Table of Contents
ToggleChancroid(Soft Chancre)
Chancroid is a sexually transmitted infection that causes painful open sores, or chancroids, to develop in the genital area. It can also often cause the lymph nodes in the groin to swell and become painful.
Incubation period: 2-5 days.

Cause
Chancroid is a sexually transmitted infection (STI) caused by the bacteria Haemophilus ducreyi.
Risk Factors:
Contracting chancroid primarily occurs through direct contact with the open sores of an infected individual. Additional risk factors include:
- Unprotected sexual contact
- Multiple sexual partners
- Sexual engagement with sex workers
- Substance abuse
- Anal intercourse
- General sexual activity
- Residence in specific developing nations
- Rough intercourse
Signs and symptoms:
- A small, painful ulcer appears on the genital parts, known as a soft chancre.
- Enlargement and inflammation of the inguinal area with pus.
- Headache.
- Fever.
- Generalized malaise.
Treatment:
Timely medical intervention is crucial, usually involving a prescribed course of antibiotics. Recommended antibiotic therapies include:
- Azithromycin: 1 g orally once daily.
- Ceftriaxone: 250 mg intramuscular once daily.
- Ciprofloxacin: 500 mg orally twice daily for 3 days.
- Erythromycin base: 500 mg orally three times a day for 7 days.
- Completing the full antibiotic course is imperative to prevent chronic or untreated infections, which are more challenging to address. Follow-up assessments after 3 to 7 days may involve reevaluation, medication adherence checks, testing for other STIs, and consideration of antibiotic resistance in H. ducreyi strains.
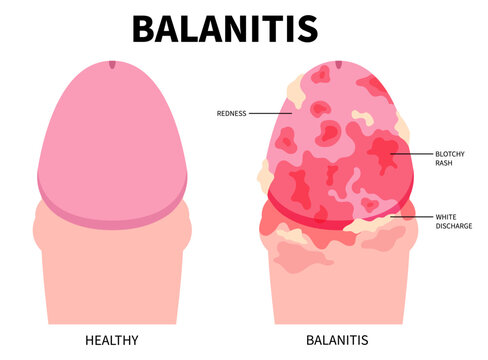
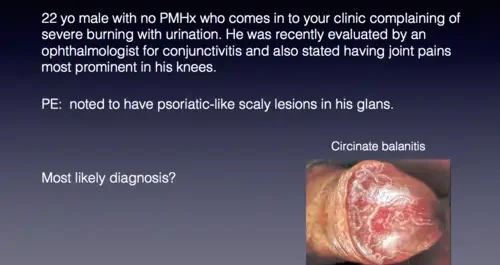
Balanitis
Balanitis refers to the inflammation of the glans penis, a condition that can be influenced by various factors, with Candida being a common causative agent, and Trichomonas, though rare, also implicated.
Aetiology:
The primary causative agents for balanitis are fungal, with Candida being the commonest. In rare cases, Trichomonas may contribute to the inflammation.
Clinical Features:
- Discharge: Patients often present with noticeable discharge, indicating the presence of infection.
- Erythema: Redness and inflammation of the glans penis are common clinical features.
- Erosions: The presence of erosions on the glans further characterizes the inflammatory condition.
- Retractable Prepuce: The prepuce is retractable..
Management:
Effective management of balanitis involves an approach aimed at addressing the underlying infection and promoting genital hygiene.
- Fluconazole 200 mg Stat: A single, stat dose of Fluconazole is recommended to combat fungal infections effectively.
- Metronidazole 400 mg Every 12 Hours for 7 Days: The addition of Metronidazole, administered every 12 hours over a week, provides broad-spectrum coverage, particularly against certain anaerobic microorganisms.
- Hygiene Counselling: Patients are advised on proper genital hygiene practices to mitigate the risk of recurrent infections.
- Circumcision: Circumcision is suggested as part of the management plan, potentially reducing the risk of future episodes.
Follow-Up Measures:
In cases where the condition persists despite initial management:
- Partner Treatment: Ensuring the partner receives appropriate treatment to prevent potential reinfection and establish comprehensive care.

Syphilis:
Syphilis is an STI caused by the spirochete known as Treponema Pallidum, with an incubation period of 9-90 days.
Modes of transmission:
- Vertical transmission through mother to child during intrauterine life (transplacental).
- Direct contact with infected discharges.
- Sexually (unprotected sex) with infected persons.
Signs and symptoms:
Primary stage:
- Identified by the presence of painless sores or lesions, known as chancre, which disappears at the site of contact from the 10th to 90th day after initial exposure.
- The sore/chancre is firm, painless, superficial, ulcerated, and may persist for 4-6 weeks, healing spontaneously.
- Painless regional Lymphadenopathy may develop within 1-2 weeks after the appearance of the chancre. This stage may be missed since the sore is usually painless.
Secondary stage:
- Occurs about 1-6 months after the primary infection.
- Characterized by flu-like syndrome (mild pyrexia, headache, anorexia, and sometimes weight loss).
- Lymphadenopathy and the appearance of systemic reddish-pink rashes on the trunk, extremities, palms, soles of the feet, anus, and vagina.
- Flat-broad whitish lesions develop from the rash, known as Condylomata Lata.
- Grey-white patches on the tongue, soft palate, and throat, known as Snail Tracks.
- Loss of hair (alopecia) may occur.
- Serological tests are positive.
- This stage may last up to 9 months and is followed by a latent period where no clinical signs are present.
Latent period:
- A period of natural cure with no clinical presentations. Lesions disappear, and the patient feels perfectly well.
Tertiary stage:
- Affects the cardiovascular and nervous systems 1-10 years after initial infection.
- Without treatment, complications may include:
Swelling (gumma) on the skin, mucous membrane, and bones.
Ulceration of skin swellings resulting in chronic ulcers.
Spread to the cardiovascular system may lead to aortic aneurysm, aortic insufficiency, or coronary arteriosclerosis.
Spread to the nervous system may result in memory loss, confusion, mental disability, and general paralysis of the insane.
Joint degeneration, failing sight, and deafness may occur.
Diagnosis:
- VDRL (venereal disease research laboratory) test.
- RPR (rapid plasma reagent) test, which confirms the presence of the disease.
- Rahm test and Wasserman are some of the tests for syphilis.
Treatment:
- No penicillin resistance exhibited
- Benzyl benzathine penicillin 2.4 mu weekly 3-4 doses/Benzathine benzyl penicillin 2.4 mu once weekly for 3 weeks.
- Allergic patients will be treated with erythromycin 500mg orally 6 hourly for 2 weeks.
- All exposed sexual partners should be treated
- Treated patients need blood tests at 3-month intervals to ensure freedom from the bacterium
- To prevent birth defects and fetal death, all pregnant women are recommended to be tested for syphilis at the first prenatal visit
- Babies of mothers diagnosed with or showing signs of syphilis are given Benzathine penicillin 50,000 IU as a single dose into the lateral aspect of the thigh.
Education of clients:
- Drug compliance to ensure care and prevent resistance.
- Explanation of the risk of vertical transmission.
- Mandatory patient treatment.
- Partner counselling and testing for HIV.
- Abstinence during treatment or correct and consistent use of condoms.
Effects of untreated syphilis in pregnancy and childbirth:
- Mid-trimester abortion, usually after 20 weeks.
- Premature labour.
- Intrauterine foetal death.
- IUGR (Intrauterine Growth Restriction).
- Stillbirth, usually macerated.
- Congenital syphilis.
- Aortic aneurysm and insufficiency from spread to the cardiovascular system.
- Loss of memory, confusion, mental disability, and general paralysis of the insane.
- Coronary artery stenosis.
- Joint degeneration, failing sight, and deafness.
Basic Facts About STIs:
Sexually transmitted diseases (STDs) are infectious conditions caused by one or more microorganisms primarily transmitted from one infected person to another during unprotected sexual intercourse.
The following table provides a summary of the most common STDs, categorizing them based on their etiological grouping and highlighting their main clinical features.
STD | Main Clinical Features | Causative Agents | Incubation Period |
Bacterial STIs | |||
Gonorrhoea | Pus discharge from urethra or cervix, dysuria, frequency | Neisseria Gonorrhoea | 2-6 days |
Syphilis | Primary chancre is painless, well-demarcated ulcer; other features depend on clinical stage | Treponema pallidum | 2-4 weeks |
Non-gonococcal urethritis/cervicitis | Thin, non-itchy discharge from cervix or urethra | Chlamydia, Mycoplasma hominis, and others | 7-14 days |
Lymphogranuloma venereum (LGV) | Swollen, painful inguinal glands (buboes) occasionally with an ulcer; may be bilateral | Chlamydia organism, LGV strains | 3-30 days |
Granuloma inguinale | Heaped-up (beefy) ulcer, usually painless, associated with inguinal lymph node swelling | Calymatobacteria granulomatis | 1-10 weeks |
Bacteria vaginosis | Thin discharge with a fishy smell from the vagina | Gardnerella vaginalis | May be endogenous |
Chancroid | Dirty, painless ulcer, usually underlying | Haemophilus ducreyi | 1-3 weeks |
Viral STIs | |||
Herpes Genitalis | Recurrent small, multiple painful ulcers beginning as vesicles | Herpes Simplex Virus | 2-7 days (initial infection) |
Hepatitis B virus infection (HBV) | Jaundice with inflammation of the liver | Hepatitis B virus | Varies |
HIV/AIDS | According to WHO clinical criteria for the case definition for AIDS | Human Immunodeficiency Virus | Months-10 years or more |
Venereal warts/HPV | Finger-like growths on the genitals | Human Papilloma Virus | Weeks-months |
Fungal STIs | |||
Genital candidiasis | White curd-like discharge coating vaginal walls, itchiness, soreness, excoriation, cuts | Candida Albicans | May be endogenous and recurrent |
Ringworm (fungal) | Patches of hypo/hyperpigmentation in the pubic area | Tinea Organisms | Varies |
Protozoal STI | |||
Trichomoniasis | Greenish, itchy discharge from the vagina with an offensive smell | Trichomonas vaginalis | Variable |
Other STIs | |||
Scabies | Vesicles containing mites in the pubic area | Sarcoptes scabiei | 30 days |
Pediculosis (vermin) | Presence of nits in pubic hair, itching in pubic area | Phthirus pubis (pubic lice) | 7 – 10 Days |
Risk Factors for STI/STDs:
Risk factors contributing to the prevalence of STDs in Uganda encompass a range of influential elements. These include:
- Multiple Sexual Partners: Engaging with numerous sexual partners increases the risk of contracting and spreading STDs.
- Lack of and Inconsistent Condom Use: Inadequate or irregular use of condoms exposes individuals to heightened susceptibility to sexually transmitted infections.
- Lack of Circumcision in Men: Non-circumcision in men has been identified as a potential risk factor for the transmission of STDs.
- Alcohol/Drug Use: Alcohol consumption and drug use significantly impact sexual health. Regular alcohol use, especially in social contexts, may lead to less discerning choices in sexual partners, lower inhibitions, and hinder the negotiation and correct usage of condoms during sexual activities.
- Early Sexual Involvement by Younger Age Group: Premature engagement in sexual activities among younger age groups contributes to the prevalence of STDs.
- Socio-Cultural Factors, such as Early Marriage: Societal and cultural norms, including early marriage practices, can contribute to the spread of STDs.
- Economic Factors, Particularly Poverty: Economic challenges, notably poverty, can limit access to preventive measures and healthcare services, increasing vulnerability to STDs.
- Gender-Related Factors, Including Limited Negotiation Powers for Women: Gender dynamics, where women may have restricted negotiation powers concerning sexual matters, contribute to the risk of STD transmission.
- Legal and Human Rights Constraints, Stigma, and Discrimination: Legal prohibitions, human rights limitations, and the stigma associated with certain populations, such as sex workers, can affect interventions aimed at preventing and controlling STDs.
- Inequality in Access to Social and Health Services: Differences in accessing social and health services further increases the risk of STDs, creating a scenario where certain populations face increased vulnerability.