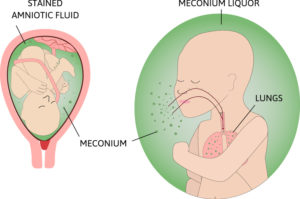
Meconium aspiration syndrome is troubled breathing (respiratory distress) in a newborn who has breathed (aspirated) a dark green, sterile fecal material called meconium into the lungs before or around the time of birth
- Meconium is the earliest stool of a newborn. Occasionally, newborns pass meconium during labor or delivery, resulting in a meconium-stained amniotic fluid (MSAF). Meconium is the first intestinal discharge from newborns, a viscous, dark-green substance composed of intestinal epithelial cells, lanugo, mucus, and intestinal secretions (eg, bile.
- Meconium aspiration syndrome (MAS) is the inhalation of stained amniotic fluid, which can occur before, during, or immediately after birth.
Table of Contents
ToggleCauses of Meconium Aspiration Syndrome
- Placental insufficiency. When a mother has placental insufficiency, there is a lack of adequate blood flow to the baby, which can cause fetal distress, leading to the untimely passage of meconium.
- Preeclampsia. When the placenta does not carry adequate oxygen and nutrition for the fetus due to maternal underperfusion such as preeclampsia, the placental villi show increased syncytial knots, villous agglutination, intervillous fibrin, and distal villous hypoplasia, while maternal vessels in the deciduadisclose atherosis or mural hypertrophy of the arterioles.
- Maternal infection/chorioamnionitis. When the placental membranes are ruptured and amniotic fluid infection occurs, the placenta shows acute chorioamnionitis (as the maternal inflammatory response) and funisitis (as the fetal inflammatory response).
- Fetal hypoxia. Fetal hypoxia leads to passage of meconium from neural stimulation of a maturing gastrointestinal system.
Clinical Features
- Severe respiratory distress. Severe respiratory distress may be present; symptoms include cyanosis, end-expiratory grunting, nasal flaring, intercostal retractions, tachypnea, barrel chest due to the presence of air trapping, and in some cases, auscultated rales and rhonchi.
- Staining of the fingernails. Yellow-green staining of fingernails, umbilical cord, and skin may be also observed.
- Green urine. Green urine may be noted in newborns with MAS less than 24 hours after birth; meconium pigments can be absorbed by the lung and can be excreted in urine.
- Meconium or dark green stains in the amniotic fluid
- Tachypnea
- Nasal flaring
- Retractions
- Cyanosis or desaturation
- Rales
- Rhonchi
- Greenish yellow staining of the umbilical cord, nail beds, or skin. Meconium staining may be visible in the oropharynx and (on intubation) in the larynx and trachea.
- Neonates with air trapping may have a barrel-shaped chest
- Fetal distress
- Signs of neonatal asphyxia
Pathophysiology
In utero, meconium passage results from neural stimulation of a maturing gastrointestinal (GI) tract, usually due to fetal hypoxic stress.
- As the fetus approaches term, the GI tract matures, and vagal stimulation from the head or spinal cord compression may cause peristalsis and relaxation of the rectal sphincter, leading to meconium passage.
- Meconium directly alters the amniotic fluid, reducing antibacterial activity and subsequently increasing the risk of perinatal bacterial infection.
- In addition, meconium is irritating to fetal skin, thus increasing the incidence of erythema toxicum(common rash seen in full-term newborns)
- However, the most severe complication of meconium passage in utero is perinatal aspiration of stained amniotic fluid (before, during, or immediately after birth)—ie, meconium aspiration syndrome (MAS).
- Aspiration of meconium-stained amniotic fluid may occur if the fetus is in distress, leading to a gasping breathing pattern.
- This aspiration induces hypoxia via four major pulmonary effects: airway obstruction, surfactant dysfunction, chemical pneumonitis, and pulmonary hypertension.
Diagnosis
- Acid-base status. Measurement of arterial blood gas (ABG) pH, partial pressure of carbon dioxide (pCO2), and partial pressure of oxygen (pO2), as well as continuous monitoring of oxygenation by pulse oximetry, are necessary for appropriate management; the calculation of an oxygenation index (OI) can be helpful when considering advanced treatment modalities, such as extracorporeal membrane oxygenation (ECMO).
- Serum electrolytes. Obtain sodium, potassium, and calcium concentrations at 24 hours of life in infants with MAS, because syndrome of inappropriate secretion of antidiuretic hormone (SIADH) and acute renal failure are frequent complications of perinatal stress.
- Complete blood cell count. Hemoglobin and hematocrit levels must be sufficient to ensure adequate oxygen-carrying capacity; thrombocytopenia increases the risk for neonatal hemorrhage; neutropenia or neutrophilia with left shift of the differential may indicate perinatal bacterial infection.
- Chest radiography. Chest radiography is essential in order to confirm the diagnosis of meconium aspiration syndrome (MAS) and determine the extent of the intrathoracic pathology; identify areas of atelectasis and air leak syndromes; ensure appropriate positioning of the endotracheal tube and umbilical catheters. Diagnosis is confirmed by chest x-ray showing hyperinflation with variable areas of atelectasis and flattening of the diaphragm
- Echocardiography. Echocardiography is necessary to ensure normal cardiac structure and for assessment of cardiac function, as well as to determine the severity of pulmonary hypertension and right-to-left shunting.
Meconium passage and Respiratory distress
Differential Diagnosis
- Aspiration Syndromes
- Congenital Heart Disease with Pulmonary Hypertension
- Pediatric Congenital Diaphragmatic Hernia
- Pediatric Idiopathic Pulmonary Artery Hypertension
- Pediatric Pneumonia
- Pediatric Sepsis
- Persistent Pulmonary Hypertension of the Newborn (PPHN)
- Surfactant Deficiency
- Transient Tachypnea of the Newborn
- Transposition of the Great Arteries
Management of Meconium Aspiration Syndrome
- Infants born with meconium aspiration syndrome should have routine neonatal care while monitoring for signs of distress according to the general neonatal resuscitation guidelines e.g. Suctioning to open up the airway
- Pediatrics no longer recommend routine endotracheal suctioning for non-vigorous infants with meconium aspiration syndrome, Chest tube insertion under water seal drainage to treat atelectasis and pneumothorax in vigorous infants.
- Newborns are admitted to the neonatal intensive care unit (NICU) if necessary.
- Oxygen therapy: Supplemental oxygen is often needed in meconium aspiration syndrome with goal oxygen saturation > 90% to prevent tissue hypoxia and improve oxygenation.
- Surfactant: The use of surfactant in meconium aspiration syndrome is not standard of care, however, as discussed above, surfactant inactivation has a role in the pathogenesis of meconium aspiration syndrome. Therefore surfactant may be helpful in some cases
- Cardiac exam. In patients with meconium aspiration syndrome (MAS), a thorough cardiac examination and echocardiography are necessary to evaluate for congenital heart disease and persistent pulmonary hypertension of the newborn (PPHN).
- Rooming-in. If the baby is vigorous (defined as having a normal respiratory effort and normal muscle tone), the baby may stay with the mother to receive the initial steps of newborn care; a bulb syringe can be used to gently clear secretions from the nose and mouth.
- Placing in a radiant warmer. If the baby is not vigorous (defined as having a depressed respiratory effort or poor muscle tone), place the baby on a radiant warmer, clear the secretions with a bulb syringe, and proceed with the normal steps of newborn resuscitation (ie, warming, repositioning the head, drying, and stimulating).
- Minimize handling. Minimal handling is essential because these infants are easily agitated; agitation can increase pulmonary hypertension and right-to-left shunting, leading to additional hypoxia and acidosis; sedation may be necessary to reduce agitation.
- Insertion of umbilical artery catheter. An umbilical artery catheter should be inserted to monitor blood pH and blood gases without agitating the infant.
- Respiratory care. Continue respiratory care includes oxygen therapy via hood or positive pressure, and it is crucial in maintaining adequate arterial oxygenation; mechanical ventilation is required by approximately 30% of infants with MAS; make concerted efforts to minimize the mean airway pressure and to use as short an inspiratory time as possible; oxygen saturation should be maintained at 90-95%.
- Surfactant therapy. Surfactant therapy is commonly used to replace displaced or inactivated surfactant and as a detergent to remove meconium; although surfactant use does not appear to affect mortality rates, it may reduce the severity of disease, progression to extracorporeal membrane oxygenation (ECMO) utilization, and decrease the length of hospital stay.
- IV fluids. Intravenous fluid therapy begins with adequate dextrose infusion to prevent hypoglycemia; intravenous fluids should be provided at mildly restricted rates (60-70 mL/kg/day).
- Diet. Progressively add electrolytes, protein, lipids, and vitamins to ensure adequate nutrition and to prevent deficiencies of essential amino acids and essential fatty acids.
- Antibiotics such as Ampicillin and Gentamicin to prevent or treat any infection
- Systemic vasoconstrictors. These agents are used to prevent right-to-left shunting by raising systemic pressure above pulmonary pressure; systemic vasoconstrictors include dopamine, dobutamine, and epinephrine; dopamine is the most commonly used.
- Pulmonary vasodilator. Inhaled nitric oxide is a pulmonary vasodilator that has a role in pulmonary hypertension and persistent pulmonary hypertension (PPHN)
- Neuromuscular blocking agents. These agents are used for skeletal muscle paralysis to maximize ventilation by improving oxygenation and ventilation; they are also used to reduce barotrauma and minimize oxygen consumption.
- Sedatives. These agents maximize the efficiency of mechanical ventilation, minimize oxygen consumption, and treat the discomfort of invasive therapies.

Nursing Diagnosis
- Hyperthermia related to inflammatory process/ hypermetabolic state as evidenced by an increase in body temperature, warm skin and tachycardia.
- Fluid volume deficit related to failure of regulatory mechanism.
- Ineffective tissue perfusion related to impaired transport of oxygen across alveolar and on capillary membrane.
- Interrupted breastfeeding related to neonate’s present illness as evidenced by separation of mother to infant.
- Risk for Impaired parent/neonates attachment related to neonates physical illness and hospitalization
Nursing Care Planning and Goals
- Patient will maintain normal core temperature as evidenced by vital signs within normal limits and normal WBC level.
- Patient will be able to maintain fluid volume at a functional level as evidenced by individually adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor and prompt capillary refill and resolution of edema.
- Patient will be able to maintain fluid volume at a functional level as evidenced by individually adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor and prompt capillary refill and resolution of edema.
- Patient will demonstrate increased perfusion as evidenced by warm and dry skin, strong peripheral pulses, normal vital signs, adequate urine output and absence of edema.
- The mother will identify and demonstrate techniques to sustain lactation until breastfeeding is initiated.
- The mother shall still be able to identify and demonstrate techniques to sustain lactation and identify techniques on how to provide the newborn with breast milk.
- The mother will identify and demonstrate techniques to enhance behavioral organization of the neonate
- After discharge, the parents will be able to have mutually satisfying interactions with their newborn.
Nursing Intervention
- Reduce body temperature. Provide TSB to help lower down the temperature; ensure that all equipment used for the infant is sterile, scrupulously clean; do not share equipment with other infants to prevent the spread of pathogens, and administer antipyretics as ordered.
- Improve fluid volume level. Monitor and record vital signs to note for alterations; provide oral care by moistening lips & skin care by providing daily bath; administer IV fluid replacement as ordered to replace fluid losses.
- Increase tissue perfusion. Note quality and strength of peripheral pulses; assess respiratory rate, depth, and quality; assess skin for changes in color, temperature, and moisture; elevate affected extremities with edema once in a while to lower oxygen demand.
- Improve frequency of breastfeeding. Demonstrate the use of manual piston-type breast pump.; review techniques for storage/use of expressed breast milk; provide privacy, calm surroundings when the mother breastfeeds; recommend for infant sucking on a regular basis, and encourage the mother to obtain adequate rest, maintain fluid and nutritional intake, and schedule breast pumping every 3 hours while awake.
- Improve infant-parent relationship. Educate parents regarding child growth and development, addressing parental perceptions; involve parents in activities with the newborn that they can accomplish successfully, and recognize and provide positive feedback for nurturing and protective parenting behaviors.
Evaluation
Goals are met as evidenced by:
- Patient maintained normal core temperature as evidenced by vital signs within normal limits and normal WBC level.
- Patient was able to maintain fluid volume at a functional level as evidenced by individually adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor and prompt capillary refill and resolution of edema.
- Patient was able to maintain fluid volume at a functional level as evidenced by individually adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor and prompt capillary refill and resolution of edema.
- Patient demonstrated increased perfusion as evidenced by warm and dry skin, strong peripheral pulses, normal vital signs, adequate urine output and absence of edema.
- The mother identified and demonstrated techniques to sustain lactation until breastfeeding is initiated.
- The mother was able to identify and demonstrate techniques to sustain lactation and identify techniques on how to provide the newborn with breast milk.
- The mother identified and demonstrated techniques to enhance behavioral organization of the neonate
- After discharge, the parents were able to have a mutually satisfying interaction with their newborn.
Complications
- Persistent pulmonary hypertension
- Pneumothorax
- Aspiration pneumonia
- Brain damage due to lack of oxygen
- Breathing difficulty that lasting for several days
- Atelectasis (Collapsed lung)