Table of Contents
ToggleEATING DISORDERS
Eating disorders are conditions characterized by an extreme disturbance in eating related behaviour.
OR
Eating disorders are moderate to severe illnesses that are characterized by disturbances in thinking and behaviour around food, eating and body weight or shape.
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, American Psychiatric Association,
2013) outlines six types of disordered eating patterns but four types are commonly diagnosed:
- Anorexia Nervosa (AN)
- Bulimia Nervosa (BN)
- Binge Eating Disorder (BED)
- Avoidant Restrictive Food Intake Disorder (ARFID)
The rest of the two types are;
5. Other Specified Feeding or Eating Disorders (OSFED)
OSFED is also a moderate to severe illness and may include eating disorders of clinical significance that do not meet the criteria for AN or BN. OSFED and USFED may be as severe as AN or BN.
6. Unspecified Feeding or Eating Disorders (USFED)
USFED applies to where behaviours cause significant distress or impairment of functioning, but do
not meet the full criteria of any of the other feeding or eating disorder criteria.
ANOREXIA NERVOSA
Anorexia nervosa (AN) is a severe eating disorder characterized by a distorted body image that leads to restricted eating, over exercise and other behaviors that prevents a person from gaining weight or
maintaining a healthy weight.
OR
Anorexia Nervosa is defined as self-induced starvation resulting from fear of gaining weight rather than from true loss of appetite.
Person with anorexia nervosa continues to feel hunger but persists in denying himself or her self food.
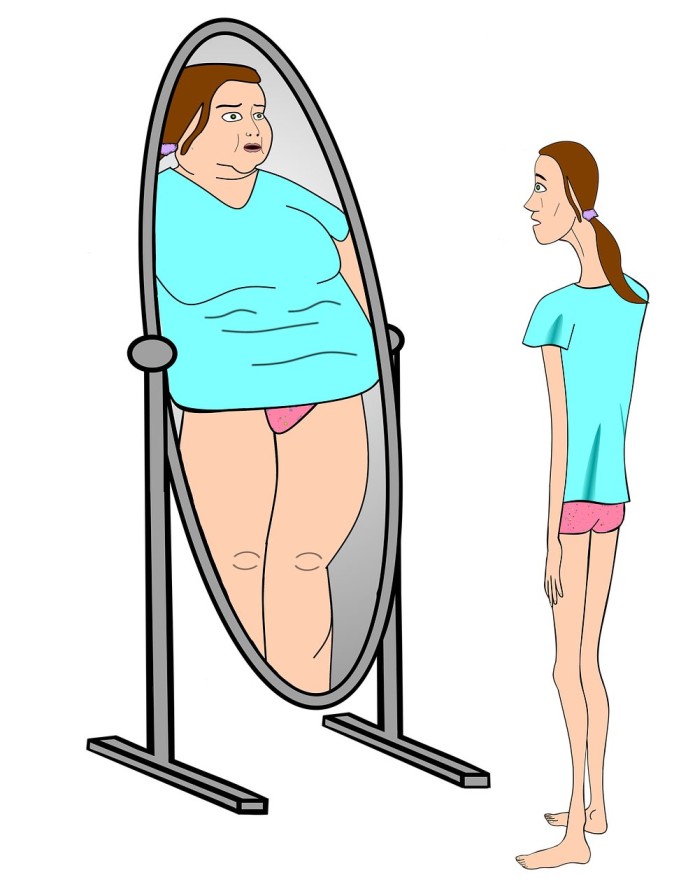
Children and teens with anorexia have a distorted body image. People with anorexia view themselves as heavy, even when they are dangerously skinny. They are obsessed with being thin and refuse to maintain even a minimally normal weight.
Signs and Symptoms of Anorexia Nervosa
- Refusal to maintain a minimum normal body weight.
- Is intensely afraid of gaining weight.
- Significant disturbance in the perception of the shape or size of his or her body.(distorted image)
- Dieting even when one is thin or emaciated
- The individual maintains a body weight that is below a minimally normal level for age and weight.
- They exclude from their diet what they perceive to be highly caloric foods. ie they restrict diet.
- Purging i.e. self-induced vomiting or misuse of laxatives, diuretics.
- There is excessive exercise to reduce weight.
- Reduced total food intake
- Intense fear of becoming fat or obese.
- Strange eating habits, very picky.
- Infrequent menstruation or Amenorrhea due to reduced estrogen and loss of weight
- Oligomenorrhoea or failure to reach menarche.
- Loss of sexual interest
- Anxiety, depression, perfectionism(hold themselves to impossibly high standards)
Possible complications of Anorexia Nervosa
Anorexia nervosa is fatal in about 10% of cases. Most common death from anorexia nervosa is due to, cardiac arrest, electrolyte imbalance and suicide.
- Heart muscle damage that can occur as a result of malnutrition or repeated vomiting may be life threatening.
- Arrhythmias (a fast, slow, or irregular heartbeat)
- Hypotension (low blood pressure)
- Electrolyte imbalance.
- Anaemia (low RBC’s) and Leukopenia(low WBC’s)
- GIT disturbances.
- Dehydration
- Refeeding Syndrome,
Refeeding Syndrome “is potentially a fatal condition defined by severe electrolyte and fluid shifts as a result of a rapid reintroduction of nutrition after a period of inadequate nutritional intake
Management or Treating Anorexia Nervosa
- The major aim of treatment is to bring the young person back to normal weight and eating habits.
- Hospitalization, sometimes for weeks, may be necessary. In cases of extreme or life-threatening malnutrition, tube or intravenous feeding may be required.
Nursing care
- Short term management is focused on ensuring weight gain and correcting nutritional deficiencies. maintaining normal weight and preventing relapses
- provide a balanced diet of at least 3000 calories in 24 hours
- a nurse should always supervise the patient during meals
- patient should be under complete bed rest initially under nurses observation so as to achieve a weight gain goal of 0.5 to 1kg per week
- control vomiting by making the bathroom inaccessible 2 hours after food
- in extreme cases when the patient refuses to comply with treatment and eating, gavage feeding may need to be instituted
- weight should be checked regularly and plotted on a weight chart
- maintain a strict intake and output chart
- monitor skin status and oral mucous membrane for signs of dehydration
- encourage patient to verbalise feelings of fear and anxiety related to the achievement
- encourage family to participate in education regarding patients disorder
- avoid discussions that focus on food and weight
Long-term treatment addressing psychological issues include:
- antidepressant medication
- Neuroleptics
- appetite stimulants
- behavioral therapy
- individual therapy
- cognitive behavioural therapy
- family therapy
- psychotherapy
- support groups
BULIMIA NERVOSA
Bulimia nervosa, or bulimia, is a type of eating disorder in which a person engages in episodes of bingeing—during which he or she eats a large amount of food—and then purges, or tries to get rid of the extra calories.
OR
Bulimia nervosa is a syndrome of episodes of binge eating followed by self-induced vomiting or purge behaviour accompanied by an excessive pre occupation with weight and body shape.
Young people with bulimia try to prevent weight gain by inducing vomiting or using laxatives, diet pills, diuretics, or enemas. After purging the food, they feel relieved. Binge eating is often done in private. Because most people with bulimia are of average weight or even slightly overweight, it may not be readily apparent to others that something is wrong.
The condition often begins in the late teens or early adulthood and is diagnosed mostly in women. People with bulimia may have other mental health issues, including depression, anxiety, drug or alcohol abuse, and self-injurious behaviors.
Doctors make a diagnosis of bulimia after a person has two or more episodes per week for at least three months. People with bulimia usually fluctuate within a normal weight range, although they may be overweight, too. As many as one out of every 25 females will have bulimia in their lifetime.
Binge is eating in a discrete period of time an amount of food that is definitely larger than most individuals would eat under similar circumstances.

Signs and Symptoms of Bulimia Nervosa
- The individual is typically ashamed of his or her eating problem.
- Persistent heart burn and sore throat.
- Abdominal and epigastric pain.
- They tend to conceal their symptoms, It occurs in secrecy
- Food is consumed rapidly
- Binge eating continues until the individual is uncomfortable or even painfully full.
- The binge eating is usually triggered by low mood, interpersonal stressors, intense hunger
following dietary restraint. - Loss of self control, Difficult in resisting binge eating or difficult in stopping it.
- Employs compensatory technique for example induce vomiting after binge eating.
- They place emphasis on body shape and weight in their self evaluation.
- Have fear in losing weight.
- May be overweight or underweight
- Low self esteem
- Increased frequency of anxiety for example fear of social situation
- Fluid and electrolyte imbalance due to purging
- Menstrual irregularity or amenorrhea may occur
- Rectal prolapse
- Increased dental caries
- Scarring of knuckles from using fingers to induce vomiting.
Management or Treating Bulimia Nervosa
Treatment aims to break the binge-and-purge cycle. Treatments may include the following:
Nursing care
- engage patient in therapeutic alliance to obtain commitment to treatment
- establish contract with the patient that specifies amount and type of food she must eat at each meal
- set a time limit for each meal
- identify patients elimination patterns
- encourage the patient to recognize and verbalize her feelings about her eating behavior
- explain the risks of laxative, emetic and diuretic abuse
- assess and monitor patients suicide potential
Other treatment modalities
- antidepressants medication
- behavior modification
- individual, family, or group therapy
- nutritional counseling
- self help groups
Complications of Bulimia Nervosa
- Stomach acids from chronic vomiting can cause,
- damage to tooth enamel,
- inflammation of the esophagus,
- swelling of the salivary glands in the cheeks,
- low potassium which can lead to abnormal heart rhythms.
BINGE EATING DISORDER
Binge eating is similar to bulimia.
Binge eating refers to chronic, out-of-control eating of large amounts of food in a short time, even to the point of discomfort without purging the food through vomiting or other means.
People with binge eating disorder eat unusually large amounts of food often and in secret but do not attempt to get rid of calories once the food is consumed. People with the condition may be embarrassed or feel guilty about binge eating, but they feel such a compulsion that they cannot stop.
These people can be of average weight, overweight, or obese. They may also have other mental health disorders, such as depression. Many binge eaters have trouble coping with anger, sadness, boredom, worry, and stress.
Binge eating disorder often has no physical symptoms, but it has psychological symptoms that may or may not be apparent to others, such as depression, anxiety, or shame or guilt over the amount of food eaten. Frequent dieting without weight loss is another symptom.
The excess weight caused by binge eating puts the child at risk of these health problems:
- heart disease
- high blood pressure
- high cholesterol
- type 2 diabetes
Treatments include the following: Refer to General Management,
- behavioral therapy
- medications, including antidepressants
- psychotherapy
AVOIDANT/RESTRICTIVE FOOD INTAKE DISORDER
Avoidant/restrictive food intake disorder, is an eating disorder where a person is unable to or refuses to eat certain foods based on texture, color, taste, temperature, or aroma.
The condition can lead to weight loss, inadequate growth, nutritional deficiencies, and impaired psychosocial functioning, such as an inability to eat with others. Unlike anorexia nervosa, there are not weight or shape concerns or intentional efforts to lose weight.
For instance, a child may consume only a very narrow range of foods and refuse even those foods if they appear new or different. This type of eating disorder commonly develops in childhood and can affect adults as well.
Assessment/Screening for an Eating Disorder
- The SCOFF Test:
Early detection in patients with unexplained weight loss improves prognosis and may be aided by use of the SCOFF questionnaire, developed by John Morgan at Leeds Partnerships NHS Foundation
Trust.
This questionnaire uses five simple screening questions and has been validated in specialist and primary care settings. It has a sensitivity of 100% and specificity of 90% for anorexia nervosa. A score of 2 or more positive answers should raise your index of suspicion of a case, highlighting the need for a comprehensive assessment for an eating disorder and
consultation with an eating disorder expert or mental health clinician.

2. SUSS (Sit up – Squat – Stand Test) for muscle strength
1. Sit-up: patient lies down flat on the floor and sits up without, if possible, using their hands
2. Squat–Stand: patient squats down and rises without, if possible, using their hands.
Scoring (for Sit-up and Squat-Stand tests separately)
| Parameter | Score |
|---|---|
| Unable | 0 |
| Able only when using hands to help | 1 |
| Able with noticeable difficulty | 2 |
| Able with no difficulty | 3 |
A Sit up – Squat – Stand(SUSS) score ≤ 2 indicates a RED FLAG.
Anorexia Nervosa (AN) has the HIGHEST MORTALITY rate of ALL mental health illnesses
Patients with AN are at risk of sudden death if the have the RED FLAGS below.
RED FLAGS
- SUSS score less or equal to 2
- Postural drop
- Bradycardia
- Hypothermia
- Electrolyte abnormalities
Nurses Role during assessment
- Nurses in the hospital or primary care setting are in a crucial position to screen for and detect eating disorders, hence the importance for nurses to have an awareness of the indicators for eating disorder assessment.
- supporting psychological based therapies, psycho-education regarding
effects of the eating disorder, - assessment of risk,
- promoting recovery and hope,
- involving famil and caretakers,
- observing for co-morbidities.
GENERAL MANAGEMENT OF EATING DISORDERS
Aims
- To restore the patient’s nutritional status.
- To prevent complications.
General management
- Develop a trusting relationship with the patient.
- Convey positive regard to the patient
- Stay with the patient especially at the time of meals and 1 hour after meals.
- Avoid arguing or bargaining with the patient who is resistant to treatment.
- State matters of facts which behaviours are unacceptable.
- Encourage the patient to verbalize feelings regarding role within the family and issues related to dependence.
- Help the patient to recognize ways to gain control over these problems in life.
- Help the patient to develop a realistic perception of body image and relationship with food.
- Promote feelings of control within the environment through participation and dependent
decision making. - Weigh patient daily. Always use the same weighing scale to avoid errors.
- Keep strict record of observations especially fluid input and output.
- Assess skin; motility and tugor regularly.
- Assess moistness and color of the skin and oral mucus membranes.
Behaviour modification
- Develop care plan together with the client
- Encourage the client to sign a contract is necessary
- Staff and client can agree on a system of reward.
- Individual therapy such as psychotherapy may be important. This is particularly helpful when there is underlying psychological problems contributing to the maladaptive behaviour.
- Family therapy:
> Counsel the family members. This includes educating the family about the disorder, assessing the family perception or attitudes.
> Support given to the family - Refer if necessary
- Chemotherapy: there are no specific drugs indicated for the treatment of the condition. Drugs
such as flouxetine, chlorpromazine, and lithium carbonate have been used.
Nursing Diagnoses
- Imbalanced nutrition less than body requirement related to refusal to eat or self induced vomiting as evidenced by loss of weight.
- Ineffective denial related to fear of losing or retarded ego development as evidenced by inability to admit the impact of maladaptive eating behaviours on life pattern.
- Disturbed body image related to false perception of increased body weight evidenced by patient’s verbalization of that she has global over weight.


