Table of Contents
ToggleCongenital Toxoplasmosis
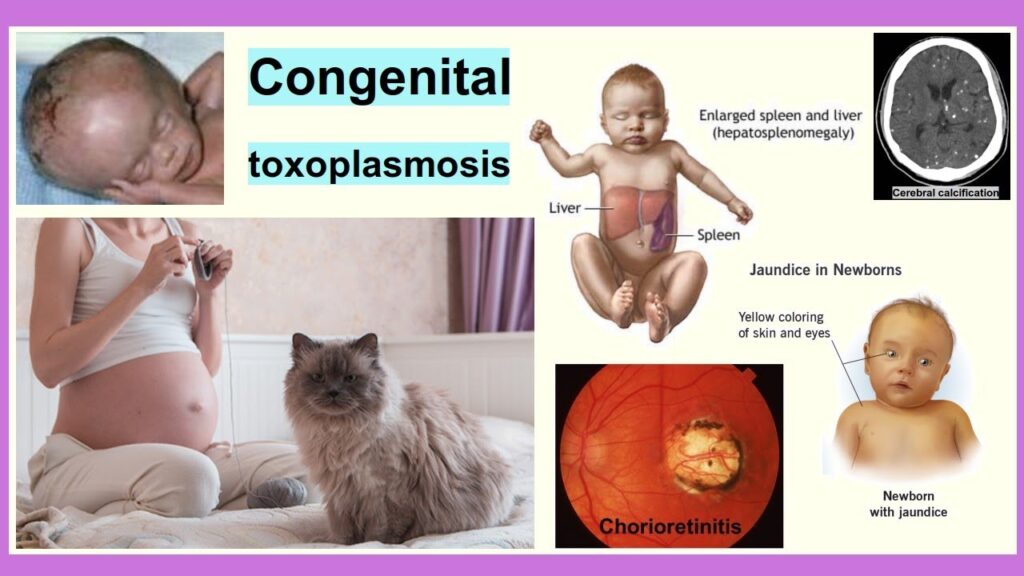
Congenital toxoplasmosis is a disease that occurs in fetuses or new-borns infected with Toxoplasma gondii, a protozoan parasite, which is transmitted from mother to fetus.
- It can cause miscarriage or stillbirth.
- It can also cause serious and progressive visual, hearing, motor, cognitive, and other problems in a child.
- In healthy people it causes asymptomatic infection however in immunocomprised people and pregnant mothers it may cause serious infection
- At birth there is no obvious damage but develops later in early childhood or adult hood.
- The severity of the disease depends on the gestational age at transmission
Causes of Toxoplasmosis
Toxoplasmosis is caused by Toxoplasma gondii.
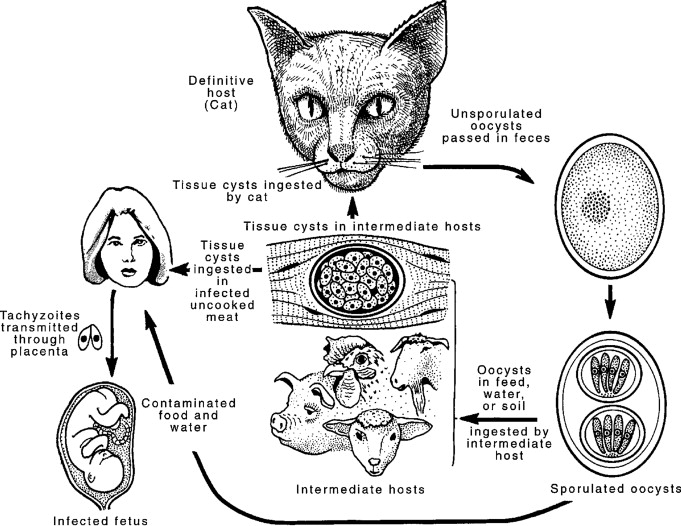
It which burrows in wild and domestic cats through which their infectious forms, oocysts, get excreted in their feces.
Mode of Transmission
There are different ways for a person to contract toxoplasmosis:
Vertical transmission.
- Congenital transmission. A patient with toxoplasmosis can infect the unborn child. The patient may not present symptoms, but the unborn baby can have serious complications which can affect the nervous system and eyesight
Horizontal Transmission
- Foodborne. Humans can contract toxoplasmosis by eating undercooked meat containing infective tissue forms of the parasite T. gondii. It can also be transferred to food and therefore to humans through contaminated utensils and cutting boards. Also, drinking unpasteurized goat’s milk can cause toxoplasmosis infection.
- Zoonotic transmission. Zoonotic transmission refers to animal to human transfer of the infection. Cats play a major role in this type of transmission. Cats serve as hosts to T. gondii. They shed their oocysts through their feces, and these oocysts are microscopic and can be transferred to humans through accidental ingestion by not washing hands after cleaning the cat’s litter box, drinking water infected with oocysts, or not using gloves when gardening.
- Rare means of transmission. In very rare occasions, toxoplasmosis can be transmitted through organ donation and transplant, as well as in blood transfusion.
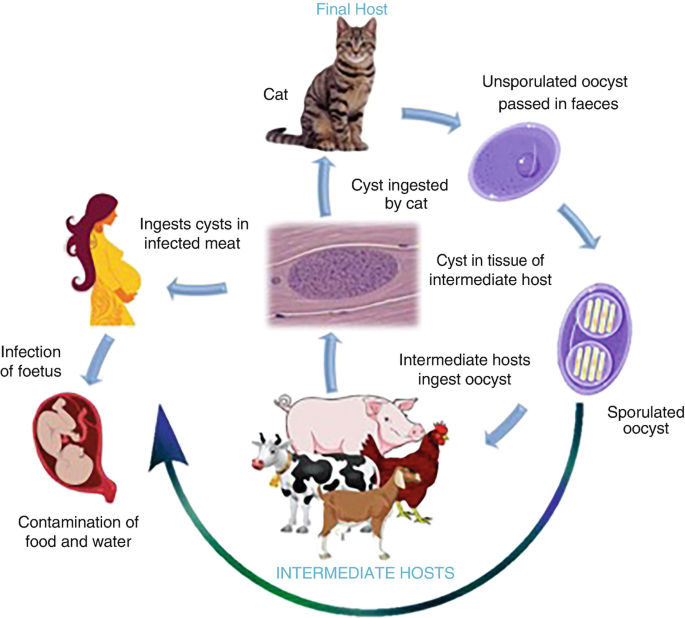
LIFE CYCLE OF TOXOPLASMA GONDII
- It is an ubiquitous obligate intracellular protozoa that infects animals and humans
- It has intestinal and extra intestinal cycles in cats and only extra intestinal cycles in hosts.
- It exists in 3 infective forms; Bradyzoites, Tachyzoites and Sporozoites
Bradyzoites: – slowly multiplying contained in tissue cysts usually localized to skeletal and cardiac muscles, Eyes and the brain. These live in their host cells for months to years.
- Once ingested, gastric enzymes degrade the cyst wall liberating viable Bradyzoites
Tachyzoites: – rapidly dividing organisms found in the tissue in acute phases of the infection. They localize in neural and muscle tissues and develop into tissue cysts. They are responsible for tissue destruction. Multiplication continues till either the cyst formation or host cell destruction occurs. After cell death, the free Tachyzoites invade other cells and resume rapid multiplication
Sporozoites: – result from the parasite’s sexual cycle which takes place in the cat’s intestines. When eliminated by the cat these cysts first undergo sporulation to become infectious (2-3 days) therefore the risk of spread is minimized if cat litter is cleaned daily.
Pathogenesis for vertical transmission
- Acute infection with Tachyzoites in blood during pregnancy increase the risk of transplacental infections
- The Tachyzoites colonize in the placenta and cross the barrier to reach the fetus.
- The frequency of transmission of the Tachyzoites to the fetus is related to the gestational age where the transmission rate is low in the first trimester and highest in the third trimester however the disease is more severe if the infection is acquired in early pregnancy.
Clinical Features
- Premature birth — as many as half of infants with congenital toxoplasmosis are born prematurely
- Abnormally low birth weight
- Eye damage (Blurred vision, Photophobia, Epiphora)
- Intrauterine growth restriction
- Low-grade fever
- Vomiting
- Jaundice, yellowing of the skin and whites of the eyes
- Diarrhea
- Anemia
- Hearing loss
- Motor and developmental delays
- Hydrocephalus
- Difficulty feeding
- Swollen lymph nodes (Lympadenopathy; painless, firm and confined to one chain)
- Enlarged liver and spleen
- Macrocephaly, an abnormally large head
- Microcephaly, an abnormally small head
- Rash (usually Maculopapular that spares hands and soles)
- Bulging fontanelle
- Abnormal muscle tone
- Seizures
- Motor and developmental delays
- Hydrocephalus, a buildup of fluid in the skull
- Intracranial calcifications, evidence of areas of damage to the brain caused by the parasites
Diagnosis of Toxoplasmosis
- History taking
- Physical examination
Investigations
- Serologic testing – a blood test to measure the level of immunoglobulin G (IgG) can tell if a person has been infected. Immunoglobulin M (IgM) may also be tested if the time of infection needs to be determined. This is mostly appropriate to pregnant women as the time of infection is necessary to give the clinician a better understanding of the possible effects of toxoplasmosis to the unborn baby.
- Culture – tissue sample like cerebrospinal fluid may be used to observe the parasite through culture. However, this method is not commonly done as the sample is not easily obtained.
- Amniotic fluid testing – to check for the presence of the parasite’s DNA. This is particularly helpful in pregnant women with toxoplasmosis.
- Brain biopsy – if the individual is not responding to treatment, a brain biopsy is performed to check for toxoplasmosis cysts.
- LFT’s will be elevated(ALT, AST)
- CBC: will show Eosinophilia.
- RFT’s: elevated blood urea, creatinine.
- Electrolytes: elaveted pottasium, calcium and sodium.
Imaging
- ultrasound can be performed in pregnant women. It will not definitely diagnose toxoplasmosis, but it will give clinicians a visual of the baby’s brain for the presence of hydrocephalus. If the fetus is between 20 – 24 weeks of gestation, scan will show hepatosplenomegaly, intrahepatic calcification.
- Magnetic Resonance Imaging (MRI) may also be performed to get images of the brain if nervous system involvement is suspected.
- CT Scan will show intracranial calcifications, ventriculomegaly, hydrocephalus.
Treatment and Management
- Usually managed as outpatient cases in patients who are immune competent or those without vial organ damage
- Limitation of activity in patients with toxoplasmosis depends on the severity of the disease and organ system involved
- Patient education on prevention methods, effects of T. gondii on the fetus to pregnant mothers.
- Follow-up every 2 weeks till the patient is stable then monthly during the therapy. Perform CBC weekly for the first month then every 2 weeks perform LFTs and RFTs monthly.
- Administer drugs such as
- Pyrimethamine. This drug is typically used for malaria. It is a folic acid antagonist, and it prevents the body from absorbing folate.
- Sulfadiazine. It is commonly prescribed together with pyrimethamine to treat toxoplasmosis.
- Sulfadiazine is active against Tachyzoites however adjust doses it in renal insufficiency because it is only excreted by the kidneys, also avoids in G6PD because it causes haemolysis. It can be substituted with Clindamycin

- Dose: 1-1.5g QID for 3-4 weeks or 100mg/kg/day in 2DD
- Pyrimethamine when given in high doses may cause haemolytic anaemia therefore monitor closely
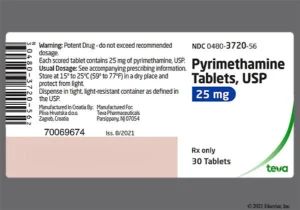
- Dose: 50-75mg OD PO for 2-3weeks then 25-37.5mg OD PO for 4-5 weeks
- Corticosteroids; esp. with elevated CSF protein and vision threatening Chorioretinitis administer Predinsolone 1mg/kg/day till they resolve
- Trimethoprim Sulphamethoxazole: 40mg/kg/day in 2DD
- Dapsone(in combination with Pyrimethamine): 100mg/kg/day PO for 1-3weeks
- Clindamycin (in combination with Pyrimethamine for sulfadiazine sensitive patients):10-12mg/kg BD PO for 4 weeks
- Folic acid: to prevent hematological effects associated with bone marrow suppression and also reduce effects of Pyrimethamine
- Dose: 10mg 3times per week
Prevention
- This is particularly important to pregnant mothers and immunocompromised
- Avoid consuming raw or half cooked meat, unpasteurized milk or uncooked eggs
- Wash hands after touching raw meat, gardening or having contact with soil
- Avoid contact with cat feces
- Disinfect litter for 5 minutes with boiling water
- Cook food thoroughly
- Wash and peel all fruits and vegetables
- Wash hands frequently and any cutting boards used to prepare meat, fruits or vegetables
- Wear gloves when gardening or avoid gardening altogether to avoid contact with soil that may contain cat waste
- Avoid cleaning the litter box
Complications
- Intrauterine growth restriction
- Chorioretinitis (Blurred vision, Photophobia, Epiphora)
- Cerebral calcifications
- T. Encephalitis
- Mental retardation
- Seizures
Nursing Diagnosis for Toxoplasmosis
- Hyperthermia related to parasitic infection secondary to toxoplasmosis, as evidenced by temperature of 38.5 degrees Celsius, rapid and shallow breathing, flushed skin, profuse sweating, and weak pulse.
- Deficient Knowledge related to new diagnosis of toxoplasmosis as evidenced by patient’s verbalization of “I want to know more about my condition, cause and treatment”

Pathophysiology of congenital toxoplasmosis
good notes pliz
Best research site for nurses to improve on professional skills and knowledge
Thanx alot for that research continue with the same spirit
Thanks for the research
Thnx for the notes,,
I like it
Very nice notes thank you