CONGENITAL CATARACTS
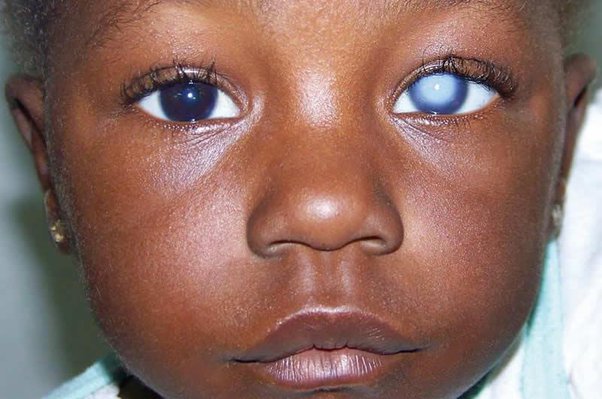
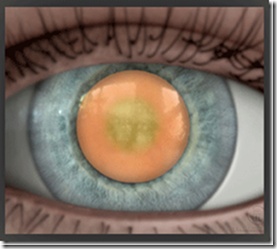
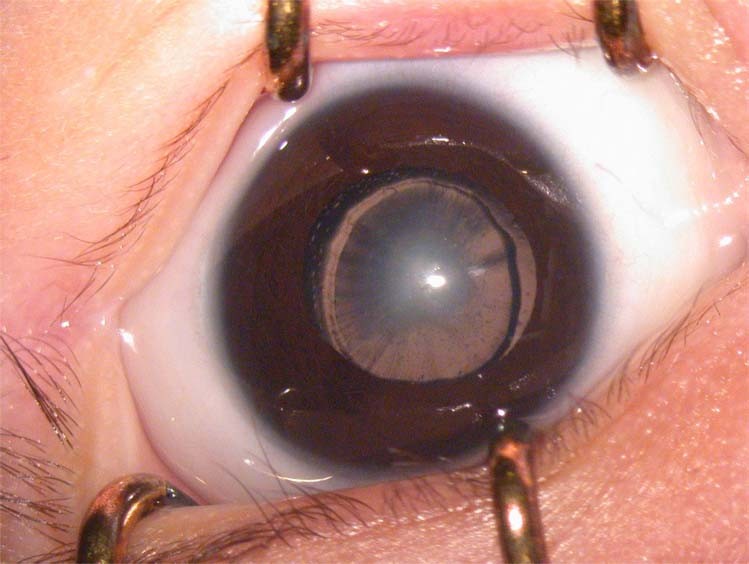
Congenital cataracts are a type of cataract that occurs at birth or during a baby’s first year of life, characterized by clouding or opacity of the lens of the eye.
A lens of the eye is the transparent tissue that helps focus light onto the retina.
Congenital cataracts cover a broad spectrum of severity: whereas some lens opacities do not progress and are visually insignificant, others can produce profound visual impairment. Therefore, Congenital cataracts can be Visually significant or not, Stable or Progressive, Congenital or Acquire, Unilateral or Bilateral or else, Partial or Complete.
Classifications of Congenital Cataracts.
Congenital cataracts can be classified based on various factors such as morphology, age of onset, and etiology.
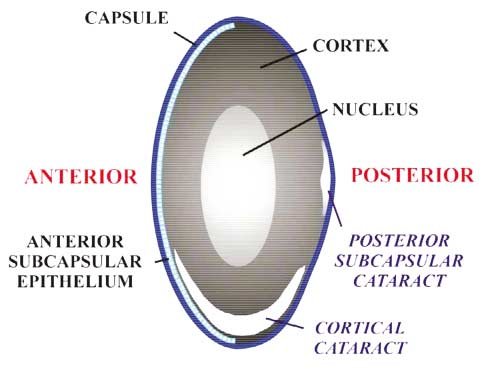
Morphology: Based on their physical appearance.
- Polar Cataract: Lens opacities that involve the subcapsular cortex and lens capsule of the anterior or posterior pole of the lens. Anterior polar cataracts present as Small, bilateral, symmetric, non progressive opacities that do not impair vision. Posterior polar cataracts produce more visual impairment than anterior polar cataracts because they tend to be larger and are positioned closer to the nodal point of the eye.
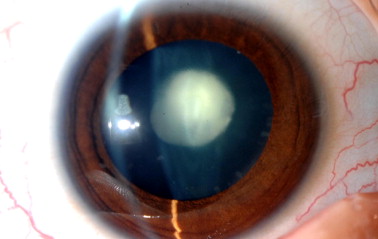
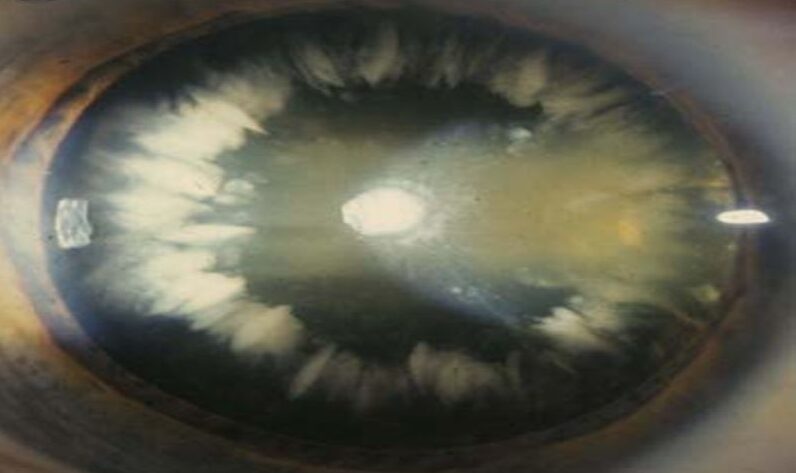
- Lamellar Cataract/Zonular Cataract: Lamellar cataracts are the most common type of congenital cataracts. The cataract is visible as an horseshoe- shaped opacity that surrounds a clearer center and is itself surrounded by a layer of clear cortex. Lamellar cataracts may be inherited or result from a transient toxic influence during embryonic lens development.
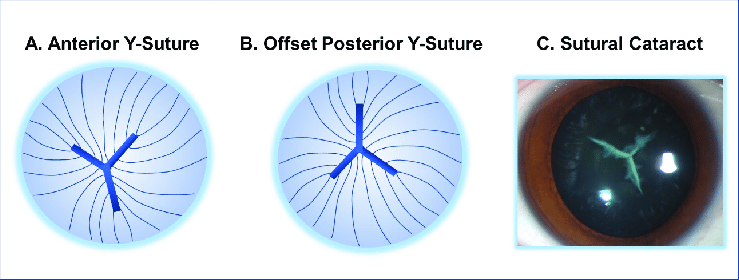
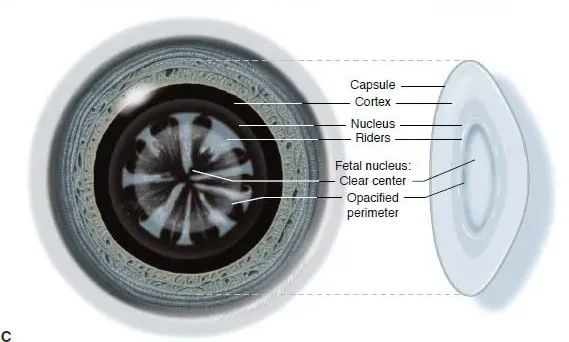
- Sutural Cataract: Opacification of the Y-sutures of the fetal nucleus that commonly do not impair vision. They are usually bilateral, symmetric, and frequently inherited in an autosomal dominant pattern. These opacities often have branches or knobs projecting from them.
- Coronary Cataract: Coronary cataracts consist of club-shaped cortical opacities arranged around the equator of the lens like a crown or corona. They cannot be seen unless the pupil is dilated, and they usually do not affect visual acuity. They are often inherited in an autosomal dominant pattern.
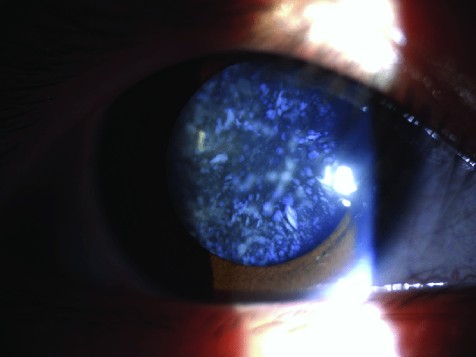
- Cerulean Cataract/Blue-dot Cataract: Cerulean cataracts are small bluish opacities located in the lens cortex. They are nonprogressive and usually do not cause visual symptoms.
- Nuclear Cataract: Opacities of either the embryonic nucleus alone or both the embryonic and fetal nuclei. They are usually bilateral, with a wide spectrum of severity. Eyes with congenital nuclear cataracts tend to be microphthalmic and have an increased risk of developing aphakic glaucoma.
- Capsular Cataract: Small opacifications of the lens epithelium and anterior lens capsule that spare the cortex. They are differentiated from anterior polar cataracts by their protrusion into the anterior chamber, but generally do not affect vision.
- Membranous Cataract: Membranous cataracts occur when lens proteins are resorbed, allowing the anterior and posterior lens capsules to fuse into a dense white membrane. They cause significant visual disability due to the resulting opacity and lens distortion.
Age of Onset:
- Congenital/Infantile cataract: Lens opacities present at birth.
- Acquired/Juvenile cataract: Onset after infancy, in childhood.
Etiology:
- Genetic cataract/Hereditary: Caused by mutations in genes involved in lens structure or clarity. The affected individuals are usually perfectly well, and have no associated systemic illness. Associated with microphthalmos.
- Metabolic cataract: Caused by metabolic disorders such as galactosemia, hypoglycemia, hypocalcemia. Galactosemia is a metabolic disorder in which the child’s body cannot metabolize galactose, a major component of milk and milk products. The baby develops typical ‘oil droplet’ cataracts which are easily seen by examining the red reflex. These are reversible, and the lens returns to normal on removing dairy products from the diet.
- Traumatic cataract: Caused by external injuries to the eye. Trauma is the most common cause of unilateral cataract in children. Traumatic cataract is usually the result of a penetrating injury, though blunt trauma can also lead to cataract formation.
- Secondary cataracts: Such as those secondary to marternal infection during pregnancy. TORCH syndrome: Toxoplasmosis, Others(Syphilis, Hepatitis B), Rubella, Cytomegalovirus (CMV), Herpes infection.. Usually bilateral, dense, and central. The most common maternal infection to cause congenital cataract in the child is Rubella. The cataracts caused by Rubella may be present at birth, or develop several months later.
- Iatrogenic cataract: Caused by well-intentioned medical treatment, Such as Radiation, Drugs, Surgeries, e.t.c. latrogenic cataract is most commonly seen in children who have had Total body irradiation for leukemia, Organ transplants, On long-term systemic steroid therapy. These children are usually older children and do very well after cataract surgery.
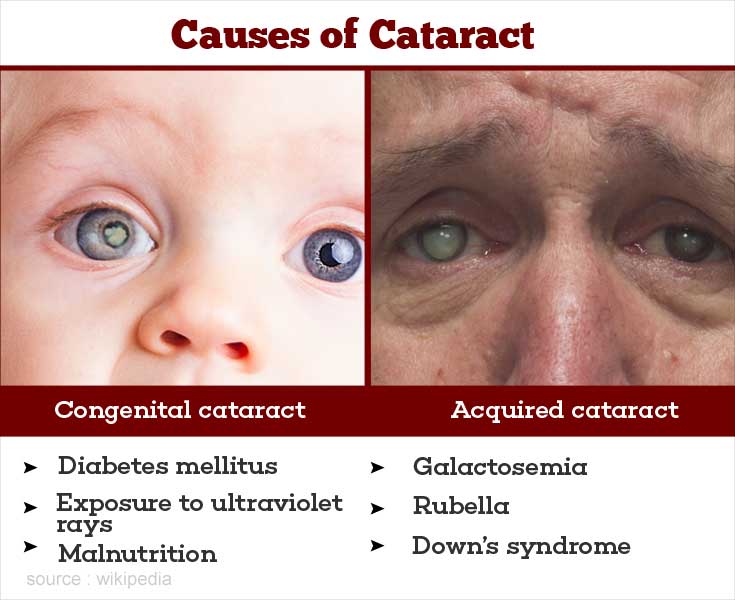
Causes of Congenital Cataracts
The causes of congenital cataracts can vary and may include genetic factors, infections, physical trauma during pregnancy, hypoglycemia, and premature birth, It’s important to note that in many cases, the exact cause of congenital cataracts is not known.
Genetic Factors: In some cases, congenital cataracts are caused by a faulty gene that is passed from parents to their child. It is estimated that around 1 in every 5 cases of congenital cataracts have a family history of the condition.
Infections: Certain infections during pregnancy can increase the risk of congenital cataracts in babies. These infections include:
- Infections during pregnancy, such as those caused by STORCH (Syphilis, Toxoplasmosis, Rubella, Cytomegalovirus, and Herpes simplex), can lead to congenital cataracts.
- Other infections like influenza, measles, polio, and rubella.
- Other conditions: Certain conditions like hypoparathyroidism, Conradi syndrome, aniridia, anterior segment dysgenesis, persistent fetal vasculature (PFV), posterior lenticonus, and corticosteroid use can also contribute to the development of congenital cataracts.
Physical Trauma during Pregnancy: Physical trauma to the mother’s abdomen during pregnancy, such as from a car accident, a fall, or intimate partner violence, can cause injury to the baby’s eyes in the womb and lead to congenital cataracts.
Hypoglycemia during Pregnancy: Hypoglycemia, which is low blood sugar levels, can occur in pregnant women with uncontrolled diabetes. This condition may increase the risk of congenital cataracts in the baby.
Premature Birth: Babies born prematurely, before 37 weeks of pregnancy, have a higher risk of developing congenital cataracts.
Metabolic disorders: Certain metabolic disorders, such as galactosemia and hypoglycemia, can increase the risk of developing congenital cataracts.
Syndromes: Several syndromes have been associated with congenital cataracts, including Down syndrome, Lowe syndrome, Cockayne syndrome, Marfan syndrome, Trisomy 13-15, Alport syndrome, Myotonic dystrophy, Fabry disease, and Incontinentia pigmenti.

Diagnosis and Investigations for Congenital Cataracts:
Diagnosing congenital cataracts involves a comprehensive eye examination by an ophthalmologist, who specializes in eye disorders.
There is no benefit in doing a large number of tests and investigations on all children with cataract. It is better to take a careful history.
- Family History and Genetic Testing: A detailed family history is important, as congenital cataracts can have a genetic component. Genetic testing may be recommended to identify specific gene mutations associated with cataract formation.
- Complete Eye Examination: This includes a thorough evaluation of the infant’s eyes, including visual acuity assessment, examination of the lens, and assessment of the red reflex. The red reflex is particularly useful in estimating the size and location of the cataract within the visual axis. The red reflex test is best performed in a darkened room and involves shining a bright direct ophthalmoscope into both eyes simultaneously from a distance of 1– 2 ft.
- Slit Lamp Examination: A slit lamp is a specialized microscope that allows the ophthalmologist to examine the structures of the eye in detail. It helps in visualizing the cataract and determining its characteristics, such as size, location, and morphology.
- Intraocular Pressure Measurement: This test measures the pressure inside the eye and helps in assessing or ruling out other conditions.
- Ultrasound of the Posterior Pole: In cases where the cataract is not clearly visible, an ultrasound may be performed to visualize the posterior pole of the eye and assess the presence of any abnormalities.
- Laboratory Tests: Depending on the clinical presentation and suspected underlying cause, various laboratory tests may be performed. These may include TORCH (toxoplasmosis, rubella, cytomegalovirus, varicella) screening, Venereal Disease Research Laboratory (VDRL) test for syphilis, blood tests for calcium, phosphorus, glucose, and galactokinase levels, and urine tests for reducing sugars.
Management of Congenital Cataracts
Management and treatment of congenital cataracts involve a multidisciplinary approach and may vary depending on the specific case and underlying cause.
Aims of Management
- To remove the cloudy lens and restore clear vision in the affected eye(s).
- Regaining the usual level of cognition.
- Recognizing awareness of sensory needs.
- Preventing injury.
- Identifying potential risk factors in the environment.
- Reducing anxiety to a manageable level.
- Providing education on coping with altered abilities
In general, the younger the child, the greater the urgency in removing the cataract, because of the risk of amblyopia.
- For optimal visual development in newborns and young infants, a visually significant unilateral congenital cataract should be detected and removed before age 6 weeks, and visually significant bilateral congenital cataracts should be removed before age 10 weeks.
- Some congenital cataracts are too small to affect vision, therefore no surgery or treatment will be done. If they are superficial and small, an ophthalmologist will continue to monitor them throughout a patient’s life.
- Commonly, a patient with small congenital cataracts that do not affect vision will eventually be affected later in life; generally this will take decades to occur .
- Congenital cataracts are one of the most common treatable causes of visual impairment and blindness during infancy, with an estimated prevalence of 1 to 6 cases per 10,000 live births.
Nursing Assessment:
- Recent medication intake: Anticoagulant therapy may be withheld to reduce the risk of retrobulbar hemorrhage.
- Preoperative tests: Standard preoperative tests such as complete blood count, electrocardiogram, and urinalysis may be prescribed based on the patient’s medical history.
- Vital signs: Stable vital signs are necessary before surgery. These include TPR/Bp.
- Visual acuity test results: Assessment of visual acuity using tests like Snellen’s chart is important.
- Patient’s medical history: Assessing the patient’s medical history helps determine the required preoperative tests.
Nursing Diagnosis:
- Disturbed visual sensory perception related to altered sensory reception or status of sense organs as evidenced by the patient using hand to locate environment.
- Risk for trauma related to poor vision and reduced hand-eye coordination.
- Anxiety related to the threat of permanent loss of vision/independence as evidenced by the patients restlessness.
Medical Management: Pharmacologic Therapy:
- Dilating drops: These are administered pre and postoperatively to dilate the pupil and facilitate surgery.
- Antibiotic drugs: Prophylactic administration of antibiotics helps prevent postoperative infection and inflammation.
- Intravenous sedation: Sedation may be used to minimize anxiety and discomfort before surgery.
Surgical Intervention:
- Surgery is the mainstay of treatment for congenital cataracts.
- Pediatric ophthalmologists who specialize in congenital cataract surgery perform the procedure.
- During surgery, a small incision is made in the eye, and the cloudy lens is removed.
- In some cases, additional surgical procedures may be required, such as intraocular lens implantation or capsulotomy.
Lens Replacement:
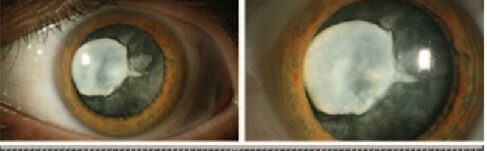
- Phacoemulsification: This procedure involves removing a portion of the anterior capsule, extracting the lens nucleus and cortex, and leaving the posterior capsule and zonular support intact. Different lens replacement options include aphakic glasses, contact lenses, and intraocular lens (IOL) implants.
- Extracapsular cataract extraction (ECCE): This procedure removes the anterior lens and cortex, leaving the posterior capsule intact.
- Intracapsular cataract extraction: This procedure removes the entire lens within the intact capsule.
Timing of Surgery:
- The timing of surgery depends on various factors, including the age of the child, the severity of the cataract, and the presence of any associated eye conditions.
- Early surgery is generally recommended to prevent visual deprivation and promote normal visual development.
- In some cases, surgery may be delayed if there are other medical conditions that need to be addressed first.
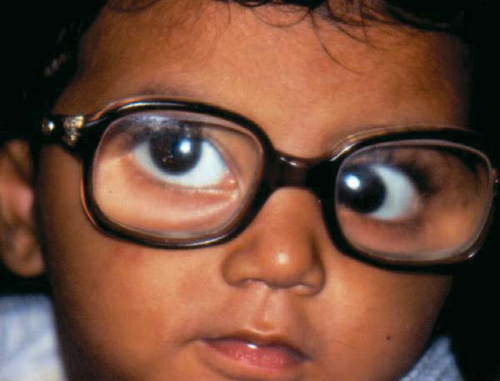
Correction of Refractive Errors:
- After cataract surgery, children may develop refractive errors, such as nearsightedness or farsightedness.
- Corrective measures, such as glasses or contact lenses, may be prescribed to optimize visual acuity.
Amblyopia Management:
- Amblyopia, also known as lazy eye, is a common complication of congenital cataracts.
- Amblyopia occurs when the brain favors one eye over the other due to visual deprivation.
- Treatment may involve patching or blurring the stronger eye to encourage the use and development of the weaker eye.
Regular Follow-up and Monitoring:
- Children with congenital cataracts require long-term follow-up and monitoring by a pediatric ophthalmologist.
- Regular eye examinations are essential to assess visual acuity, monitor for any complications, and adjust treatment as needed.
Complications of congenital cataracts
- Cloudy Vision: After cataract surgery, a condition called posterior capsule opacification (PCO) can occur. This is when part of the lens capsule thickens and causes cloudy vision. PCO is not the cataract returning, but rather the growth of cells over the artificial lens. It usually develops within 4 to 12 months after surgery and may require another operation to correct it.
- Lazy Eye: Lazy eye, also known as amblyopia, can occur if there is weaker vision in one eye. The brain may ignore the visual signals from the weaker eye, leading to improper development of vision. Treatment for lazy eye usually involves wearing a patch over the stronger eye.
- Glaucoma: Increased pressure inside the eye, known as glaucoma, can affect vision. Children who have had cataract surgery are at a lifelong risk of developing glaucoma and will need regular eye pressure measurements by an optician.
- Squint: A squint, also called strabismus, is a condition where the eyes look in different directions. It can occur as a complication after cataract surgery.
- Pupil Abnormalities: Pupil abnormalities, such as the pupil becoming a more oval shape, can occur but usually do not affect vision significantly.
- Retinal Detachment: Retinal detachment is a condition where the retina becomes separated from the inner wall of the eye, leading to vision impairment. It can be a complication after cataract surgery.
- Cystoid Macular Edema: Cystoid macular edema is the buildup of fluid between layers of the retina, which can affect vision.
- Infection: In rare cases, an infection called endophthalmitis can occur after cataract surgery. It may require medication or further surgery for treatment