Table of Contents
ToggleEye Trauma (Ocular Trauma)
Eye trauma is an injury to the eye that may result in visual impairment.
Ocular trauma refers to any injury to the eye or its surrounding structures caused by physical, chemical, thermal, or radiation agents.
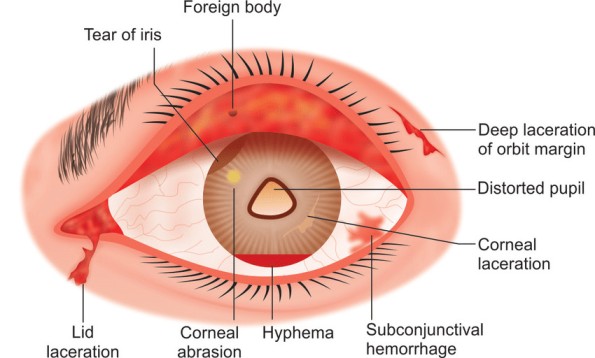
It can range from minor irritations to severe injuries affecting vision or structural integrity. Commonly injured structures include the cornea, sclera, lens, retina, vitreous, optic nerve, and orbital tissues.
Types of eye injuries
- Corneal Abrasions: A corneal abrasion is a scratch or injury to the cornea, the clear, dome-shaped surface that covers the front of the eye.
- Chemical burns: Chemical burns occur when the child gets any type of chemical in his or her eye. Chemical burns are a medical emergency, and your child should receive immediate medical care. Chemical burns can result in a loss of vision and even a loss of the eye itself, if not treated promptly and accurately. Household cleaning agents are a common cause of this type of injury.
- Hyphemia: This refers to blood in the anterior chamber of the eye. The anterior chamber is the front section of the eye’s interior where fluid flows in and out, providing nourishment to the eye and surrounding tissues. A hyphema is usually caused by an injury to the eye, and blood is seen in the eyeball. This is a medical emergency, and immediate medical care is necessary.
- Bruising or Black Eye (Ecchymosis): Ecchymosis, more commonly known as a “black eye,” usually occurs from some type of injury to the eye, causing the tissue around the eye to become bruised.
- Fractures of the orbit: The orbit is the bony structure around the eye. When one or more bones surrounding the eye are broken, the condition is called orbital fracture. An orbital fracture usually occurs after some type of injury or a strike to the face. Depending on where the fracture is located, it can be associated with severe eye injury and damage.
- Eyelid lacerations: Eyelid lacerations are cuts to the eyelid caused by injury. The physician will examine the eye closely to make sure there is no damage to the eye itself.
- Foreign bodies. Click here for more on foreign bodies of the eyes
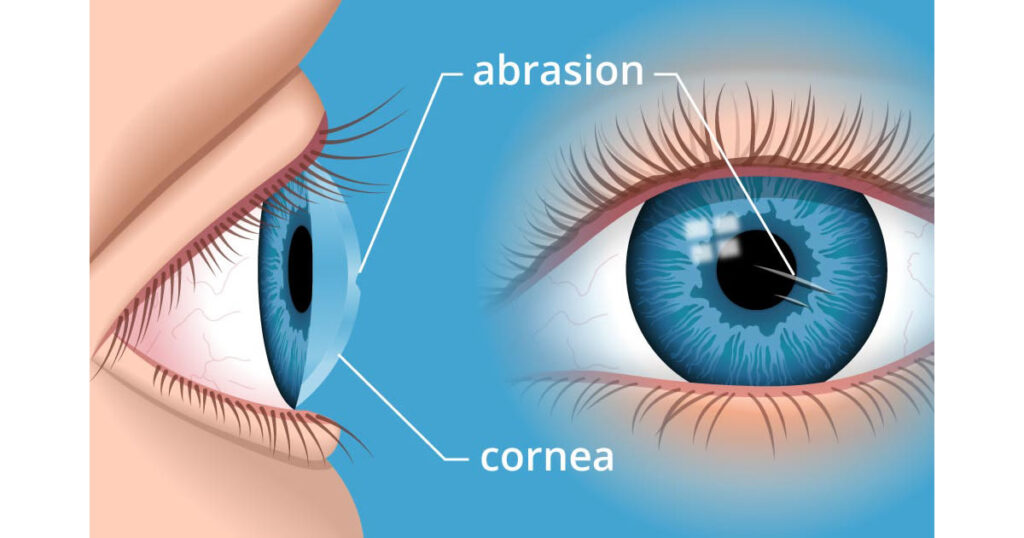
Corneal Abrasion
Corneal abrasion is defined as a superficial injury that disrupts the integrity of the corneal epithelium, typically caused by trauma, physical irritation, or external mechanical forces.
Corneal abrasion is one of the most frequent types of eye injuries and can result from various causes. Although most cases heal rapidly without long-term effects, deeper injuries can lead to complications such as facet formation or stromal scarring, which may impair vision.
Causes of Corneal Abrasion
Corneal abrasions occur when the corneal surface is physically scraped or disrupted. The following are common causes:
- Contact Lenses: Prolonged use, improper fit, or poor hygiene can irritate the cornea, causing abrasions.
- Eyelashes: Misaligned (trichiasis) or ingrown eyelashes can repeatedly rub against the cornea.
- Foreign Bodies: Small objects such as dust, dirt, sand, or metal fragments can scratch the cornea when lodged under the eyelid.
- Eye Surface Dryness: Dehydration of the corneal surface due to poor tear production or exposure to wind can predispose to abrasion.
- Chemical Irritants: Exposure to chemicals like cleaning agents or fumes may lead to epithelial disruption, increasing the risk of abrasion.
Signs and Symptoms
Corneal abrasion presents with noticeable symptoms that may significantly affect a patient’s comfort and ability to keep the eye open. These include:
- Photophobia: Sensitivity to light, causing reluctance to open the affected eye.
- Excessive Tearing: Reflex tearing occurs due to irritation and stimulation of the lacrimal glands.
- Severe Eye Pain: The cornea is highly innervated, so even small abrasions cause significant discomfort.
- Redness (Conjunctival Injection): Inflammation of the conjunctiva due to irritation or injury.
- Blurred Vision: If the abrasion affects the visual axis, it may temporarily interfere with clarity of vision.
Clinical Diagnosis
History Taking: A detailed history is essential to identify the cause and assess risk factors, such as:
- Use of contact lenses.
- Exposure to environmental irritants (e.g., debris, chemicals).
- Past history of similar episodes or underlying eye conditions.
- Any known drug allergies.
Examination:
- Record Visual Acuity: Test both eyes separately to assess the extent of visual impairment.
- Use of Slit Lamp: Employ a slit lamp for high magnification to examine the corneal surface for epithelial defects. Fluorescein staining may be applied to highlight the abrasion under cobalt blue light.
- Check for Discharge: Evaluate the eye for signs of infection, such as purulent discharge.
- Rule Out Foreign Bodies: Carefully evert the eyelids and inspect for retained debris or lashes causing irritation.
Management of Corneal Abrasion
Treatment aims to promote healing, reduce pain, and prevent infection.
Antibiotic Prophylaxis:
- Apply Chloramphenicol Eye Ointment:
- Dosage: Twice daily for 5 days.
- Purpose: Prevent bacterial infection during the healing process.
- Alternatives: Fusidic acid or fluoroquinolone eye drops for contact lens-related abrasions.
Cycloplegic Eye Drops:
- Administer Cyclopentolate (1%):
- Use one drop if the patient experiences photophobia.
- Purpose: Relieves pain by paralyzing the ciliary muscle and reducing spasm.
Pain Management:
- Prescribe oral or topical analgesics for severe discomfort.
- Avoid over-the-counter anesthetic eye drops, as they delay healing and mask symptoms.
Foreign Body Removal:
- If a foreign object is present, gently remove it using sterile instruments or irrigation.
Follow-Up:
- Patients should return for reassessment if symptoms persist beyond 48 hours or worsen, as deeper corneal injuries or infections may require additional interventions.
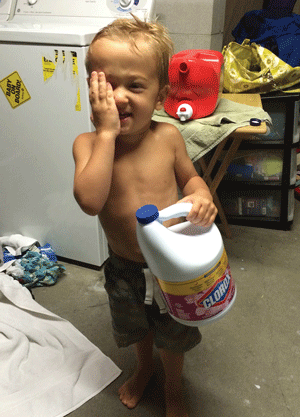
Chemical Burns
Chemical burns are serious ocular injuries caused by the exposure of the eye to harmful chemicals, which can damage the cornea, conjunctiva, and deeper ocular structures.
They are often considered ophthalmic emergencies requiring immediate attention to minimize vision loss. Depending on the type and extent of exposure, chemical burns can range from minor irritation to extensive tissue damage, including permanent scarring and blindness.
Types of Chemical Burns
Chemical burns can be broadly classified based on the nature of the chemical agent involved:
1. Alkali Burns:
- Alkalis (e.g., ammonia, lime, lye, bleach) cause more severe injuries as they penetrate tissues rapidly, leading to extensive damage.
- They saponify cell membranes and dissolve the stroma, resulting in deeper penetration.
- Common sources: Cleaning agents, fertilizers, cement, and industrial chemicals.
2. Acid Burns:
- Acids (e.g., sulfuric acid, hydrochloric acid, nitric acid) tend to cause coagulative necrosis, forming a barrier that limits further penetration.
- The damage is usually less severe than alkali burns but still can result in significant ocular injury.
- Common sources: Car batteries, glass polishing solutions, and chemical labs.
3. Irritants:
- Substances such as detergents or pepper spray may cause irritation without penetrating tissues deeply.
- The damage is commonly superficial but can be painful and temporarily debilitating.
Causes of Chemical Burns
Chemical burns are typically caused by exposure to industrial, household, or agricultural chemicals. Common sources include:
- Household Cleaners: Ammonia-based cleaners, drain cleaners, and bleach are common culprits.
- Industrial Chemicals: Cement, fertilizers, solvents, and laboratory chemicals pose occupational hazards.
- Accidents: Splashes from car batteries or exposure to acid-based solutions during industrial processes.
- Self-Harm or Assault: Intentional chemical exposure, often involving strong acids or alkalis.
- Chemical Weapons: Tear gas, pepper spray, and other irritants used in law enforcement or conflicts.
Signs and Symptoms
Chemical burns to the eye present with symptoms that depend on the type, concentration, and duration of exposure to the chemical. Common signs and symptoms include:
- Immediate Pain: Severe burning sensation and discomfort.
- Photophobia: Sensitivity to light due to corneal irritation.
- Tearing (Epiphora): Reflex tearing to flush out the chemical irritant.
- Redness (Conjunctival Injection): Intense redness due to inflammation and vascular dilation.
- Blurred Vision: Corneal edema or damage can interfere with vision clarity.
- Swelling: Swelling of the eyelids (chemosis) and conjunctiva.
- Corneal Haze or Opacity: Indicative of stromal damage, which is more common in alkali burns.
- Severe Cases: Ischemia (whitening of the conjunctiva), perforation, or loss of corneal integrity.
Management of Chemical Burns
Chemical burns require immediate intervention to prevent irreversible damage. Treatment includes the following steps:
1. Immediate Irrigation:
- Goal: Dilute and remove the chemical as quickly as possible.
- Flush the eye thoroughly with copious amounts of water, saline, or Ringer’s lactate for at least 15-30 minutes.
- Use an irrigation device (e.g., Morgan lens) if available.
- Ensure eyelids are fully everted to remove any trapped chemical or debris.
- Alkali Burns: Continue irrigation longer as they penetrate more deeply.
2. History Taking:
- Identify the chemical agent if possible (e.g., safety data sheets, packaging).
- Ask about the time of exposure and initial management attempts.
3. Assessment of pH:
- Use pH paper to assess the tear film after irrigation.
- Normal pH is 7.0-7.4; continue irrigation until pH normalizes.
4. Comprehensive Examination:
- Visual Acuity: Test both eyes separately to document baseline vision.
- Slit Lamp Examination: Assess corneal integrity, conjunctival damage, and anterior chamber involvement. Apply fluorescein dye to detect epithelial defects.
- Eyelid and Conjunctiva: Check for burns, ischemia, or necrosis.
5. Medical Management:
- Topical Antibiotics: Apply Chloramphenicol or Ciprofloxacin eye drops to prevent secondary infection.
- Cycloplegic Drops: Administer Cyclopentolate (1%) or Atropine (1%) to relieve ciliary spasm and reduce pain.
- Topical Steroids: Use cautiously to minimize inflammation but avoid long-term use as it may delay epithelial healing.
- Artificial Tears: Provide lubrication to promote epithelial regeneration and comfort.
- Ascorbic Acid and Citric Acid: Administered to promote collagen synthesis and minimize corneal ulceration.
- Tetracycline or Doxycycline: May be prescribed to inhibit collagenase activity and prevent corneal melting.
6. Surgical Management: For severe cases, surgical intervention may be required:
- Debridement: Removal of necrotic tissue to facilitate healing.
- Amniotic Membrane Grafts: Promote epithelial recovery in severe damage.
- Limbal Stem Cell Transplantation: Necessary for extensive limbal ischemia.
7. Follow-Up: Monitor the patient regularly for complications such as:
- Persistent epithelial defects.
- Corneal ulcers or thinning.
- Secondary infections or glaucoma.
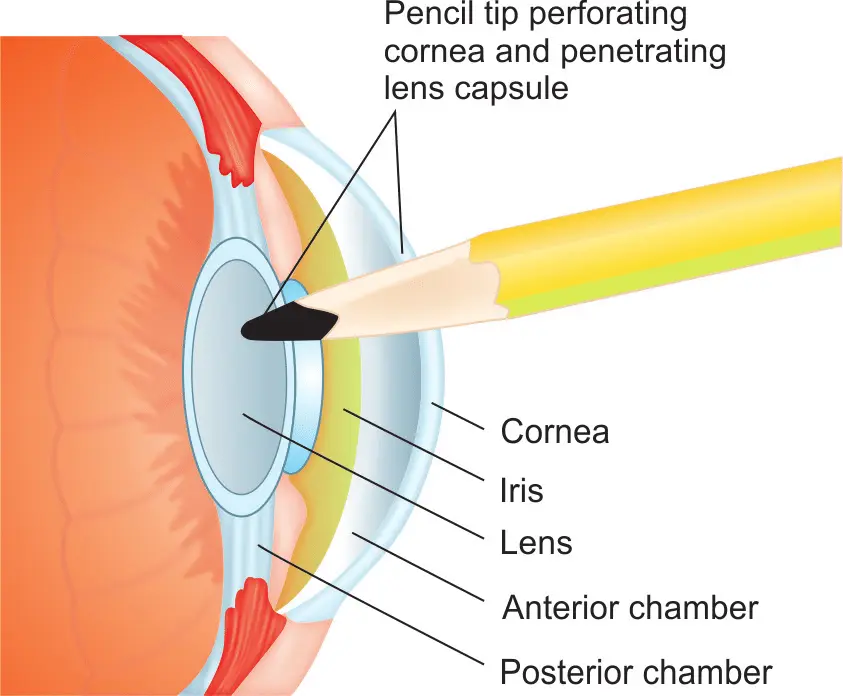
Penetrating Eye Trauma
Penetrating eye trauma is a severe ocular injury where an object pierces the eye, resulting in a full-thickness wound to the cornea, sclera, or both. This type of trauma often involves a high risk of vision loss, infection, and other complications if not treated promptly. It is a true ophthalmic emergency requiring immediate assessment and intervention.
Definition and Key Features
- Penetrating Eye Trauma: A full-thickness injury caused by a sharp or high-velocity object that creates a single-entry wound.
- Distinguished from perforating trauma, where there are both entry and exit wounds.
- Commonly associated with other ocular injuries such as lens damage, vitreous hemorrhage, or retinal detachment.
Common Causes of Penetrating Eye Trauma
Penetrating eye injuries often result from accidents, occupational hazards, or violent incidents. Typical causes include:
- Sharp Objects: Knives, scissors, needles, or glass shards.
- High-Velocity Projectiles: Metal fragments, nails, or bullets.
- Industrial or Construction Accidents: Tools like drills or saws, especially in environments without protective eyewear.
- Agricultural Work: Injuries from sharp plant material or equipment in farming.
- Assault or Violence: Stabbing or intentional harm.
- Household Incidents: Injuries caused by mishandling tools or broken objects.
Signs and Symptoms
Penetrating eye trauma presents with distinctive signs and symptoms that require urgent medical attention:
- Pain: Severe, acute pain in the affected eye.
- Vision Loss: Blurred vision, reduced visual acuity, or complete loss of vision, depending on the injury’s severity.
- Visible Wound: Laceration or puncture site visible on the cornea or sclera.
- Protrusion of Internal Structures: Uveal prolapse (iris or ciliary body visible outside the wound).
- Hyphema: Blood pooling in the anterior chamber.
- Vitreous Hemorrhage: Blood in the vitreous humor, often causing visual obscuration.
- Decreased Intraocular Pressure (IOP): Often due to globe rupture or leakage of intraocular contents.
- Signs of Foreign Body: Visible or detected foreign object within the eye or orbit.
- Eye Misalignment: Strabismus or restricted movement due to injury to extraocular muscles.
- Seidel’s Test Positive: Fluorescein dye leak indicating aqueous humor leakage.
Management of Penetrating Eye Trauma
Penetrating eye trauma is a medical emergency, requiring immediate and meticulous management to prevent complications.
1. First Aid at the Scene:
- Avoid Eye Manipulation: Do not attempt to remove the foreign object or apply pressure to the injured eye.
- Protect the Eye: Shield the eye with a rigid eye shield (e.g., a plastic cup) to prevent further injury.
- Do Not Instill Drops: Avoid placing any medications or liquids until assessed by a specialist.
- Prompt Transport: Arrange for immediate transfer to a healthcare facility specializing in eye trauma.
2. History and Examination:
History Taking:
- Mechanism of injury, time of occurrence, and presence of a foreign body.
- Assess tetanus vaccination status.
Examination:
- Record visual acuity in both eyes before intervention.
- Use a slit lamp to assess the anterior segment, if possible.
- Perform a Seidel’s test to check for aqueous leakage.
Avoid Pressure on the Eye:
- Do not press the globe while examining.
3. Imaging:
X-ray or CT Scan:
- To detect and localize intraocular or orbital foreign bodies.
- Preferred imaging modality: CT scan (without contrast) to visualize metallic or radiopaque objects.
Ultrasound (B-scan):
- For posterior segment evaluation, only if globe rupture is ruled out.
4. Medical Management:
- Antibiotics: Administer systemic antibiotics (e.g., cefazolin + ciprofloxacin) to prevent endophthalmitis.
- Tetanus Prophylaxis: Provide tetanus immunoglobulin or booster based on the patient’s vaccination history.
- Pain Relief: Systemic analgesics for pain management.
- Cycloplegics: Cyclopentolate or atropine drops to reduce ciliary spasm and pain.
- Avoid Topical Steroids: Steroids are contraindicated until epithelial healing begins.
5. Surgical Intervention: Surgical repair is essential for restoring ocular integrity and function:
- Wound Closure: Repair corneal or scleral lacerations using sutures.
- Removal of Foreign Body: Extract intraocular foreign bodies via pars plana vitrectomy or other techniques.
- Addressing Secondary Injuries: Treat associated injuries like lens damage, retinal detachment, or hemorrhage.
- Vitrectomy: Indicated in cases of vitreous hemorrhage or retinal injury.
- Enucleation (if necessary): In severe, irreparable cases, to prevent sympathetic ophthalmia or infection.
6. Postoperative Care: Close monitoring for complications:
- Endophthalmitis: Intraocular infection requiring aggressive treatment.
- Glaucoma: Secondary increase in intraocular pressure.
- Retinal Detachment: Delayed complication requiring surgical repair.
7. Follow-up: Regular follow-up to assess visual recovery and detect late sequelae.
Complications of Penetrating Eye Trauma
- Endophthalmitis: Severe, sight-threatening intraocular infection.
- Retinal Detachment: Due to posterior segment injury.
- Sympathetic Ophthalmia: Autoimmune reaction affecting the uninjured eye.
- Corneal or Scleral Scarring: Permanent scarring leading to visual impairment.
- Globe Rupture: Extensive damage causing loss of globe integrity.
- Blindness: Permanent vision loss if damage is extensive or complications arise.
Prevention
- Protective Eyewear: Essential in high-risk environments such as construction, manufacturing, or sports.
- Safety Protocols: Adherence to workplace safety guidelines to minimize risks.
- Public Awareness: Education on the importance of eye safety and early medical intervention.
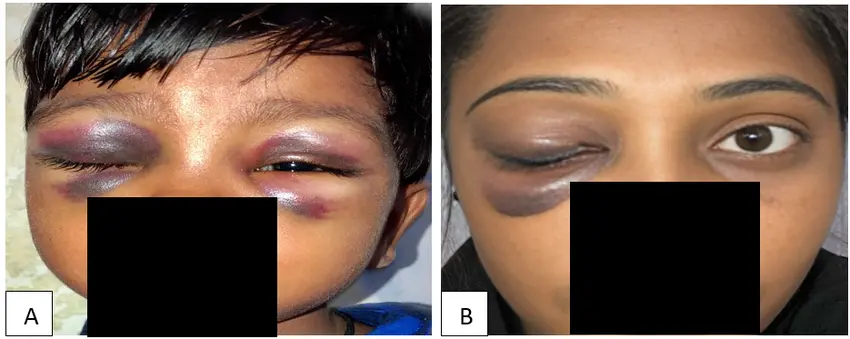
Blunt Trauma to the Eye
Blunt trauma to the eye refers to injuries caused by a non-penetrating force that impacts the eye and surrounding structures.
It is a common type of ocular trauma resulting from direct blows, sudden acceleration or deceleration forces, or high-energy impacts. These injuries can range from mild to severe, potentially leading to vision-threatening complications if not promptly addressed.
Definition and Mechanism of Injury
Blunt Trauma: Non-penetrating injuries caused by a forceful impact to the eye, leading to compression and sudden deformation of the globe.
The trauma can result in:
- Anterior Segment Injuries: Corneal abrasions, hyphema, and lens dislocation.
- Posterior Segment Injuries: Retinal detachment, choroidal rupture, and optic nerve damage.
- Orbital Injuries: Fractures or damage to adjacent structures like the eyelids or lacrimal apparatus.
Common Causes of Blunt Eye Trauma
- Sports Injuries: Injuries from balls (e.g., basketball, baseball), racquets, or physical contact in contact sports.
- Assaults: Fists, punches, or other blunt objects during physical altercations.
- Motor Vehicle Accidents: Airbag deployment, dashboard impact, or windshield collision.
- Falls: Impact with hard surfaces during slips or falls.
- Industrial Accidents: Blows from heavy machinery or tools without proper eye protection.
- Explosive Blasts: Resulting from the shockwave of an explosion.
Signs and Symptoms
Blunt trauma presents a wide variety of symptoms depending on the severity of the injury and the structures involved:
General Symptoms:
- Pain: Ranges from mild to severe, depending on the depth and location of the injury.
- Blurred Vision: Visual impairment due to corneal, lens, or retinal involvement.
- Photophobia: Sensitivity to light, especially in anterior segment injuries.
- Periorbital Swelling or Bruising: “Black eye” or ecchymosis around the orbit.
- Visible Deformity: In cases of orbital fractures or severe swelling.
Specific Clinical Signs:
- Hyphema: Accumulation of blood in the anterior chamber.
- Subconjunctival Hemorrhage: Blood pooling under the conjunctiva, giving a red appearance to the eye.
- Corneal Abrasions or Edema: Scraping or swelling of the corneal epithelium.
- Iris or Pupil Abnormalities: Traumatic mydriasis or irregularly shaped pupil due to sphincter damage.
- Retinal Detachment: Flashes, floaters, or loss of peripheral vision due to retinal separation.
- Globe Rupture: Severe globe deformity, decreased intraocular pressure (IOP), and prolapse of intraocular contents.
- Orbital Fractures: Diplopia (double vision) and enophthalmos (sunken eye) due to damage to the orbital bones.
Management of Blunt Eye Trauma
Blunt trauma to the eye can lead to complex injuries requiring prompt, systematic management.
1. Initial Assessment:
History Taking:
- Mechanism of injury, time of occurrence, use of protective eyewear, and associated symptoms.
- Tetanus vaccination history if there are lacerations.
Visual Acuity Testing:
- Assess vision in both eyes using a Snellen chart or pinhole test.
Comprehensive Examination:
- Inspect for swelling, bruising, lacerations, and deformities.
- Perform slit-lamp examination to evaluate corneal, anterior chamber, and lens injuries.
- Measure intraocular pressure (if no globe rupture is suspected).
2. Imaging:
- CT Scan (Preferred): Essential for detecting orbital fractures, intraocular foreign bodies, and posterior segment injuries.
- Ultrasound (B-scan): To assess vitreous hemorrhage or retinal detachment, only if globe integrity is intact.
- X-ray: May identify fractures but is less sensitive than CT.
3. Acute Medical Management:
- Pain Management: Administer systemic analgesics for pain relief.
- Cycloplegics: Cyclopentolate drops to reduce ciliary spasm and photophobia.
- Topical Antibiotics: Prophylactic antibiotic eye drops or ointments to prevent infection.
- Steroids: Considered in non-perforating injuries to reduce inflammation and swelling (under specialist guidance).
- Elevate Head: Helps reduce intraocular pressure and manage hyphema.
4. Specialized Interventions:
- Hyphema Management: Treat with bed rest, head elevation, and monitoring of intraocular pressure. Avoid NSAIDs (e.g., aspirin) as they may worsen bleeding.
- Surgical Repair: Required for globe rupture, retinal detachment, or severe orbital fractures.
- Orbital Decompression: Necessary for severe orbital fractures causing nerve or muscle entrapment.
- Secondary Procedures: Removal of vitreous hemorrhage or scar tissue in delayed presentations
Complications of Blunt Trauma to the Eye
Blunt eye trauma can lead to acute and long-term complications, including:
- Vision Loss: Temporary or permanent, depending on the severity of injury.
- Glaucoma: Traumatic glaucoma due to elevated intraocular pressure.
- Retinal Detachment: A sight-threatening complication requiring surgical repair.
- Post-Traumatic Cataract: Opacification of the lens following trauma.
- Sympathetic Ophthalmia: A rare autoimmune reaction affecting the uninjured eye.
- Scarring or Deformities: Visible scars or orbital deformities impacting function and appearance.
Prevention
- Protective Eyewear: Use safety goggles in high-risk environments such as sports, construction, or industrial work.
- Public Awareness: Educate on the importance of eye safety and early medical evaluation.
- Occupational Safety Measures: Follow workplace safety protocols to minimize the risk of injury.
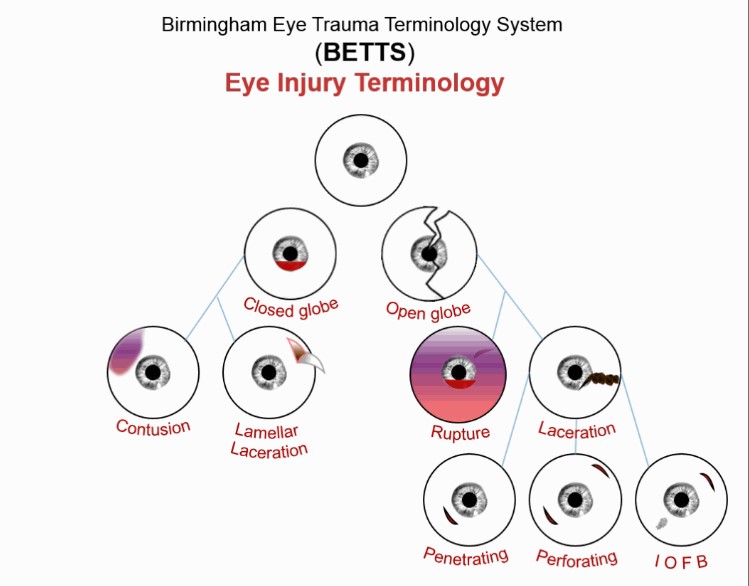
Classification of Eye Injuries Based on BETTS
The Birmingham Eye Trauma Terminology System (BETTS) provides a systematic approach for classifying ocular trauma. It categorizes injuries based on whether the globe remains intact (closed globe) or is compromised (open globe).
Closed Globe Injuries
In closed globe injuries, the outer layers of the eye (cornea and sclera) remain intact, and the injury is confined within the eye.
A. Contusion: Caused by blunt trauma that compresses and damages ocular tissues without causing an open wound.
Features:
- Hyphema: Blood in the anterior chamber.
- Vitreous Hemorrhage: Bleeding into the vitreous humor.
- Choroidal Rupture: Break in the choroid, visible on fundus examination.
- Retinal Edema or Detachment: May result from force transmitted through the eye.
Examples: Punch to the eye, sports injuries (e.g., impact from a ball).
B. Lamellar Laceration: A partial-thickness wound where the outer layers of the cornea or sclera are disrupted but do not penetrate fully.
Features:
- No communication between the external environment and the interior of the eye.
- Symptoms include pain, tearing, and light sensitivity.
Causes: Sharp objects that lightly scrape the eye without full penetration.
Open Globe Injuries
Open globe injuries involve a full-thickness wound of the cornea or sclera, leading to exposure of intraocular structures.
A. Rupture: Caused by a blunt force that increases intraocular pressure, resulting in a burst injury at the weakest point of the globe.
Features:
- Irregular globe shape due to prolapse of internal tissues.
- Severe vision loss or no light perception.
Causes: Direct blows to the eye or accidents causing sudden, severe impact.
B. Laceration: A full-thickness wound caused by a sharp object cutting through the eye wall.
Subcategories:
1. Penetrating Injury:
- A single-entry wound caused by a sharp object.
- Example: Injury from a nail, knife, or pencil.
2. Perforating Injury:
- Two wounds: an entry and an exit wound.
- Example: Gunshot or sharp object passing entirely through the globe.
3. IOFB (Intraocular Foreign Body):
- A foreign object enters the eye and remains lodged inside.
- Examples: Metal shards, glass, or wood splinters.
- Complications include infection (endophthalmitis) or chronic inflammation.
Key Differences in BETTS Terminology
Type | Key Characteristics | Examples |
Closed Globe | Intact outer layers (no full-thickness wound). | Contusion, lamellar laceration. |
Open Globe | Full-thickness wound of cornea or sclera. | Rupture, laceration, IOFB. |
Contusion | Non-penetrating injury causing internal damage. | Hyphema, retinal detachment. |
Lamellar Laceration | Partial-thickness wound. | Sharp objects causing abrasion. |
Rupture | Burst injury due to increased intraocular pressure. | Blunt trauma from fist or object. |
Laceration | Full-thickness cut with intraocular involvement. | Penetrating, perforating injuries. |
IOFB | Retained foreign body inside the eye. | Metallic or glass fragments. |
Injury by Ocular Structures
Structure | Injuries |
Cornea | – Simple abrasions or epithelial damage. – Recurrent erosions. – Corneal opacity from trauma or edema. |
Sclera | – Partial or full-thickness lacerations. – Associated with globe rupture in severe cases. |
Anterior Chamber | – Hyphema (blood in the chamber). – Exudates from traumatic uveitis. |
Iris and Pupil | – Traumatic miosis (pupil constriction). – Traumatic mydriasis (dilated, non-responsive pupil). – Iridodialysis (detachment of the iris root). – Aniridia (complete loss of the iris). |
Lens | – Vossius ring: Pigment deposit on the lens capsule. – Concussion cataracts. – Lens dislocation. |
Retina and Vitreous | – Commotio retinae (retinal whitening). – Retinal tears or detachment. – Vitreous hemorrhage. |
Choroid | – Rupture seen as crescent-shaped whitish areas on fundus examination. – Choroidal hemorrhage or detachment. |
General Nursing Interventions for Patients with Eye Trauma
1. Assess Visual Acuity
- Intervention: Perform baseline and ongoing visual acuity testing using a Snellen chart or equivalent.
- Rationale: Establishes the degree of visual impairment and helps monitor progression or recovery of vision.
2. Inspect the Eye for Injuries
- Intervention: Examine the eye for lacerations, swelling, foreign bodies, or other visible abnormalities.
- Rationale: Identifies the type and extent of injury, guiding appropriate care and treatment.
3. Apply Sterile Eye Dressing
- Intervention: Cover the affected eye with a sterile eye patch or dressing if indicated.
- Rationale: Protects the injured eye from further trauma, infection, or environmental irritants.
4. Maintain Head Elevation
- Intervention: Position the patient with the head elevated at 30–45 degrees.
- Rationale: Reduces intraocular pressure, minimizes edema, and assists in the management of hyphema or swelling.
5. Administer Prescribed Medications
- Intervention: Administer antibiotics, cycloplegics, or anti-inflammatory eye drops as prescribed.
- Rationale: Prevents infection, reduces pain, and controls inflammation to promote healing.
6. Avoid Eye Rubbing
- Intervention: Educate the patient to avoid touching or rubbing the injured eye.
- Rationale: Prevents further damage, infection, or aggravation of the injury.
7. Assess for Pain
- Intervention: Monitor the patient’s pain level and administer analgesics as prescribed.
- Rationale: Pain relief enhances comfort and compliance with treatment, facilitating recovery.
8. Use Cold Compresses for Swelling
- Intervention: Apply a cold compress to the affected area if there is swelling (avoid direct pressure on the globe).
- Rationale: Reduces inflammation and bruising in cases of blunt trauma.
9. Monitor for Signs of Infection
- Intervention: Observe for redness, warmth, purulent discharge, or worsening pain.
- Rationale: Early detection of infection allows for timely intervention to prevent complications.
10. Provide Emotional Support
- Intervention: Reassure the patient and provide emotional support throughout treatment.
- Rationale: Helps reduce anxiety and promotes trust, improving the patient’s cooperation and recovery.
11. Educate on Proper Medication Use
- Intervention: Teach the patient how to administer eye drops or ointments correctly.
- Rationale: Ensures effective use of medications and reduces the risk of further injury or contamination
12. Monitor for Vision Changes
- Intervention: Frequently assess the patient for any new or worsening visual symptoms.
- Rationale: Detects complications such as retinal detachment, glaucoma, or optic nerve damage early.
13. Protect the Unaffected Eye
- Intervention: Advise the patient to limit activities that may strain the uninjured eye.
- Rationale: Prevents sympathetic ophthalmia, a rare condition where the unaffected eye becomes inflamed.
14. Facilitate Diagnostic Testing
- Intervention: Prepare the patient for imaging (e.g., CT scan, ultrasound) as ordered.
- Rationale: Provides detailed information about the injury, aiding in accurate diagnosis and treatment planning.
15. Prepare for Surgical Intervention
- Intervention: If surgery is required, educate and prepare the patient for the procedure.
- Rationale: Ensures the patient is informed and reduces preoperative anxiety, improving surgical outcomes.


Thanks brother kutiddeee olimusomesa