Table of Contents
ToggleBursitis
Bursitis is inflammation of a bursa, a small fluid-filled sac that acts as a cushion between bone and muscle, skin or tendon.
Bursitis can also be defined as a painful medical condition characterized by inflammation of the bursae found in large joints.
Bursae are fluid-filled sacs that act as a cushion between bones, tendons, joints, and muscles. When these sacs become inflamed it is called bursitis.
There are over 150 bursae in the human body. They cushion and lubricate points between the bones, tendons, and muscles near the joints.
The bursae are lined with synovial cells. Synovial cells produce a lubricant that reduces friction between tissues. This cushioning and lubrication allows our joints to move easily.
Causes of Bursitis
Bursitis often results from sport injuries or repetitive movements. But it can also be caused by:
- Autoimmune disorders
- Crystal deposition (gout and pseudo gout)
- Infectious diseases
- Traumatic events
- Hemorrhagic disorders
- Being secondary to overuse. Overuse and repetitive injuries to the joint, abnormal bony structure can cause bursitis.
- Stress on soft tissues from an abnormal or poorly positioned joint or bone
- Some types of arthritis and related conditions (rheumatoid arthritis, osteoarthritis or gout.)
- Metabolic conditions such as diabetes.
- Septic bursitis can be caused by bacterial infection of the bursa through skin injury following repetitive trauma.
Pathophysiology of Bursitis
Repetitive injury within the bursa results in local vasodilatation and increased vascular permeability, which stimulate the inflammatory cascade. One study suggests that this process may be mediated by cytokines, metalloproteases, and cyclooxygenases.
Trauma or infection leads to inflammation of the bursa which causes synovial cells to multiply and thereby increases collagen formation and fluid production. A more permeable capillary membrane allows entrance of high protein fluid. The bursal lining may be replaced by granulation tissue followed by fibrous tissue. The bursa becomes filled with fluid, which is often rich in fibrin, and the fluid can become hemorrhagic.
Types of Bursitis, with Signs and Symptoms
(a) According to duration.
- Acute Bursitis: (0months to 3months) During the acute phase of bursitis, local inflammation occurs and the synovial fluid is thickened, and movement becomes painful as a result.
- Chronic Bursitis: (3months and above): leads to continual pain and can cause weakening of overlying ligaments and tendons and, ultimately, rupture of the tendons. Because of the possible adverse effects of chronic bursitis on overlying structures, bursitis and tendinitis may occur together.
(b) According to presence of infection.
- Septic Bursitis: Septic (or infectious) bursitis occurs when infection from either direct inoculation (usually superficial bursa) or hematogenous or direct spread from other sites (deep bursa involvement) causes inflammatory bursitis. Septic bursitis can be acute, subacute, or recurrent/chronic. Fluid may present with , White blood cell count (WBC) greater than 100,000/µL with a predominance of neutrophils, High protein and lactate, Positive culture and Gram stain.
- Aseptic Bursitis. A non-infectious condition caused by inflammation resulting from local soft-tissue trauma or strain injury. Fluid may present with White blood cell count (WBC) range from 2000 to 100,000/µl, Negative culture and Gram stain.
(c) According to Anatomy/Affected body part.
1. Subacromial bursitis.
Subacromial bursitis is a common etiology of shoulder pain. It results from inflammation of the bursa, a sac of tissue present under the acromion process of the shoulder. It is usually brought about by repetitive overhead activities or trauma.

- Mid-shoulder pain early in the course of bursitis, which gradually increases over time; eventually pain may be felt even at rest
- Pain after repetitive activity such as painting, throwing a ball, or playing tennis
- Pain worsens at night
- Popping sensation with shoulder movements.
2. Olecranon bursitis
The olecranon bursa is synovial membrane located immediately posterior to the olecranon bone of the elbow. The bursa’s function is to allow the bony olecranon to glide smoothly across the overlying tissues with flexion and extension of the elbow.

- Painful or painless focal swelling at the posterior elbow
3. Trochanteric bursitis
Trochanteric bursitis is inflammation (swelling) of the bursa at the outside (lateral) point of the hip known as the greater trochanter. When this bursa becomes irritated or inflamed, it causes pain in the hip. This is a common cause of hip pain.
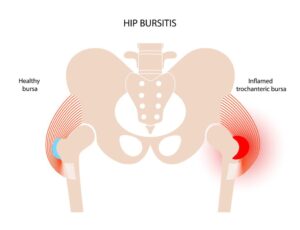
- Pain in the lateral side of the hip with walking, running, or stair-climbing
- Weakness of the lower extremities
- Pain with active and passive motion.
4. Prepatellar bursitis
Prepatellar bursitis is an inflammation of the bursa in the front of the kneecap (patella). It occurs when the bursa becomes irritated and produces too much fluid, which causes it to swell and put pressure on the adjacent parts of the knee.

- Reduced range of motion at the knee
- Focal swelling, pain, and redness
- Difficulty kneeling and walking.
5. Retrocalcaneal bursitis
Retrocalcaneal bursitis (also known as ankle bursitis or Achilles tendon bursitis) is a condition in which the retrocalcaneal bursa, a small cushioning sac between the heel bone and the Achilles tendon, becomes inflamed.

- Swelling at the back of heel
- Pain at the back of the heel, especially when running uphill
- Pain while standing on tiptoes
Diagnosis and Investigations.
- History and symptoms.
- Physical examination.
- Lab tests. There are no diagnostic lab findings associated with bursitis. However, patients with septic bursitis may present with elevated ESR, CRP, and white blood cells.
- X-ray. X ray may be used as a diagnostic measure to support a clinical diagnosis of bursitis. Joint x ray is generally reserved for patients with history of significant trauma. A plain x ray may be helpful in the diagnosis of fracture or dislocation
- CT Scan. It is usually reserved for the patients who do not respond to initial treatment. On CT scan, superficial bursitis may be characterized by fluid density at the subcutaneous tissue. Additionally, a CT scan will detect any foreign bodies.
- Ultrasound Scan. Useful in confirming the diagnosis of bursitis. On ultrasound, bursitis may be characterized by bursal wall distention with the presence of local hypoechoic or anechoic intra-bursal material, synovial proliferation, calcifications, and rheumatoid nodules.
Management and Treatment of Bursitis
Aims
- To reduce the inflammation and pain.
- To identify and treat the cause.
- To prevent complications.
Nursing Management
- Most patients with bursitis are treated conservatively to reduce inflammation.
- Conservative treatment involves control of pain and inflammation, which may be guided by the PRICEMM acronym, as follows:
- P rotect – Use padding, braces, or changes in technique
- R est – Avoid activities that exacerbate pain
- I ce – Cryotherapy can relieve pain and decrease inflammation
- C ompression – Elastic dressings can ease pain, as in olecranon bursitis
- E levation – Raise the affected limb above the level of the heart
- M odalities – Employ electrical stimulation, ultrasonography, or phonophoresis
- M edications – Administer nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or corticosteroid injections, bursal aspiration, and intra-bursal steroid injections (with or without local anesthetic agents).
- Patients who have bursitis secondary to overuse should be educated about the importance of regular periods of rest and possible alternative activities to prevent recurrence.
- Applying cold treatments for 20 minutes every several hours may be of value in the first 24-48 hours. Such treatments may be followed by heat treatments.
- Elevation is useful, particularly in lower-limb bursitis. Consider site-specific therapy (eg, cushions for ischial bursitis, well-fitting padded shoes for calcaneal bursitis).
- Patients with suspected septic bursitis should be treated with antibiotics while awaiting culture results. Superficial septic bursitis can be treated with oral outpatient therapy.
- Those with systemic symptoms or who are immunocompromised may require admission for intravenous (IV) antibiotic therapy.
- Surgical excision of bursae may be required for chronic or frequently recurrent bursitis however Surgery is reserved as a last resort for patients in whom conservative treatment fails.
Medical Management.
Medical management for bursitis depends on the involved bursa.
Septic
- Systemic antibiotics
- Staphylococcus aureus, bursitis often resolves with antibiotics alone
- Sporothrix schenckii bursitis often requires bursectomy
- Most patients respond to oral antibiotics alone, although some require intravenous therapy
Antimicrobial Regimens
Standard antimicrobial regimens for septic bursitis are as follows:
1. Staphylococcus aureus, methicillin-susceptible (MSSA)
- Oxacillin 2g IV q.i.d
- Dicloxacillin 500 mg PO q.i.d

2. Staphylococcus aureus, methicillin-resistant (MRSA)
- Vancomycin 1g IV b.d
Aseptic
- Usually managed with PRICEMM regimen
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Local corticosteroid injections may be used in some patients who do not respond to initial therapy
Subacromial Bursitis
Conservative measures that are recommended among all patients who develop subacromial bursitis include:
Physical therapy (PT)
- Scapular strengthening and postural reeducation
- Shoulder exercise
- Nonsteroidal anti-inflammatory medications (NSAIDs)
Prepatellar Bursitis
Conservative measures that are recommended among all patients who develop prepatellar bursitis include:
- Nonsteroidal anti-inflammatory medications (NSAIDs) is often used as a first choice
- Reduce physical activity
- PRICEMM regimen in the first 72 hours after the injury
- Physical therapy
- Local corticosteroid injections may be used in some patients who do not respond to initial therapy
Olecranon Bursitis
Conservative measures that are recommended among all patients who develop olecranon bursitis include:
- PRICEMM regimen in the first 72 hours after the injury.
- Avoidance of aggravating physical activity
- Most patients improve significantly with these measures, so physical and occupational therapy are not usually necessary
- Early aspiration (with or without corticosteroid injection) may be helpful among patients with bothersome fluid collections
- Diagnostic aspiration should be performed among patients who do not respond to treatment in order to rule out possible infection
Trochanteric Bursitis
Conservative measures that are recommended among all patients who develop trochanteric bursitis include:
- Modification of physical activity
- Weight loss
- Physical therapy
- Nonsteroidal anti-inflammatory medications (NSAIDs)
- Local glucocorticoid injections are reserved for patients with refractory symptoms
Physical therapy and NSAIDs are the most effective therapies for trochanteric bursitis. Most patients do not require any surgical intervention.
Retrocalcaneal Bursitis
Conservative measures that are recommended among all patients who develop retrocalcaneal bursitis include:
- PRICEMM regimen in the first 72 hours after the injury.
- Maneuvers that stretch the Achilles tendon may be helpful
- Limitation of activity and modification of footwear to avoid posterior heel irritation
- Nonsteroidal anti-inflammatory medications (NSAIDs)
- Physical therapy
Corticosteroid injections are not recommended as they may have adverse effects on the Achilles tendon.
Surgical Management
Bursectomy
Surgical intervention is not usually recommended for the management of bursitis. Bursectomy is generally reserved for patients with chronic, recurrent, or septic bursitis.
Indications for surgical intervention (open incision/endoscopic bursectomy) in patients with bursitis include:
- Inability to drain the infected bursa effectively with needle aspiration
- Presence of a foreign body in superficial bursa
- Adjacent skin or soft tissue infection requiring debridement
- Critically ill patients who are immunocompromised
- Chronically infected and thickened bursa
- Severe refractory and recurrent bursitis
Prevention of Bursitis.
- Regular exercise
- Doing warm-ups or stretches before physical activity
- Maintaining a healthy weight
- Strengthening muscles around the joint
- Taking breaks from repetitive tasks
- Using foam for kneeling or elbow pads
- Refraining from sitting still for long periods of time
- Practicing good posture and positioning the body properly when going about daily activities
Complications of Bursitis.
- Chronic pain: Untreated bursitis can lead to a permanent thickening or enlargement of the bursa, which can cause chronic inflammation and pain.
- Muscle atrophy: Long term reduced use of joint can lead to decreased physical activity and loss of surrounding muscle.

