Table of Contents
ToggleGLAUCOMA
Glaucoma is a group of disorder characterized by an abnormally high intraocular pressure , optic nerve dystrophy, and peripheral filed loss. (BRUNNER)
Glaucoma is a group of eye diseases which result in damage to the optic nerve and vision loss due to IOP.
It’s among the common causes of blindness.
Glaucoma occurs as a result of increased intraocular pressure (IOP) caused by a malformation or malfunction of the eyes drainage system.
The main cause of damage to the optic nerve is intraocular pressure (IOP), excessive fluid pressure within the eye, which can be due to various reasons including blockage of drainage ducts, and narrowing or closure of the angle between the iris and cornea.
Normal intraocular pressures average from 12-21 mm Hg. The increased pressure causes compression of the retina and the optic nerve, and causes progressive , permanent loss of eyesight if left untreated.
INCIDENCE
- Globally 6 to 67 million.
- More common in peoples older than 40 years.
Glaucoma has been called the “silent thief of sight” because the loss of vision usually occurs slowly over a long period of time. Worldwide, glaucoma is the second-leading cause of blindness after cataracts.
Normal Pathway of Aqueous Humor
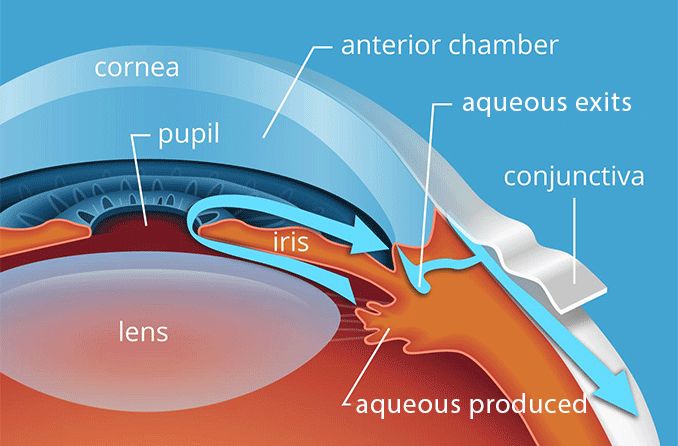
Aqueous fluid Circulation:
- The aqueous fluid is a clear fluid produced in the Cilliary body then it will flow out through the Iris, lens, Pupil, Cornea, Anterior Chamber Trabecular Meshwork then to the Schlemm Canal.
- The aqueous fluid flows nourishing the cornea and lens.
- The eye has an internal fluid circulation system
- Fluid is produced at the base of the iris
- The fluid flows through the pupil to the front of the iris
- The fluid exits the eye at the angle between the iris and the cornea where it drains through a spongy meshwork
The IOP is determined by:
- Rate of aqueous production in the ciliary body
- Resistance encountered by the aqueous as it flows out of the passages.

Causes/ Aetiology of Glaucoma
Glaucoma is a chronic eye disease that can lead to vision loss and blindness. We have primary causes of glaucoma which refers to the underlying mechanism or condition that directly leads to the development of glaucoma or secondary causes of glaucoma which refer to an underlying condition or factor that contributes to the development of glaucoma.
Primary Causes of Glaucoma:
- Increased Eye Pressure: One of the major risk factors for glaucoma is elevated eye pressure. An abnormality in the eye’s drainage system can cause fluid to build up, leading to excessive pressure that damages the optic nerve.
- Optic Nerve Damage: Glaucoma develops when the optic nerve becomes damaged. The exact reason for this nerve damage is not fully understood, but it is often related to increased eye pressure.
- Fluid Buildup: The fluid inside the eye, known as aqueous humor, may not drain properly due to a malfunction in the drainage system. This can result in a gradual increase in eye pressure, leading to glaucoma.
Secondary Causes of Glaucoma:
- Angle-Closure Glaucoma: This form of glaucoma occurs when the iris bulges and partially or completely blocks the drainage angle, preventing fluid circulation and increasing eye pressure.
- Normal-Tension Glaucoma: In some cases, optic nerve damage occurs even when eye pressure is within the normal range. The exact cause of this type of glaucoma is unknown, but it may be related to reduced blood flow to the optic nerve.
- Glaucoma in Children: Children can be born with glaucoma or develop it in the first few years of life. Blocked drainage, injury, or underlying medical conditions can cause optic nerve damage in children.
- Pigmentary Glaucoma: In pigmentary glaucoma, pigment granules from the iris can block or slow fluid drainage from the eye, leading to increased eye pressure.
- Inflammation of the Middle Layer of the Eye: Uveitis, which is inflammation of the middle layer of the pigmented vascular eye structure, can lead to uveitic glaucoma
Risk Factors for Glaucoma:
- High Internal Eye Pressure: Elevated intraocular pressure is a significant risk factor for glaucoma.
- Age: Glaucoma is more common in older adults, especially those over the age of 60.
- Ethnicity: Individuals of Black, Asian, or Hispanic heritage have a higher risk of developing glaucoma.
- Family History: Glaucoma tends to run in families, so having a close relative with glaucoma increases the risk.
- Medical Conditions: Certain medical conditions, such as diabetes, migraines, high blood pressure, and sickle cell anemia, can increase the risk of glaucoma.
- Thin Corneas: Having thin corneas is associated with a higher risk of glaucoma.
- Extreme Nearsightedness or Farsightedness: Individuals with severe nearsightedness or farsightedness are at an increased risk of developing glaucoma.
- Eye Injury or Surgery: Previous eye injuries or certain types of eye surgery can increase the risk of glaucoma.
- Long-term Use of Corticosteroid Medications: Taking corticosteroid medicines, especially eye drops, for an extended period can increase the risk of glaucoma.
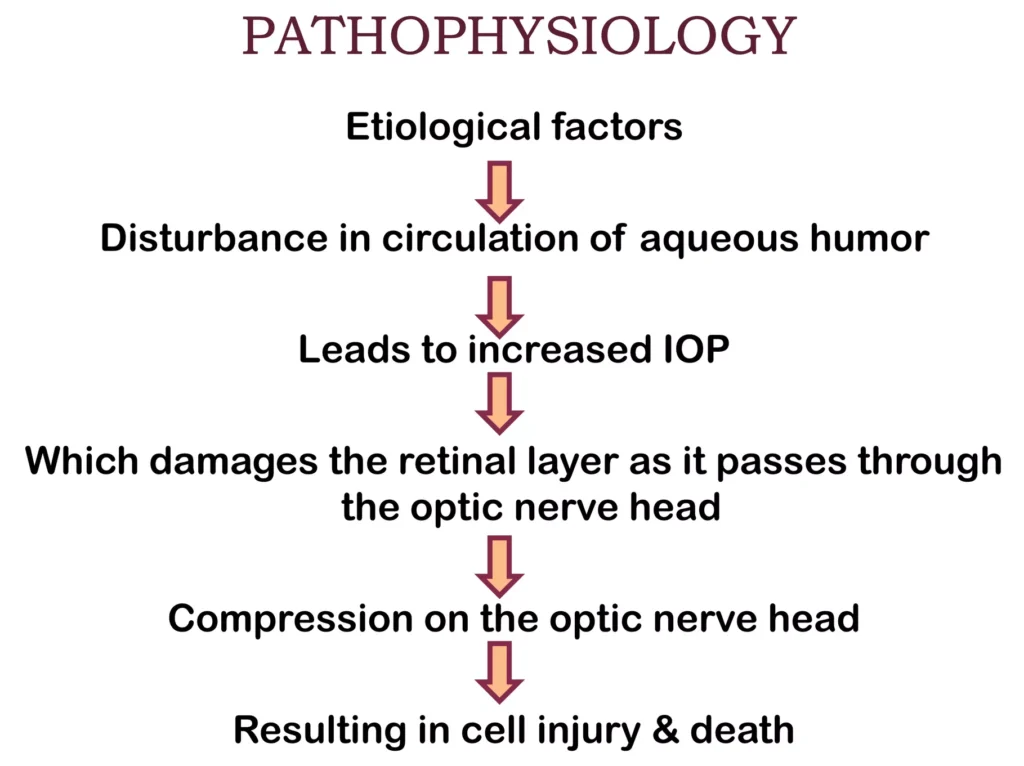
Pathophysiology of Glaucoma
The underlying cause of open-angle glaucoma remains unclear.
Excess production of aqueous humor, and decreased outflow of aqueous humor, are the key factors in the pathophysiology of glaucoma.
Excess production of aqueous humor can occur, leading to an increase in intraocular pressure. Additionally, there may be a decrease in the outflow of aqueous humor due to blockage or narrowing of the drainage pathways.
The increased intraocular pressure puts pressure on the optic nerve, compromising its blood supply and leading to ischemia. The optic nerve is responsible for transmitting visual information from the eye to the brain. When the optic nerve is damaged, it can result in the loss of vision.
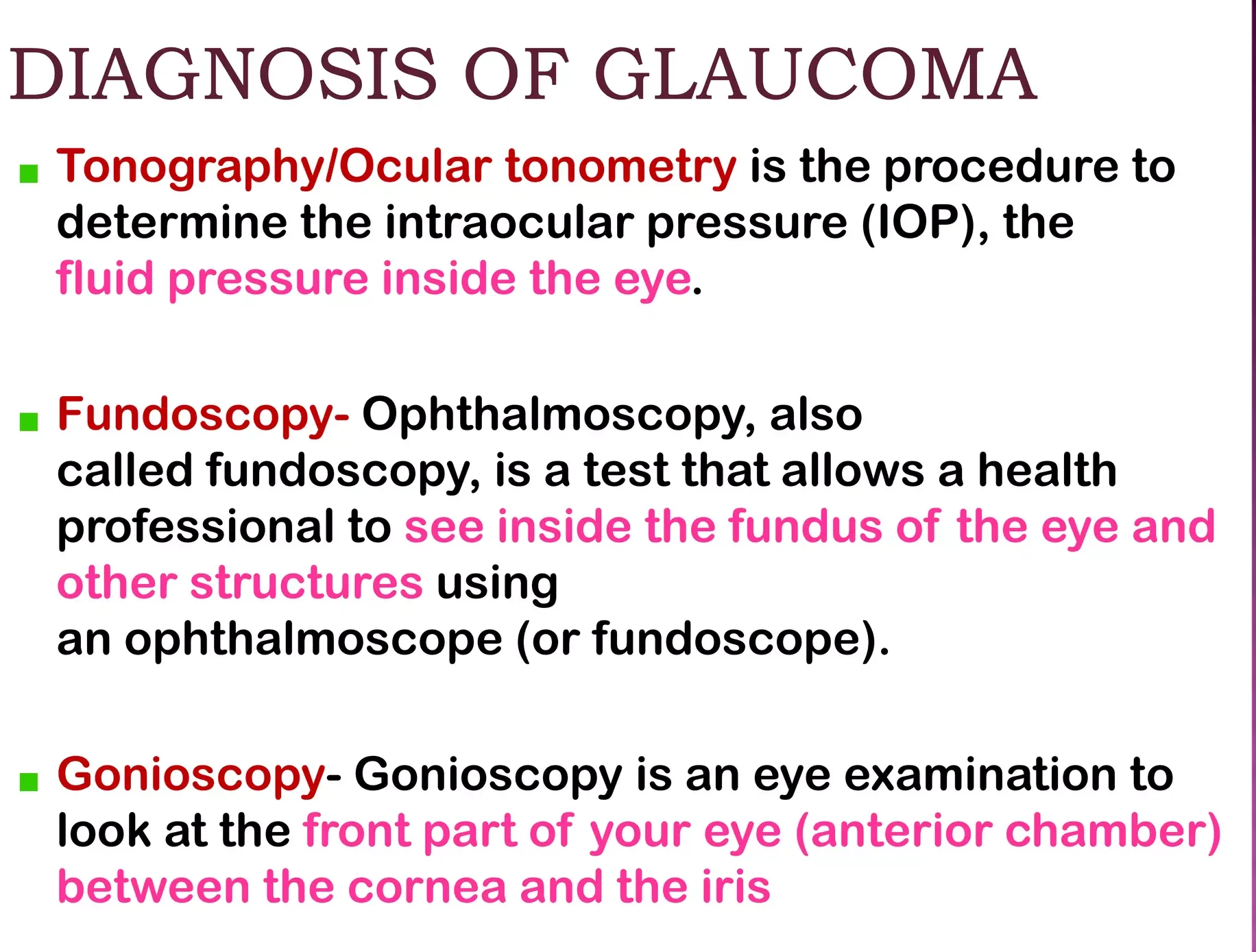
Diagnosis of Glaucoma
Screening for glaucoma is usually performed as part of a standard eye examination performed by optometrists and ophthalmologists.
- History taking: Examination for glaucoma also could be assessed with more attention given to sex, race, history of drug use, refraction, inheritance and family history.
Glaucoma tests;
- Tonometry: This test measures the intraocular pressure (IOP) within the eye. The examiner will numb the eye with eye drops and then use a tonometer to measure the pressure. This can be done by applying a puff of warm air or using a tiny tool.
- Gonioscopy: This test examines the angle where the iris meets the cornea. Eye drops are used to numb the eye, and a hand-held contact lens with a mirror is gently placed on the eye to visualize the angle between the cornea and iris.
- Ophthalmoscopy (Dilated Eye Examination): This test examines the shape and color of the optic nerve. Eye drops are used to dilate the pupil, allowing the examiner to use a magnification device with a light to examine the optic nerve
- Perimetry (Visual Field Test): This test assesses the complete field of vision. Patient is asked to look straight ahead while a light spot is presented in different areas of the peripheral vision. This helps create a map of the vision.
- Pachymetry: This test measures the thickness of the cornea. A pachymeter is gently placed on the front of the eye to measure the corneal thickness. This measurement can help in understanding eye pressure readings.
- Nerve Fiber Analysis: Imaging techniques such as optical coherence tomography, scanning laser polarimetry, and scanning laser ophthalmoscopy can be used to assess the thickness of the retinal nerve fiber layer.
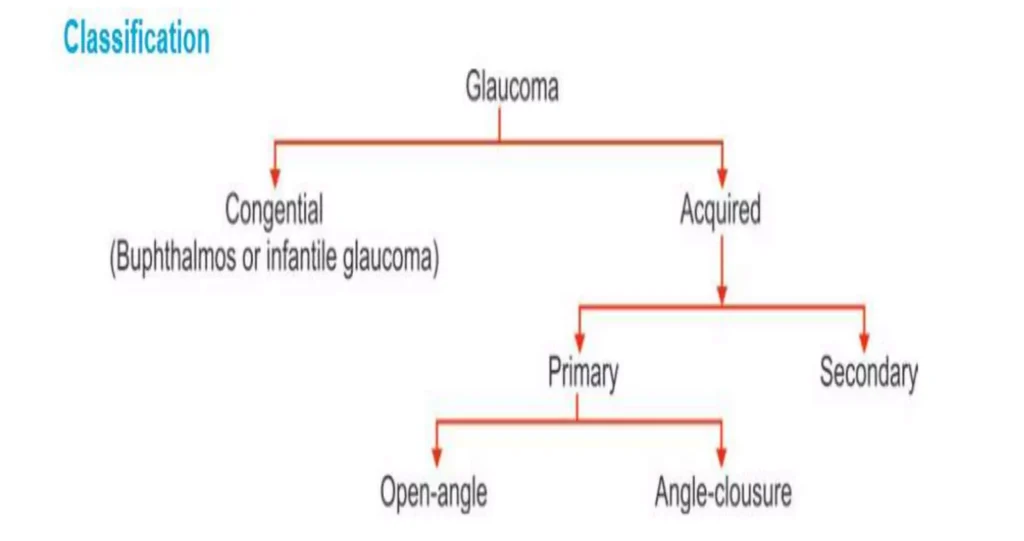
Classification of Glaucoma.
Glaucoma has been classified into specific types:

Congenital Glaucoma
Congenital glaucoma is a rare form of glaucoma that is present at birth or develops shortly after birth.
- It is characterized by abnormalities in the angle of anterior chamber obstructing the outflow of aqueous humour, leading to increased intraocular pressure and potential damage to the optic nerve.
- Congenital glaucoma can manifest at birth ( True Congenital) before 3 years ( Infantile) or between 3-16 years Juvenile).
Clinical Feature of Congenital Glaucoma.
- Age of onset: Congenital glaucoma presents in infants and young children, usually before the age of 3 years.
- Triad of symptoms: The classic triad of symptoms associated with congenital glaucoma includes :
- Watering (epiphora): Excessive tearing or watery eyes.
- Photophobia: Sensitivity to light.
- Blepharospasm: Involuntary contraction or twitching of the eyelids.
- Buphthalmos: Congenital glaucoma can cause enlargement of the eyeball, known as buphthalmos or “ox eye or bull’s eye” . This occurs due to increased intraocular pressure (IOP) and rapid expansion of the eye.
- Corneal changes: The elevated IOP in congenital glaucoma can lead to corneal enlargement and clouding. This can result in corneal edema and opacification, which may cause visual impairment.
- Haab striae: Horizontal or oblique breaks in Descemet membrane, known as Haab striae, can be seen in congenital glaucoma. These striae are a result of the stretching of the cornea due to increased IOP.
- Optic nerve damage: If left untreated or uncontrolled, congenital glaucoma can lead to optic nerve damage. This can result in vision loss.
- Variable presentation: The severity and presentation of congenital glaucoma can vary. Some cases may be unilateral (affecting one eye) while others may be bilateral (affecting both eyes).
- Blepharospasm (involuntary forceful closure of eyes): In congenital glaucoma, blepharospasm is a common clinical feature that refers to the involuntary and forceful closure of the eyelids.
- Excessive lacrimation: Excessive tearing or lacrimation is another common symptom of congenital glaucoma since the increased pressure in the eye can cause the tear ducts to produce more tears than usual.
- Enlarged and edematous cornea: The cornea, the clear front part of the eye, can become enlarged and edematous in congenital glaucoma. The increased pressure in the eye can lead to fluid accumulation in the cornea, causing it to swell which can result in cloudiness and opacification of the cornea.
- Thin and blue sclera: The sclera, the white outer layer of the eye, may appear thin and blue in congenital glaucoma, due to increased pressure in the eye. The blue color is due to the visibility of the underlying choroid layer through the thin sclera.
- Deep anterior chamber: Congenital glaucoma can cause a deepening of the anterior chamber, which is the space between the cornea and the iris. The increased pressure in the eye can push the iris backward, resulting in a deeper anterior chamber.
- Flat lens: In congenital glaucoma, the lens of the eye may appear flat. The increased pressure in the eye can affect the shape and position of the lens. This can lead to changes in the focusing ability of the eye.
- Optic disc atrophy: Optic disc atrophy, which refers to the degeneration and loss of nerve fibers in the optic disc, can occur in congenital glaucoma. The increased pressure in the eye can cause damage to the optic nerve.
Management of Congenital Glaucoma
The management of congenital glaucoma involves a combination of medical therapy and surgical interventions.
The main Aims of management is to lower intraocular pressure (IOP) and prevent further damage to the optic nerve.
Medical Therapy:
- Medical therapy is often used as a temporary measure to control IOP and clear the cornea before surgery.
- Medications such as topical beta-blockers like timolol, betaxolol, or prostaglandin analogs, and carbonic anhydrase inhibitors may be prescribed to reduce IOP.
Surgical Interventions:
1. Angle Surgery: The mainstay of treatment for congenital glaucoma is angle surgery, which aims to improve aqueous outflow and lower IOP.
- Goniotomy: In this procedure, an incision is made across the trabecular meshwork to improve drainage of aqueous humor.
- Trabeculotomy: This surgery involves incising the trabecular meshwork to create a new drainage pathway for aqueous humor.
2. Trabeculectomy: If angle surgery is not successful in controlling IOP, trabeculectomy may be performed. This procedure involves creating a new drainage channel to bypass the trabecular meshwork.
3. Glaucoma Implant Surgery: In cases where other surgical options fail, glaucoma implant surgery may be considered. This involves the placement of a drainage device, such as a Molteno, Baerveldt, or Ahmed implant, to regulate the flow of aqueous humor and lower IOP.
Follow-up and Monitoring:
- Regular follow-up visits with an ophthalmologist are essential to monitor IOP, assess the effectiveness of treatment, and detect any potential complications or disease progression.
- Ongoing management may involve adjustments to medication dosages, additional surgical interventions if necessary, and monitoring for potential long-term complications such as refractive errors or amblyopia.
ACQUIRED GLAUCOMA
Acquired glaucoma refers to glaucoma that develops later in life due to various factors such as age, genetics, underlying medical conditions, or trauma.
It is a chronic and progressive condition that requires ongoing management to control IOP and preserve vision.
It is further divided into;
PRIMARY GLUCOMA.
- Primary Open angle glaucoma.
- Primary angle closure Glaucoma
- Chronic angle closure glaucoma.
SECONDARY GLAUCOMA
- Lens induced glaucoma
- Glaucoma due to uveitis
- Neurovascular Glaucoma
- Glaucoma associated with intraocular tumor
- Steroid induced glaucoma.

PRIMARY OPEN-ANGLE GLAUCOMA (POAG)
Primary Open-Angle Glaucoma (POAG) also called as open angle glaucoma or chronic simple glaucoma or simple complex glaucoma results from the overproduction of aqueous humour through trabecular mesh work resulting into increased IOP and damage to optic nerve, resulting into loss of vision.
In this type there in no narrowing of the anterior chamber BUT there is resistance in the trabecular meshwork to aqueous flow resulting in gradual increase in IOP along with cupping of the optic disc and visual fields defects.
Predisposing factors for primary glaucoma include:
- Cigarette smoking.
- Diabetes Mellitus and Hypertension diseases.
- Myopia (nearsightedness).
- Old age.
Clinical features of primary glaucoma may include:
- Asymptomatic in the early stages.
- Mild headache and pain in the eye.
- Difficulty in reading.
- Delayed dark adaptation.
- Alteration in vision sites.
- Mild ache in the eyes
- Increased IOP ( more than24 mmhg)
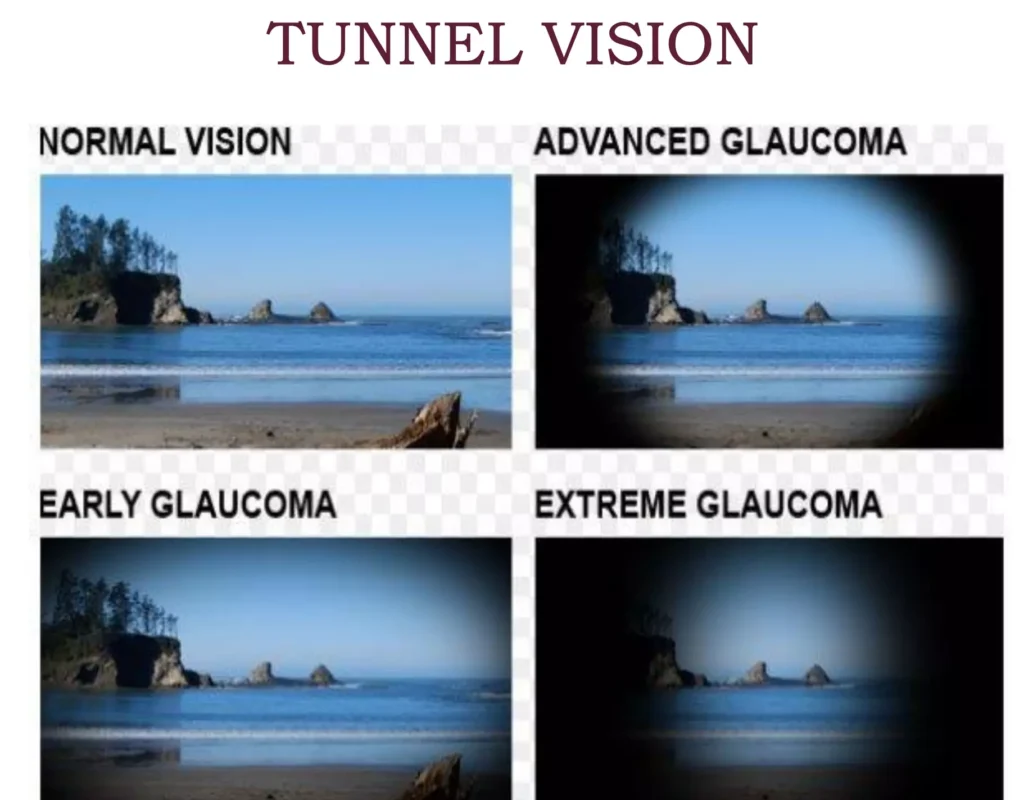
- Loss of Peripheral vision
- Reduced visual acquity at night.
- Corneal edema
- Visual field deficit.
Investigations for primary glaucoma include:
- Tonometry: To measure intraocular pressure (IOP). In glaucoma, IOP may remain permanently high in the late stages and fluctuating in the early stages.
- Gonioscopy: To assess the angle of the anterior chamber. Narrowing of the angle may be observed in glaucoma.
- Fundus examination: Done with the use of ophthalmoscopy and a slit lamp biomicroscope to look for disc changes.
- Perimetry: To assess changes in the visual field.
Treatment options for primary glaucoma include:
Medical treatment: This is the first choice for open-angle glaucoma.
- Topical beta blockers: These drugs lower the production of aqueous fluid, thereby reducing IOP. Examples include Timolol mealate: (2.5-5 mg B.D), Betaxolol 25mg B.D, Levabunolol 2.5-5% B.D it has a longer effect
- Dorzolamide(2%): It lowers IOP by decreasing the production of aqueous fluid.
- Latanoprost(0.5): It decreases the flow of aqueous fluid.
- Pilocarpine: It contracts the ciliary muscle and opens the trabecular meshwork, allowing increased outflow of aqueous humor.
- Adrenergic group: Drugs like epinephrine hydrochloride decrease aqueous production through vasoconstriction.
Surgical treatment: Surgery is considered when there is a failure to respond to maximal medical therapy.
- Laser therapy: Laser trabeculoplasty (ALT) may be performed if the patient does not respond to medical treatment
- Filtering surgery: Trabeculectomy is a surgical procedure that creates an opening in the white of the eye to allow fluid to leave the eye.
- Drainage tubes: Small tubes may be inserted in the eye to drain excess fluid and lower IOP.
- Minimally invasive glaucoma surgery (MIGS): These procedures have less risk and require less postoperative care compared to traditional surgeries
PRIMARY ANGLE CLOSURE GLAUCOMA
Primary angle closure glaucoma, also known as primary closed angle glaucoma, narrow angle glaucoma, pupil block glaucoma, or acute congestive glaucoma, is a type of glaucoma characterized by a rapid onset and is considered an ophthalmic emergency. If not treated promptly, it can lead to blindness within a few days.
It is the type of glaucoma where the IOP is raised due to narrowing of the angle of anterior chamber it is more common in female with nervous personality.
Causes and Risk Factors:
- Abnormality of the structures in front of the eyes, resulting in obstruction to the outflow of aqueous humor.
- Narrow angle glaucoma due to factors such as a large-sized lens, bigger-sized ciliary body, smaller diameter of the cornea, or a small eyeball.
- Anteriorly placed iris.
- Hypermetropic eyes (related to far-sightedness).
- Precipitating factors: Dim light, Emotional stress/anxiety and Mydriatic drugs like ( atropine, tropicamide, cyclopentolate)
Clinical Features:
The course of the disease can be divided into two types: subacute glaucoma and acute congestive glaucoma.
Subacute Glaucoma:
Gradual onset with transient attacks of blurring vision and mild headache.
- Temporary increase in intraocular pressure (IOP) during the attacks, which last for a few seconds to minutes or hours.
- Dilated pupils, shallow anterior chamber, and mild corneal edema during the attacks.
- Symptoms resolve on their own.
Acute Congestive Glaucoma:
Abrupt increase in IOP due to sudden closure of the anterior chamber.
- Symptoms include severe eye pain, defective vision, redness of the eye, photophobia, lacrimation, nausea, and vomiting.
- Dilated pupils that are non-reactive to light and edematous optic disc.
Treatment Options:
The main goals of treatment for primary angle closure glaucoma are to prevent progression of angle closure and to control IOP.
Laser Iridotomy:
- The conventional treatment for primary angle closure glaucoma is laser iridotomy (LI).
- Laser iridotomy eliminates pupillary block and widens the angles by reducing the pressure differential between the anterior and posterior chambers.
- Stepped-up standard glaucoma medications may be added if IOP remains high despite laser iridotomy .
“Stepped-up standard glaucoma medications” refers to the progression of treatment options for glaucoma patients that involves starting with the most commonly prescribed and effective medications and then adjusting or adding additional medications if necessary to achieve the desired reduction in intraocular pressure (IOP) and prevent further progression of the disease.
The following are some of the commonly used stepped-up standard glaucoma medications:
- Prostaglandin analogs: Prostaglandin analogs, such as latanoprost (Xalatan), are often the first-line treatment choice for glaucoma. They are prescribed as eye drops and work by increasing the outflow of fluid from the eye, thereby reducing IOP.
- Beta blockers: Beta blockers, such as timolol (Timoptic) and levobunolol (Betagan), are another class of medications used to treat glaucoma. They reduce IOP by decreasing the production of fluid in the eye. Beta blockers can be nonselective or selective, and they may have side effects such as burning/stinging, blurred vision, and systemic effects like decreased heart rate and bronchospasm.
- Miotics: Miotics, such as pilocarpine (Isopto Carpine), work by constricting the pupil and increasing the outflow of fluid from the eye. They can be used as eye drops and may cause side effects such as blurred vision, sweating, and gastrointestinal symptoms.
- Carbonic anhydrase inhibitors: Carbonic anhydrase inhibitors, such as dorzolamide (Trusopt) and brinzolamide (Azopt), reduce IOP by decreasing the production of fluid in the eye. They are available as eye drops and may cause side effects such as burning, bitter taste, and ocular allergies.
- Sympathomimetics: Sympathomimetics, such as dipivefrin (Propine), work by reducing IOP through various mechanisms, including increasing the outflow of fluid and decreasing its production. They are available as eye drops and may cause side effects such as burning, increased blood pressure, and tremor.
- Alpha-2 adrenergic agonists: Alpha-2 adrenergic agonists, such as brimonidine (Alphagan) and apraclonidine (Iopidine), reduce IOP by decreasing the production of fluid and increasing its outflow. They are available as eye drops and may cause side effects such as conjunctival blanching, headache, and drowsiness.
Surgical Options:
- Trabeculectomy: Effective for primary angle closure glaucoma, but associated with a higher risk of complications such as filtration failure, shallow anterior chamber, and malignant glaucoma/aqueous misdirection.
- Lens Extraction: Lens extraction, either alone or in combination with trabeculectomy, has been shown to significantly increase anterior chamber depth and widen the drainage angle, leading to IOP reduction.
- Clear lens extraction (CLE) has been found to be highly effective in reducing IOP and improving quality of life in angle-closure glaucoma patients.
- Phacoemulsification alone or combined with trabeculectomy may be considered depending on the patient’s condition.

CHRONIC CLOSED-ANGLE GLAUCOMA
Chronic closed-angle glaucoma is a condition characterized by elevated intraocular pressure (IOP) and damage to the optic nerve.
When this angle is narrowed or closed, pressure increases over time, causing damage to the optic nerve and leading to blindness. This will lead to Absolute Glaucoma.
Treatment Options for Chronic Closed-Angle Glaucoma:
Medical Therapy; This is used to lower the IOP in emergency cases as a temporary measure before surgery
This includes:
- Parenteral analgesic to relieve pain
- IV Mannitol and Acetazolamide 250mg TDS to lower IOP
- Pilocarpine eye drops (2%) instilled every 30 minutes for 2 hours later hourly
- Eye drops may include Beta blockers like Timolol mealate (5%) BD, prostaglandin analogs, alpha agonists, carbonic anhydrase inhibitors, or a combination of these medications.
- Corticosteroid eye drops to reduce inflammation
Surgery:
- Laser Iridotomy: In chronic closed-angle glaucoma, laser iridotomy is often performed to reopen the blocked drainage angle. This procedure involves creating a small hole in the iris to allow the fluid to flow freely and reduce IOP.
- Trabeculectomy: Trabeculectomy is a surgical procedure that creates a new drainage channel to lower IOP. It involves creating a small flap in the sclera (white part of the eye) to allow the fluid to drain out.
- Glaucoma Drainage Device: In some cases, a glaucoma drainage device, also known as a tube shunt, may be implanted to help drain the excess fluid and reduce IOP.
- Cyclophotocoagulation: Cyclophotocoagulation is a laser procedure that targets the ciliary body, which produces the fluid in the eye. By reducing the production of fluid, it helps lower IO.
Absolute glaucoma
Absolute glaucoma is the final stage or end stage of all types of glaucoma, characterized by permanent vision loss or blindness due to increased intraocular pressure.
The eye has no vision, absence of pupillary light reflex and pupillary response, and has a stony appearance. Severe pain is present in the eye. The primary focus of treatment for absolute glaucoma is to reduce pain and keep the eye comfortable.
The treatment of absolute glaucoma is a destructive procedure like
Risk factors:
Include elevated intraocular pressure, IOP fluctuation, male gender, pseudoexfoliation syndrome, worsening visual fields, optic disc hemorrhage, migraine, systemic diseases (hypertension, diabetes, myopia), and low socioeconomic status.
Causes:
Absolute glaucoma can occur due to various reasons, including uncontrolled raised ocular pressure, non-compliance with glaucoma medication, trauma, intraocular surgery (especially cataract extraction), and association with certain syndromes like aniridia, Lowe syndrome, or Sturge-Weber syndrome.
Symptoms:
In the final stage of glaucoma, patients may experience severe eye pain, a stone-like appearance of the eye, tearing, photophobia, lost pupillary reflex, and no pupillary response.
In absolute glaucoma :
- The pain can be relieved by retrobulbular injection of alcohol.
- The IOP may be reduced by destroying the ciliary epithelium by cryphotocoagulation.
- If the pain is not relieved by the conservative approaches then the painful blind eye is enucleated.
SECONDARY GLAUCOMA
Secondary glaucoma is a type of glaucoma that occurs as a result of underlying diseases or conditions within the eyes.
It can be caused by various factors such as uveitis (inflammation), trauma, intraocular hemorrhage, previous surgeries, diabetes, and the use of steroid medications.
Types of Secondary Glaucoma
- Lens-induced glaucoma: This type of glaucoma occurs due to trabecular blockage caused by the lens. It can happen when the lens material clogs the trabeculae, leading to increased intraocular pressure (IOP).
- Glaucoma due to uveitis: Inflammation associated with uveitis can lead to increased IOP. The inflammatory material can clog the trabecular meshwork and cause trabeculitis, resulting in elevated pressure within the eye.
- Neurovascular glaucoma: This is a less common type of glaucoma that is difficult to treat. It is caused by proliferative diabetic retinopathy, which affects the blood flow to the eyes. Individuals with poor blood flow to the eyes are at a higher risk of developing this condition.
- Glaucoma associated with intraocular tumors: Intraocular tumors, such as retinoblastoma and malignant melanoma, can cause an increase in IOP.
- Steroid-induced glaucoma: Some individuals may develop glaucoma as a result of sensitivity to steroid medications. Sudden rises in IOP can occur, but appropriate use of steroids can help prevent this.
- Pigmentary glaucoma: This is a rare condition where pigment cells slough off from the back of the iris and float around in the aqueous humor. It can lead to increased IOP.
Treatment of secondary glaucoma depends on the underlying cause and may involve a combination of medical management, laser therapy, or surgical intervention.
Nursing care for patients with glaucoma
- Recognize and assess signs and symptoms of glaucoma.
- Monitor intraocular pressure (IOP) and optic nerve function.
- Administer prescribed medications, such as eye drops, to manage intraocular pressure.
- Educate patients about glaucoma, including risk factors, treatment options, and the importance of regular eye exams.
- Provide support and guidance on strategies to optimize eye health and prevent disease progression.
- Coordinate referrals to ophthalmologists or glaucoma specialists for further evaluation and management.
- Offer emotional support and counseling to patients adjusting to the diagnosis of glaucoma.
- Assess for gradual loss of peripheral vision.
- Monitor for increased intraocular pressure.
- Assess for blurred or hazy vision, halos around lights, vision loss, headaches, or eye strain.
- Implement measures to assist patients in managing visual limitations, such as reducing clutter, arranging furniture out of the travel path, and correcting for dim light and problems of night vision.
- Demonstrate administration of eye drops, including counting drops, adhering to the schedule, and not missing doses.
- Assist with the administration of medications as indicated, such as topical myotic drugs or other prescribed medications.
- Provide sedation and analgesics as necessary, especially during acute glaucoma attacks associated with sudden pain.
Nursing Diagnosis for Glaucoma.
Impaired Visual Sensory Perception related to increased intraocular pressure and optic nerve damage.
- Assess the patient’s visual acuity and field.
- Monitor for changes in visual perception.
- Provide education on strategies to optimize visual function.
Risk for Injury related to visual impairment and decreased peripheral vision.
- Assess the patient’s mobility and safety awareness.
- Implement measures to reduce environmental hazards.
- Educate the patient on fall prevention strategies.
Anxiety related to the fear of vision loss and the chronic nature of the disease as evidenced by patient asking alot of questions about the diagnosis.
- Assess the patient’s anxiety level and coping mechanisms.
- Provide emotional support and counseling.
- Teach relaxation techniques to help manage anxiety.
Deficient Knowledge related to glaucoma diagnosis and treatment as evidenced by the patient asking alot of questions.
- Assess the patient’s understanding of glaucoma.
- Provide education on the disease process, treatment options, and the importance of regular eye exams.
- Encourage the patient to ask questions and clarify any misconceptions.
Noncompliance related to difficulty adhering to medication regimen as evidenced by the patient verbalizing problems in eye drop self administration.
- Assess the patient’s understanding of the prescribed medications.
- Identify barriers to medication adherence.
- Provide education on the importance of medication compliance and strategies to improve adherence.
Disturbed Body Image related to changes in visual appearance and functional limitations as evidenced by the patient wearing black glasses.
- Assess the patient’s perception of body image and self-esteem.
- Provide emotional support and counseling.
- Encourage the patient to express feelings and concerns about body image changes.

Preventive measures for glaucoma
- Regular Eye Exams: Schedule regular comprehensive eye exams, especially if you are at a higher risk for glaucoma. Early detection and treatment can help prevent vision loss.
- Medication Adherence: If you have been diagnosed with glaucoma or are at risk, it is important to take prescribed medications as directed by your healthcare provider. These medications help in reducing intraocular pressure and preventing further damage to the optic nerve.
- Know Your Risk Factors: Be aware of the risk factors associated with glaucoma, such as age, family history, race (African Americans are at higher risk), and certain medical conditions like diabetes. If you fall into any high-risk category, it is important to be vigilant and take appropriate preventive measures.
- Lifestyle Modifications:
- Healthy Diet: Include a diet rich in leafy green vegetables, colored fruits, berries, and vegetables. These foods contain vitamins and minerals that are beneficial for eye health.
- Regular Exercise: Engage in regular exercise at a moderate pace, as it can help lower eye pressure and improve overall health. However, avoid intense exercises that significantly raise your heart rate, as they may increase eye pressure.
- Eye Protection: Wear protective eyewear during sports or activities that may pose a risk of eye injury.
- Avoid Head-down Positions: If you have glaucoma or are at high risk, avoid prolonged head-down positions, as they can significantly raise eye pressure.
- Sleep Position: Avoid sleeping with your eye against the pillow or on your arm, especially if you have obstructive sleep apnea (OSA), as it may increase the risk or severity of glaucoma.
- Sun Protection: Wear quality polarized sunglasses and a hat to protect your eyes from harmful UV rays.
- Oral Hygiene: Maintain good oral hygiene by brushing and flossing your teeth regularly, as there may be a link between gum disease and optic nerve damage in glaucoma.
- Blood Pressure Management: Inform your ophthalmologist about your blood pressure medication, as low blood pressure during sleep can worsen glaucoma damage.
Complications of glaucoma
- Vision Loss: Glaucoma can cause gradual and irreversible vision loss, starting with peripheral vision and eventually affecting central vision.
- Blindness: If left untreated or poorly managed, glaucoma can lead to permanent blindness. It is one of the leading causes of irreversible blindness worldwide.
- Optic Nerve Damage: Glaucoma causes damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. This damage can result in permanent vision impairment.
- Increased Intraocular Pressure: Elevated intraocular pressure can cause discomfort, pain, and headaches. It can also lead to corneal damage and changes in the shape of the eye.
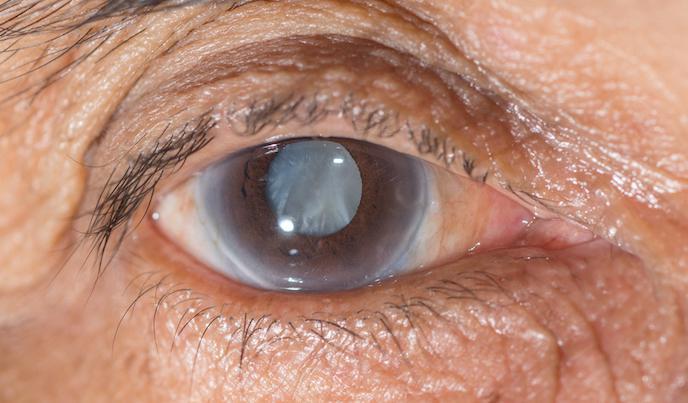
- Secondary Cataracts: Some types of glaucoma, such as angle-closure glaucoma, can lead to the development of secondary cataracts.
- Macular Edema: In some cases, glaucoma can lead to macular edema, which is the accumulation of fluid in the macula, the central part of the retina. This can cause blurred or distorted central vision.
- Visual Field Defects: Glaucoma can result in the loss of peripheral vision, leading to blind spots and difficulty with activities such as driving or navigating crowded spaces.
- Corneal Damage: Increased intraocular pressure can cause corneal thinning and damage, leading to vision disturbances and discomfort.
- Emotional and Psychological Impact: Glaucoma can have a significant emotional and psychological impact on individuals, causing anxiety, depression, and a decreased quality of life.

The os simplified and easily red
Thank you for the wonderful work done by providing us with the Note
Kindly we request you to produce books for easy accessibility
To put in the library for students to study