loss, and weak peripheral pulses.
- Postural hypotension
- Inspect the skin for pigmentation changes
- Inspect the patient’s gums and oral mucous membranes to see if they are bluish-black.
- Temperature
- Any loss of axillary and pubic hair that could be caused by decreased androgen levels.
Investigations
1. ACTH stimulation test
- Short test: compares blood cortisol levels before and after 250 mcg of tetracosactide (IM/IV) is given.
- Increased ACTH level: Primary insufficiency
- Decreased ACTH level: Secondary insufficiency
2. Other investigations
- Complete blood count (CBC): Anaemia
- Blood urea nitrogen (BUN): Increased
- Electrocardiography (ECG): Shows low voltage and peaked T waves caused by hyperkalaemia
- Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI): To assess the adrenal glands
- Urine cortisol and aldosterone: Decreased
- Hypoglycaemia, hyponatremia, hyperkalaemia, leukocytosis.
Complications of Addison’s Disease:
Renal Failure:
- One of the potential complications of Addison’s Disease is renal failure, which refers to the loss of kidney function.
- Addison’s Disease can disrupt the balance of electrolytes in the body, particularly causing increased levels of potassium. This imbalance can have a detrimental effect on the kidneys.
- High levels of potassium can lead to abnormal heart rhythms (arrhythmias) and, in severe cases, impair kidney function.
Adrenal Hemorrhage:
- Adrenal hemorrhage, though rare, is another complication that can occur in individuals with Addison’s Disease.
- It involves bleeding into the adrenal glands, typically due to an adrenal crisis or severe stress. This can lead to sudden and severe abdominal or back pain.
- Adrenal hemorrhage requires immediate medical attention, as it can be life-threatening.
Addisonian Crisis:
- An Addisonian crisis, also known as an adrenal crisis, is a severe and potentially life-threatening complication of Addison’s Disease.
- It occurs when the adrenal glands fail to produce enough cortisol to meet the body’s needs, often triggered by stress, illness, trauma, or abrupt cessation of corticosteroid medications.
- Symptoms of an Addisonian crisis can include extreme weakness, confusion, low blood pressure, rapid heart rate, and even loss of consciousness.
- Prompt emergency medical treatment is essential to stabilize the patient, typically through intravenous administration of cortisol and fluids.
Depression:
- Chronic illnesses like Addison’s Disease can lead to emotional and psychological challenges, including depression.
- Coping with the demands of managing a chronic condition, along with the physical symptoms and potential complications, can take a toll on a person’s mental health.
- It’s essential for individuals with Addison’s Disease to receive comprehensive care that includes addressing emotional well-being and providing support for mental health issues such as depression.
Management of Addison’s Disease
The management of Addison’s disease involves lifelong hormone replacement therapy to compensate for the deficiency of cortisol and aldosterone. Treatment aims to:
Replace missing hormones:
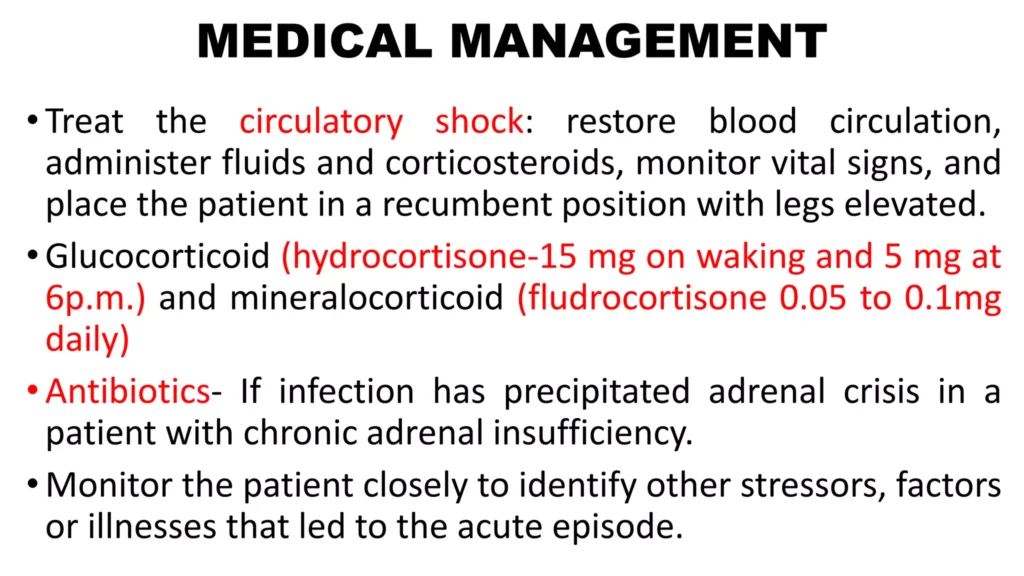
- Glucocorticoids: Hydrocortisone is the most commonly used glucocorticoid, administered in divided doses throughout the day to mimic the body’s natural cortisol production. (hydrocortisone-15 mg on waking and 5 mg at 6p.m.)
- Mineralocorticoids: Fludrocortisone is the primary mineralocorticoid used to replace aldosterone. (fludrocortisone 0.05 to 0.1mg daily).
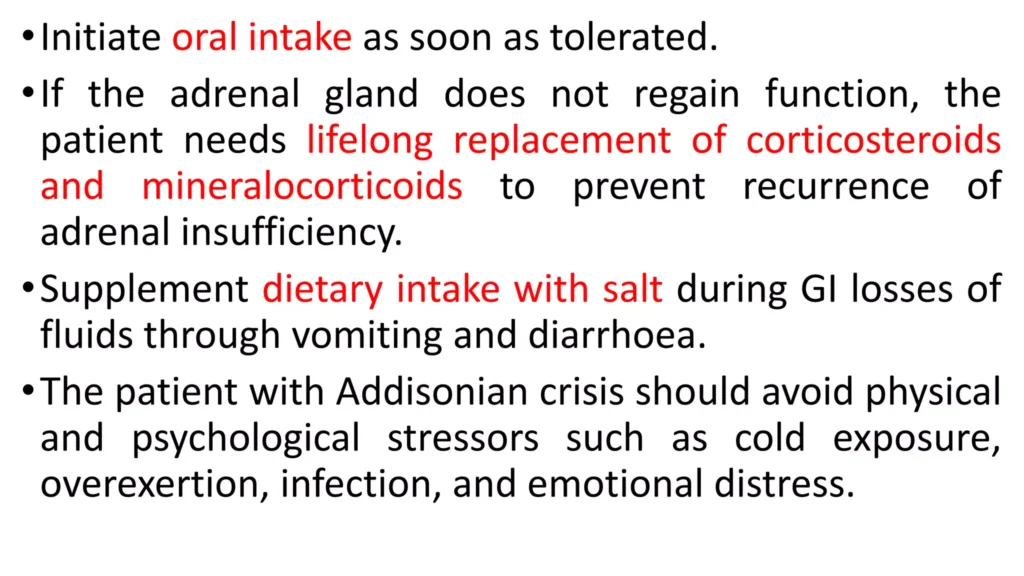
- If the adrenal gland does not regain function, the patient needs lifelong replacement of corticosteroids and mineralocorticoids to prevent recurrence of adrenal insufficiency.
Manage complications:
- Addisonian crisis: A life-threatening emergency caused by severe adrenal insufficiency. It requires immediate medical attention with intravenous fluids, electrolyte replacement, and high doses of hydrocortisone.
Treatment of patient with Addisonian crisis
- Administration of fluid, glucose, and electrolytes, especially sodium.
- Replacement of missing steroid hormones; and vasopressors(Vasopressors are drugs used to raise blood pressure in people whose blood pressure is very low.)
- Large volumes of 0.9% saline solution and 5% dextrose are administered to reverse hypotension and electrolyte imbalances until blood pressure returns to normal.
Electrolyte imbalances: Regular monitoring of electrolytes (sodium, potassium) and prompt correction of imbalances are crucial.
Osteoporosis: Glucocorticoid therapy can increase the risk of osteoporosis. Calcium and vitamin D supplementation, along with weight-bearing exercises, are recommended.
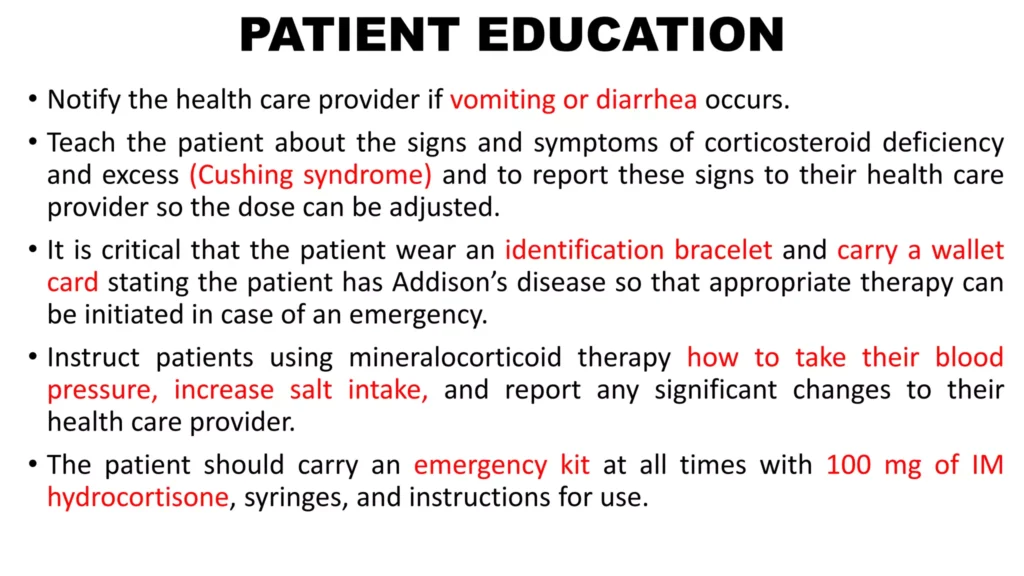
Patient education:
- Self-management: Patients need to learn about their condition, medication regimen, and how to recognize and manage symptoms.
- Emergency preparedness: Patients should carry an emergency kit containing injectable hydrocortisone and a medical identification card.
- Stress management: Patients should avoid excessive stress and learn techniques to manage stress effectively.
- Dietary modifications: A balanced diet with adequate salt intake is essential.
- Supplement dietary intake with salt during GI losses of fluids through vomiting and diarrhoea.
- Regular follow-up: Regular visits with a healthcare provider are necessary to monitor the patient’s condition and adjust medication doses as needed.
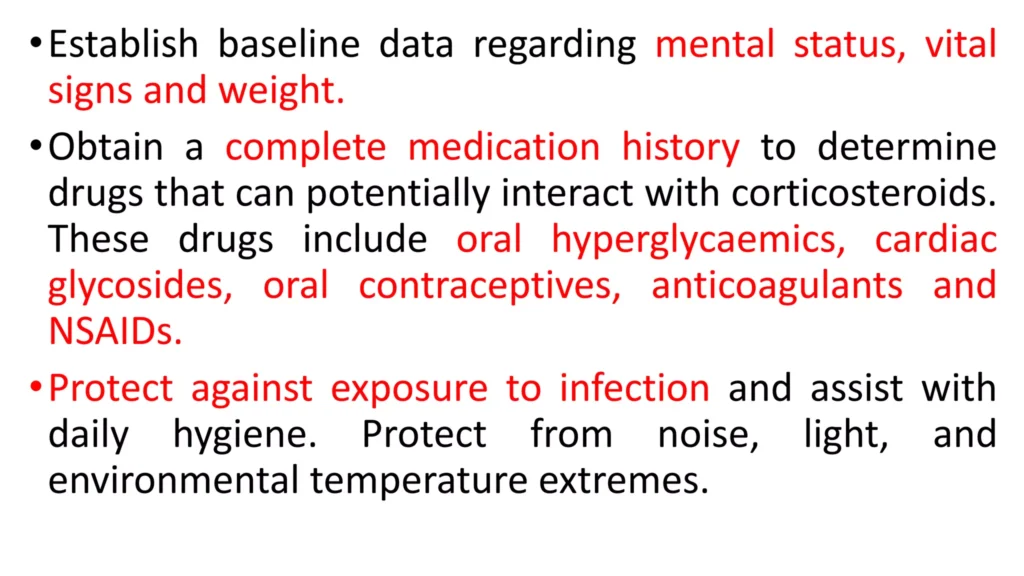
Nursing Interventions.
- Hormone Replacement Therapy: Collaborate with the healthcare team to ensure the patient receives appropriate hormone replacement therapy, with glucocorticoids (such as hydrocortisone) and mineralocorticoids (such as fludrocortisone). Administer medications as prescribed and monitor for the desired therapeutic response.
- Medication Education: Provide education to the patient and their family regarding the importance of adhering to the prescribed medication regimen. Explain the purpose, dosage, timing, and potential side effects of hormone replacement medications.
- Stress Management: Educate the patient about the need for increased medication during times of physical or emotional stress, such as illness, injury, or surgery. Instruct them to carry an emergency card or wear a medical alert bracelet to inform others about their condition.
- Fluid and Electrolyte Balance: Monitor the patient’s fluid intake and output and assess for signs of dehydration or electrolyte imbalances. Encourage the patient to maintain adequate hydration and offer oral rehydration solutions as needed.
- Blood Pressure Monitoring: Regularly measure the patient’s blood pressure to assess for hypotension. Collaborate with the healthcare team to adjust medication dosages if necessary to maintain appropriate blood pressure levels.
- Dietary Education: Provide dietary education to the patient, emphasizing the importance of a well-balanced diet with adequate sodium intake. Encourage the patient to include foods rich in sodium in their diet or consult with a dietitian for personalized guidance.
- Emotional Support: Provide emotional support and encourage open communication with the patient. Offer a safe space for them to express any concerns, fears, or emotional challenges related to their condition.
- Education on Recognizing and Managing Emergencies: Educate the patient and their family about the signs and symptoms of adrenal crisis, a life-threatening condition that can occur in Addison’s disease. Instruct them to seek immediate medical help if symptoms such as severe weakness, dizziness, abdominal pain, or altered consciousness occur. Increase dosage in times of stress.
- Collaboration and Referrals: Collaborate with the healthcare team to ensure comprehensive care for the patient. This may involve referrals to specialists such as endocrinologists or social workers who can provide additional support and resources.
Nursing Concerns in Addison’s Disease:
Hypotension and Fluid Balance:
- Concern for the patient’s risk of hypotension and dehydration.
- Monitoring blood pressure and fluid status, implementing interventions to address imbalances.
Electrolyte Imbalances:
- Concern for potential electrolyte imbalances, such as hyponatremia and hyperkalemia.
- Regular monitoring of electrolyte levels and interventions to maintain balance.
Adrenal Crisis Risk:
- Concern for the risk of adrenal crisis during stress or illness.
- Patient education on stress dosing and vigilant monitoring during times of increased stress.
Medication Adherence:
- Concern for adherence to medication regimens.
- Assessing the patient’s understanding of the importance of medication compliance.
Skin Integrity:
- Concern for skin changes and hyperpigmentation.
- Regular skin assessments and education on skin care to prevent breakdown.

Medical Management
- Restore blood circulation IV fluids NS and Dextrose.
- Small dose of fludrocortisones 0.05 – 0.1mg/day is given to maintain BP and electrolytes
- Hormone replacement with cortisone daily in divided doses i.e prednisolone 20mg in the morning and 10mg in the evening
- Vasopressor amines may be required if hypertension persists.
- Antibiotic therapy if infection has precipitated the adrenal crisis
- Lifelong replacement of corticosteroids and mineralocorticoids.
- ORS for salt replacement.
- May need additional salt intake
- Treat underlying cause ie TB
Nursing Care
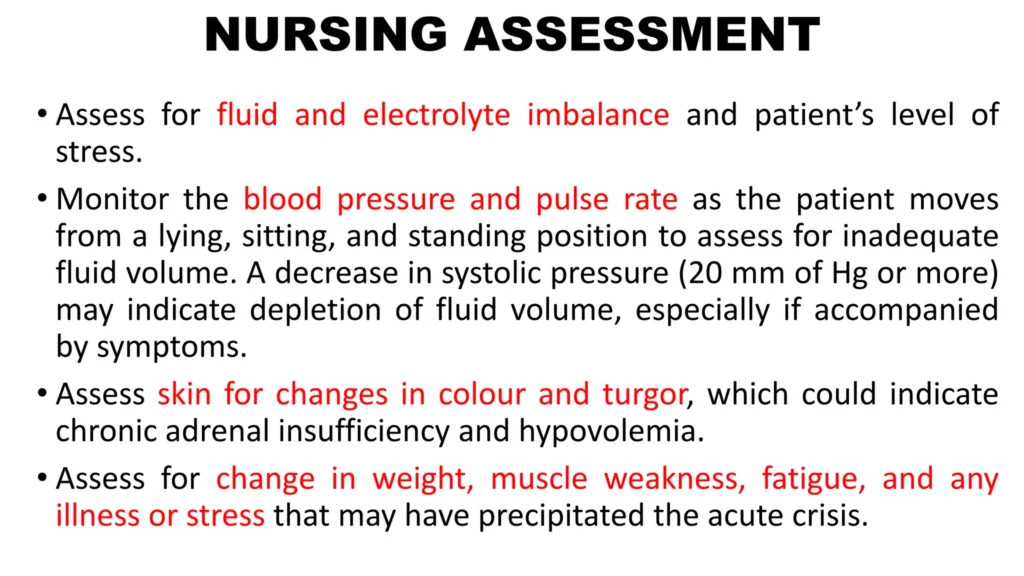
- Monitor for BP,P, as patient moves from lying, sitting, and standing position to asses for inadequate fluid volume.
- Assess skin color and turgor
- Assess history of weight changes, muscle weakness, and fatigue.
- Ask patient and family about onset of illness or increased stress that may have precipitated the crisis
Nursing diagnosis
- Electrolyte imbalance related to low sodium level as evidenced by craving for salt, vomiting and diarrhea.
- Ineffective tissue perfusion related to hyperpigmentation of skin as evidenced by skin tanning.
- Risk for fluid volume deficit related to vomiting and diarrhea.
.

Nursing care plan for Addison’s disease:
Assessment | Nursing Diagnosis | Goals/Expected Outcomes | Interventions | Rationale | Evaluation |
1. Patient reports fatigue, muscle weakness, and dizziness. | Activity Intolerance related to fatigue and muscle weakness as evidenced by the patient reporting the inability to perform daily activities without exhaustion. | The patient will demonstrate increased energy levels and participate in daily activities with minimal fatigue. | – Encourage rest periods between activities to conserve energy. – Assist with activities of daily living (ADLs) as needed. – Educate the patient on the importance of balancing activity and rest. | Rest periods prevent exhaustion and allow for energy conservation. Assistance with ADLs reduces the physical strain on the patient. Education promotes effective energy management. | The patient reports increased energy and is able to participate in daily activities with minimal fatigue. |
2. Patient presents with hypotension, darkened skin, and weight loss. | Deficient Fluid Volume related to adrenal insufficiency as evidenced by hypotension, weight loss, and decreased skin turgor. | The patient will maintain adequate fluid volume as evidenced by stable blood pressure and normal skin turgor. | – Monitor vital signs, especially blood pressure, regularly. – Administer prescribed corticosteroid therapy (e.g., hydrocortisone). – Encourage increased oral fluid intake, and administer IV fluids as needed. – Educate the patient on recognizing signs of dehydration and the importance of fluid intake. | Monitoring vital signs detects changes in fluid status. Corticosteroid therapy helps manage adrenal insufficiency. Increased fluid intake and IV fluids help maintain fluid balance. Education empowers the patient to prevent dehydration. | The patient maintains stable blood pressure and demonstrates normal skin turgor. |
3. Patient expresses concern about skin changes and weight loss. | Disturbed Body Image related to hyperpigmentation and weight loss as evidenced by the patient verbalizing distress about appearance. | The patient will verbalize acceptance of their appearance and demonstrate positive body image behaviors. | – Provide emotional support and counseling to address concerns about appearance. – Encourage participation in self-care and grooming activities. – Refer to a support group or counselor specializing in chronic illness. | Emotional support helps the patient cope with changes in appearance. Self-care activities can enhance self-esteem. Support groups provide a network for shared experiences and coping strategies. | The patient reports acceptance of their appearance and demonstrates positive body image behaviors. |
4. Patient reports nausea, vomiting, and decreased appetite. | Imbalanced Nutrition: Less than Body Requirements related to nausea and vomiting as evidenced by weight loss and decreased appetite. | The patient will maintain adequate nutritional intake and demonstrate stable weight. | – Monitor daily weight and nutritional intake. – Offer small, frequent meals with high-calorie, nutrient-dense foods. – Administer antiemetics as prescribed to control nausea. – Collaborate with a dietitian to develop a nutrition plan that meets the patient’s needs. | Monitoring weight and intake helps assess nutritional status. Small, frequent meals are easier to tolerate and help maintain calorie intake. Antiemetics reduce nausea and improve appetite. A dietitian can tailor a nutrition plan to the patient’s needs. | The patient maintains stable weight and reports improved appetite. |
5. Patient reports feelings of anxiety about managing the disease and its symptoms. | Anxiety related to chronic illness and potential complications as evidenced by patient verbalizing concerns about managing Addison’s disease. | The patient will verbalize reduced anxiety and demonstrate effective coping strategies. | – Assess the patient’s understanding of Addison’s disease and its management. – Provide education on the disease, including symptom management and when to seek medical help. – Teach stress management techniques, such as deep breathing exercises and relaxation techniques. – Refer the patient to a counselor or support group if needed. | Understanding the disease reduces fear and anxiety. Education empowers the patient to manage their condition effectively. Stress management techniques help reduce anxiety levels. Counseling or support groups provide additional emotional support. | The patient reports reduced anxiety and effectively manages the disease with appropriate coping strategies. |
6. Patient presents with a blood glucose level of 60 mg/dL, sweating, and confusion. | Risk for Hypoglycemia related to impaired gluconeogenesis and decreased cortisol levels. | The patient will maintain blood glucose levels within the normal range. | – Monitor blood glucose levels regularly. – Educate the patient on recognizing early signs of hypoglycemia, such as sweating, shaking, and confusion. – Administer glucose or dextrose as prescribed in case of hypoglycemia. – Encourage the patient to carry fast-acting carbohydrates (e.g., glucose tablets) at all times. | Regular monitoring detects hypoglycemia early. Early recognition allows for prompt intervention. Glucose administration rapidly corrects hypoglycemia. Carrying fast-acting carbohydrates ensures the patient can quickly address hypoglycemia. |

Amazing work
perfect notes with nice details.
thank you